SCLERODERMA DR MAGDI AWAD SASI 2016 LMB
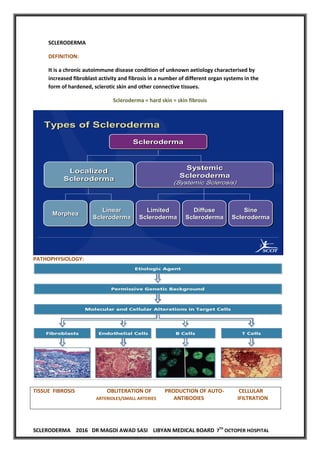
- 1. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL SCLERODERMA DEFINITION: It is a chronic autoimmune disease condition of unknown aetiology characterised by increased fibroblast activity and fibrosis in a number of different organ systems in the form of hardened, sclerotic skin and other connective tissues. Scleroderma = hard skin = skin fibrosis 2 Types of Scleroderma Scleroderma Localized Scleroderma Systemic Scleroderma (Systemic Sclerosis) Morphea Linear Scleroderma Limited Scleroderma Diffuse Scleroderma Sine Scleroderma PATHOPHYSIOLOGY: TISSUE FIBROSIS OBLITERATION OF PRODUCTION OF AUTO- CELLULAR ARTERIOLES/SMALL ARTERIES ANTIBODIES IFILTRATION
- 2. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL PREVALENCE: Incidence in US of 9-19 cases per million per year Prevalence in US of ~286 cases per million 250 patients / million / in USA New cases 20 /million /year SEX: Female to male ---- 4 to 5 times in female AGE: Average at time of diagnosis 50 years The prevalence and manifestation of scleroderma vary among racial and ethinic groups! ex; scleroderma is 100 times more common among the choctan native Americans in Oklahoma ; the disease is characterized by diffuse skin disease and pulmonary fibrosis. Milder limited disease is more common among white women and African American are more likely to have sever disease. The disease expression is influenced by: 1. Ethinic and racial groups 2. Family clustering 3. Specific autoantibodies with specific HLA 4. Environmental factors CLINICAL FEATURES: The most frequent symptoms (( in descending order )) are: A. Raynauds phenomena B. Gastro-esophageal reflux C. Swollen fingers D. Musculoskeletal pain /Arthralgias You have to be aware of scleroderma ;WHY? Because early intervention can reduce morbidity and prevent life threatening complications. The diagnostic criteria for scleroderma : 1. Thickened skin changes proximal to MCP joints. OR 2. Two of the following: i. Sclerodactaly ii. Digital pitting ---loss of tissue on finger pads iii. Bibasilar pulmonary fibrosis
- 3. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL The diagnosis of limited scleroderma can be made if the patient has 3/5 of CREST: 1. Calcinosis 2. Raynaud phenomena 3. Esophageal dysmotility 4. Sclerodactly 5. telangiectasia Early presentation of scleroderma:- A. musculoskeletal discomfort B. fatigue C. weight loss D. heart burn due to GERD when the symptoms are accompanied by raynauds or new onset of cold sensitivity ,scleroderma is more likely. Classical presentation: There are three patterns of disease: A.LIMITED CUTANEOUS SYSTEMIC SCLEROSIS : ----- Long H/O Raynauds phenomena ---Raynaud's may be first sign Scleroderma affects face and distal limbs predominately Swelling or skin thickening of the fingers. Gastroesophageal reflux and dysphagia. Systemic --- weight loss ,dyspnea ,arthralgia Associated with anti-centromere antibodies CREST syndrome is an older term for the limited cutaneous form. CREST syndrome is a subtype of limited cutaneous systemic sclerosis: Calcinosis, Raynaud's phenomenon, Esophageal dysmotility, Sclerodactyly, Telangiectasia Complications of CREST syndrome: Malabsorption can develop in these patients secondary to bacterial overgrowth of the sclerosed small intestine (dysmotility secondary to infiltration of the intestinal wall with fibrous tissue). Also, unfortunately pulmonary hypertension is one of the more common late complications seen in such patients. EX: Female pt. with SOB, lung fibrosis, GERD, Raynaud’s, +ve ANA >> Systemic sclerosis as CREST develop pulmonary HTN NOT ILF.
- 4. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL B.DIFFUSE CUTANEOUS SYSTEMIC SCLEROSIS ------ New onset of Raynauds phenomena Rapid change of skin texture and edema ,pain ,pruritis Significant systemic symptoms with arthralgia ,weight loss ,tendon friction rubs Internal organ involvement –lung ((dyspnea)) ,Kidney ((HTN)) , GIT ((malabsorption)). Scleroderma affects trunk and proximal limbs predominately ((ALL THE BODY)). Associated with scl-70 antibodies Poor prognosis Whilst diffuse systemic sclerosis is associated with more severe and rapid internal organ involvement ,it is also seen in the limited form. C. Morphea (Localized Scleroderma) (without internal organ involvement) Tightening and fibrosis of skin. May manifest as plaques (morphoea) or linear. This is a well-defined oval to round plaque. (Like a painless lesion to his left subcostal region, dry, indurated and slightly coarse to palpation). The pathogenesis is poorly defined. An autoimmune component is suggested by enhanced T helper 2 (Th2) dependent interleukin 4 (IL-4) activity, which in turn up regulates transforming growth factor beta (TGF -beta). TGF-beta stimulates fibroblast production of collagen and other extracellular matrix proteins. SYMPTOMS AND SIGNS: A. SKIN: The skin is one of the most universally and prominently involved organs in both diffuse and limited cutaneous disease. Initially may manifest as diffuse swelling, especially in the hands and fingers. This is followed by progressive skin tightening from excess collagen deposition. A notable difference in diffuse vs limited disease (and one that largely defines the different subsets) is that the skin changes in limited disease are confined to areas below the elbows and knees. Skin involvement in diffuse disease is more widespread, involving the entire arm and/or leg as well as skin on the trunk. Be aware that the skin on the face is typically involved in both disease subsets. Other skin findings may include hard calcium deposits under the skin, known as calcinosis cutis (seen more often in limited cutaneous systemic sclerosis). Small, spider-like, visible, dilated blood vessels called telangiectasias can be seen (often on the face and chest). Skin ulcers and pigment changes are not uncommon.
- 5. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL a. Thickening of the skin: - Most easily recognizable manifestation - Not prominent in all patients - Scleroderma classified according to the amount and location of involvement. Patient with limited disease:--- Skin changes on the face and distal to knees and elbows ex; CREST 1. Typically only involves the skin of fingers distal to the MCPJ –Sclerodactly. 2. Marked Telengectasias ((dilatated capillaries ))that occur on the skin of face ,the palmer surface of the hands and the mucous membranes. 3. Subcutaneous calcinosis ---fingers ,extensor surface of forearm. Patient with diffuse disease---- Patient with proximal extremity or truncal skin involvement The amount of skin thickening can be quantified by skin score . The skin is pinched between the examiners thumbs in 17 specified areas of the patients body . 0 (( Normal )) --- ------------ 3 (( Very thick)) Higher skin scores correlates with greater degree of internal organ involvement. The early stage----- inflammatory face: Skin edematous and inflamed Skin erythema Pigmentary changes ---hyperpigmented areas with depigemntation—salt&pepper appearance. Pruritis and discomfort Lasts weeks –months Fibroblasts ---over produce extracellular matrix that leads to increased collagen deposition in the skin leading to collagen cross linking –skin tighting The later stages---- Skin become thickening , dry ,scaly because of the loss of its natural oily due to sebaceous gland damage. Dry skin are intensly pruritic causing excoriation.
- 6. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL B. Vascular disease: A diffuse vasculopathy of peripheral arteries is manifested by : 1. Intimal proliferation 2. Activation of arterial smooth muscles. 3. Narrowing of the vessel lumen. Critical ischemia occurs in the tissues when vasoconstriction occlude these vessels. Evidence suggested that this vascular disease is fundamental to organ damage. Heart----------CMP Lung -----------PHTN Kidney --------- scleroderma renal crisis ((SRC)) Table 1: ACR/EULAR Revised Systemic Sclerosis Classification Criteria Item Sub-item(s) Score Skin thickening of the fingers of both hands extending proximally to the metacarpophalangeal joints (presence of this criterion is sufficient criterion for SSc classification) None 9 Skin thickening of the fingers (count the higher score only) Puffy fingers 2 Sclerodactyly (distal to the metacarpophalangeal joints but proximal to the proximal interphalangeal joints) 4 Fingertip lesions (count the higher score only) Digital tip ulcers 2 Fingertip pitting scars 3 Telangiectasia None 2 Abnormal nailfold capillaries None 2 Pulmonary arterial hypertension and/or interstitial lung disease (maximum score is 2) Pulmonary arterial hypertension 2 Interstitial lung disease 2 Raynaud phenomenon None 3 Systemic sclerosis–related autoantibodies (maximum score is 3) Anticentromere 3 Anti–topoisomerase I 3 Anti–RNA polymerase III 3 The total score is determined by adding the maximum score in each category. Patients with a total score equal to or greater than 9 are classified as having definite systemic sclerosis (modified from van den Hoogen F, Khanna D, Fransen J, et al. 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative.
- 7. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL C/F--- A) Raynauds phenomenon: Is the first manifestation of the disease in almost every patient. RP is an episodic self limited and reversible vasomotor disturbance manifested as a color changes bilaterally in the fingers ,toes sometimes ears ,nose and lips. The color changes are pallor ,cyanosis and then erythema((white ,blue ,then red)). There is triad of colours: initial whitening of the fingers resulting from vasospasm, followed by blue discolouration and then reddening and pain. Raynaud's phenomena may be: Primary (Raynaud's disease) or Secondary (Raynaud's phenomenon) Raynaud's disease typically presents in young women (e.g. 30 years old) with symmetrical attacks. There is no need for the three color for diagnosis. Episodic pallor or cyanosis that reverses to erythema or normal skin color may be all that is seen. Patient may describe symptoms of numbness ;tingling or pain on recovery. Stress and cold temperature induce an exaggerated vasoconstriction of the small arteries ,arterioles and AV shunts of the skin of the digits. This is manifested clinically as PALLOR & CYANOSIS of the digits followed by reactive hyperemia after rewarming. The attacks are often painful and lead to digital ulceration ,gangrene or amputation. In patient with Raynauds phenomena ,to suggest early SS: a) Positive ANA ,Antitopoisomerase ( SCL 70) ,Anticentromer AB b) Nail fold capillary abnormality c) GERD d) Puffy swollen fingers or legs e) Tendon friction rubs Raynauds phenomena occur in limited and diffuse scleroderma. If RP precedes skin changes by a year === LIMITED If RP occur simultaneously with skin changes ==DIFFUSE For treatment; i. Calcium channel blocker---Nifedipine ,Diltiazem ii. Antiadrenergic agents ----Prazosin ,Methyldopa iii. ACE-I ,AGB II iv. Aspirin ,Niacin NOTE: Patient > 30 years in whom RP develops should be screened with an ANA test and nail fold examination if they have sever painful episodes and signs of digital ischemia. Patient with scleroderma almost always have positive ANA.
- 8. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL A negative ANA makes diagnosis of scleroderma unlikely. HOW TO DIFFERENTIATE BETWEEN PRIMARY AND SECONDARY RAYNAUDS PHENOMENA? For primary , - Symmetrical episodes ,intermittent attacks. - Affecting both hands, but not necessarily all fingers - No evidence of peripheral vascular disease - No evidence of tissue gangrene/digital pitting/ulceration/severe ischaemia - No suspicion of underlying disease - Normal nail-fold capillary microscopy - Negative ANA with normal ESR For secondary, - Male sex - Onset > 40 years - Unilateral symptoms - Asymmetry of digits affected - Painful attacks - Digital ulcers - Tissue ischemia-- gangrene or severe ischaemia of one or more digits. - Very rarely: chilblains (pernio) are itchy, painful purple swellings which occur on the fingers and toes after exposure to the cold. - Symptoms and signs of CTD - Rashes Features which may suggest RA or SLE, e.g. arthritis or recurrent miscarriages ,calcinosis - Presence of autoantibodies--- Positive ANA The most useful initial assessment to determine whether the Raynaud’s is related to vasculitis or not >>>(( must include nail fold capillary loop examination, ideally by capillaroscopy or, if not available, by ophthalmoscopy using magnification ))>>> In CTD such as systemic sclerosis: dilated, distorted, missed nail fold capillary loops. Secondary causes: 1) Connective tissue diseases (CTD): scleroderma (most common), RA, SLE, PAN, Sjogren’s syndrome. 2) Type I cryoglobulinaemia, cold agglutinins. 3) Leukaemia , Polycythaemia , Thrombangitis obliterans (Buerger’s disease) 4) Use of vibrating tools , Drugs: oral contraceptive pill, ergot (NB: Ergotamine is associated with Raynaud's phenomenon), βB, Vinblastine, Bleomycin. 5) Cervical rib.
- 9. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL Differential diagnosis of Raynaud's phenomenon includes: A. Chilblains (perniosis): erythematous itchy swellings on fingers and toes in response to cold. B. Acrocyanosis: continuous blueness of the extremities aggravated by cold. C. Erythromelalgia: painful erythema caused by paroxysmal dilatation of blood vessels. D. Vascular embolism. E. Livedo reticularis. F. Mottled, cyanotic discolouration of skin. B) Lung involvement: 2 forms pulmonary HTN and inflammatory alveolitis –ILF ILF PULMONARY HTN Limited SS Bibasilar and non progressive ((20%)) (( 8----28%)) Poor prognosis Diffuse SS More common and progressive ((30-60%)) Very rare Over lap Common and can progress (( 85%)) 21----30% 1. INTERSTITIAL LUNG DISEASE: Many patient are asymptomatic Clinical symptoms can be insidious and include exertional dyspnea ,easy fatigability and exertional dry cough. Later ,it may progress to dyspnea at rest. Clinical signs are typically early inspiratory fine crackles. PFT or HR CT scanning can detect very mild and early disease. Routine PFT is mandatory because early intervention may prevent progression. 80% of patients have restrictive ventilator defects on PFT Only 10—20% suffer from progressive ILD. Treatment: Patient with disease restricted to bases ----no treatment Patient with progressive disease ---treatment with progression to middle &upper lobes. Patient who respond to immunosuppressive have active alveolitis a. Bronchoalveolar lavage ---- Neutrophils / Eosinophils > 5% b. HR CT scan ---nonspecific interstitial pneumonitis ---ground glass c. Lung biopsy These patients may respond to prednisolone and cyclophosphamide. Patients with progressive lung disease without alveolitis /UIP-usual interstitial pneumonitis on HRCT scan /Lung biopsy do not respond to treatment.
- 10. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL WHY? Because fibrosis due to fibroblastic foci. Treatment ---- antifibrotic therapy , alpha interferon 2. Pulmonary HTN: Risk Factors for PAH in Scleroderma— 1) Long disease duration (usually >8 yr) 2) Limited scleroderma > diffuse scleroderma 3) Abnormal pulmonary function tests a. low DLCO <55% predicted and FVC %/DLCO % >1.6 4) Autoantibody profile a. anticentromere antibody b. antinucleolar pattern on ANA (anti-U3 antibody, which is not clinically available) Due to pulmonary vascular disease. Patient usually have an insidious onset of exertional dyspnea which can become at rest with fatigue and loss of effort. Physical exam ; loud P2 ,S3 RV ,TR ,PULMONARY REGURGITATION Raised JVP ,pedal edema Isolated pulmonary HTN occurs more commonly in limited SCL which have long duration of disease. Pulmonary HTN complicates the course in 10% CREST. Treatment : Initially ;patients are placed on nasal O2. Ca channel blocker can be tried. Full anticoagulation is often administered. For sever pulmonary HTN , A. Continous I.V. epoprostenol ((PGI2)) B. Oral non specific endothelin antagonist ((bosentan))125mgBID It is Contraindicated in: 1. Pregnancy 2. Cyclosporine 3. Glyburide 4. Hepatotoxic C. Lung transplantation D. Silendafil C) GIT: Both upper and lower GIT are involved. Highly variable in its clinical expression. It can be asymptomatic ((mild constipation)) or profound dysfunction((malnutrition)). The gastrointestinal tract is involved in almost all cases of systemic sclerosis. Fibrotic and vascular changes all along the GI tract interfere with normal motility, resulting in a host of problems including gastroesophageal reflux disease (GERD), intestinal dilatation with abdominal pain, bacterial overgrowth with diarrhea, and malabsorption. An increasingly recognized problem in both diffuse and limited cutaneous forms of disease is gastric antral vascular ectasia (GAVE). Analagous to dilated blood vessels seen on the skin, blood
- 11. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL vessels in the stomach can dilate and then rupture, with the potential for massive blood loss. This photo shows the appearance of the dilated blood vessels on endoscopy. 1. GERD: The majority are symptomatic with dysphagia. The patient is complaining of sensation of the food getting stuck in the mid esophagus ,atypical chest pain ,or cough. The patient often complain that they must drink liquids to swallow solid food ,meat or bread. Reflux and dysphagia occur because of dysmotility of esophagus and stomach ((gastroparesis)). This type of organ dysfunction results from atrophy of the esophageal smooth muscle. Complication: 1. Esophagitis 2. Esophageal ulceration with bleeding 3. Esophageal stricture 4. Barret esophagus 5. Candidiasis GIT dysfunction is due to: 1. There is neural dysfunction thought to be due to arteriolar changes of vasa nervourum leading to dysmotility. 2. Smooth muscle atrophy
- 12. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL Esophagealdysmotility is assesd by: Manometry Cine –esophagography Endoscopy Barium swallow WHAT IS WATER-MELON STOMACH? Gastric antral venous ectasia It causes upper GIT bleeding in SS. Treatment: patient should not eat for 2—3 hours before bed time The head of the bed should be elevated 4 inche. Decrease the acidity of stomach by antacids. Proton pump inhibitors can be used ---Esmoprazole ,Lansoprazole Motility agents ((metoclopramide))before meals are helpful early in the diagnosis. Bowel involvement Diminished peristalsis with stasis and dilatation Bacterial over growth –H breathtest ,High folate Malabsorption Low albumin Low fat content Low B6/B12/folate/ vitD Low D xylose absorption test Low carotene Patient may complain of abdominal distention ,obstructive symptoms ,diarrhea ,vitamin deficiencies. Patient with large bowel involvement ---wide mouth diverticular on barium enema. Barium enema is contraindicated in patient with scleroderma. Treatment: Stimulation of gut motility ---metoclopramide ,erythromycin ,motilin agonist ,daily injection octreotide 50microgm /6hr S/C ,fibers. Diarrhea --bacterial overgrowth --metoclopramide ,tetracycline ,ciprofloxacin-10/d Avoid loperamide ,paregoric Smooth muscle atrophy of the bowel wall Affect small and large intestine Abnormal motility of the gut
- 13. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL Symptoms ---- Combination of constipation and diarrhea Recurrent bouts of pseudo-obstruction Bowel distention with leakage of air into the intestine— pneumatosis coli intestinalis Bowel rupture Lower bowel dys-motility can lead to bacterial overgrowth, diarrhea ,mal-absorption. D) CVS: Symptomatic cardiac disease is relatively rare. The lining around the heart may become inflamed, a condition called pericarditis. Fluid can build up around the heart (pericardial effusion) – the presence of this fluid may herald scleroderma renal crisis. The heart muscle itself may be affected causing a cardiomyopathy and the conduction system that carries electrical signals through the heart may become damaged. Usually subclinical Cardiopulmonary morbidity Ischemia ----reperfusion secondary to small arterial disease of myocardium leads to necrosis and tissue fibrosis. This leads to: 1. Cardiomyopathy 2. Arrhythmia 3. Heart failure 4. Pericarditis 5. Pericardial effusion Pericardial effusion— Detected by ECHO Large PE associated with poor prognosis It is usually clinically silent. E) RENAL: occurs almost exclusively in patients with diffuse cutaneous systemic sclerosis. It is characterized by HTN, anemia secondary to destruction of RBC (hemolytic anemia), and evidence of kidney damage (PROTEINURIA and HIGH creatinine). Patients at greatest risk for SRC include : 1. Rapid progression of skin involvement 2. Positive for anti-RNA polymerase III antibodies 3. Who have taken moderate or high doses of steroids in the preceding weeks or months. This complication is usually seen within the first 4 years of disease onset. It is almost universally fatal if not treated early and aggressively. The treatment is ACEI Clinically important kidney disease occur in minority of patients. SCR develops in 10% of patients. SCR occurs early in the course of diffuse scleroderma 2—3 years of onset ,more often in the fall and winter months.
- 14. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL SYMPTOMS:-- Symptoms are HEADACHE ,VISUAL CHANGES AND SEIZURES. The clinical presentation is typically with the symptoms of malignant hypertension: Headaches, Hypertensive retinopathy associated with visual disturbances, Seizures, Heart failure and pulmonary oedema. Renal failure may present as acute renal crisis , after prolonged HTN ,less commonly as normotensive renal failure. SCR is the abrupt onset of HTN ,appearance of flame shaped haemorrhage ,cotton wall exudates , grade III/IV retinopathy –papillodema and rapid deterioration of renal function over a month. The hypertension is almost always severe with a diastolic BP over 100 mmHg in 90% of patients. There is hypertensive retinopathy in about 85% of patients with exudates and haemorrhages and if severe, papilledema. If malignant HTN left untreated ,it can lead to renal failure Some are asymptomatic and normotensive with aprupt rise of creatinine. There may also be microangiopathic haemolytic anaemia (↓ Hb with blood film shows schistocytes and helmet cells), thrombocytopenia and raised renin levels. Renal function is impaired and usually deteriorates. TREATMENT: Scleroderma renal crisis is a medical emergency. Aggressive treatment is required to prevent the occurrence of irreversible vascular injury. ACE-I is the treatment of choice First line treatment is a gradual reduction in blood pressure (10-15 mmHg per day) with an oral ACEIs until the diastolic pressure reaches 85-90 mmHg. Upto to 400mg doses can be given to control BP. ACEI will improve hypertension and slow further renal impairment. This approach leads to a response in 90% of patients by reversing the angiotensin II mediated vasoconstriction. An abrupt fall in BP should be avoided as it can further diminish renal perfusion and increase the risk of ATN. Therefore, parenteral antihypertensive agents (for example, IV nitroprusside or IV labetalol) should be avoided. CCBs, usually nifedipine, may be added where there is inadequate reduction of BP with ACEI alone. Additional oral hypotensive agents (for example, labetalol) can be used if required, and if pulmonary oedema is present a nitrate infusion may be indicated. High dose of steroids increased the risk of renal failure in SS. There is anecdotal evidence that IV prostacyclin helps the microvascular lesion without precipitating hypotension, and this is used in some UK centres. LABRATORY ----- Renal crisis is linked with a positive ANA speckled pattern, anti-RNA polymerase I and II antibodies and absence of anti-centromere antibodies.
- 15. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL Increased RFT & RENIN ,microangiopathic hemolysis ,low platelets . Renal biopsy is not necessary in patients presenting with classical features of renal crisis Renal biopsy specimen –intestinal hyperplasia ,vasospasm of cortical arteries. F) MUSCULOSKELETAL INVOLVEMENT: Signs and symptoms related to involvement of the musculoskeletal system are found in systemic sclerosis. Many patients have joint and/or muscle pain. In diffuse cutaneous systemic sclerosis, tendon inflammation can result in an audible sound upon movement of involved structures (most commonly the fingers and wrists) known as a tendon friction rub. This finding is a marker of aggressive disease and puts patients at higher risk of serious organ involvement. Resorption of the most distal aspects of bones is a result of severe ischemia-osteolysis. Mild arthralgia Non erosive arthritis with synovitis Morning stiffness Deep tissue fibrosis ((tendon sheaths inflamed)) Areas around the tendons Active and passive range of joints motions are limited &painful Tendon friction rub over the wrists ,ankles and knees. DSS patients develop tendon friction rubs. Hand deformities and ankylosis are seen Bone ---resorption of bone---acrosclerosis and osteolysis Resoprption of ribs ,mandible ,radius ,ulna. G) MUSCLE: 1. Mild proximal weakness---fiber 2 myopathy 2. Mild elevation of muscle enzymes with waxing & waning of symptoms 3. Inflammatory type of myopathy with CPK increased(( overlap))—polymyositis. INVESTIGATION: Let’s look at a typical case of someone presenting with fairly early systemic sclerosis. The patient would statistically more likely be a female between the ages of 30-50 years old. She might complain of diffuse joint pain, fatigue and swollen hands and fingers. She might admit to new acid reflux and also to frequent episodes of her fingers turning colors when exposed to cold and pain in the fingers when they warm up. This is the Raynaud’s phenomenon already mentioned. Physical Exam: o Diffusely swollen hands/fingers o Early skin tightening in most distal
- 16. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL o aspects of extremities and around face o Changes in nail fold capillaries An important part of the physical exam is nail-fold microscopy (or nail-fold capillaroscopy). This is accomplished by looking closely with an ophthalmoscope at the capillaries near the cuticles. The picture on DOWN demonstrates possible findings. Panel a: normal nailfold capillaries Panel b: mild abnormalities (dilation of capillary loops) Panel c: dilation of capillaries and “dropout” Panel d: grossly abnormal Nailfold capillaroscopy is very important because many people, especially young women, experience Raynaud’s, but most of them never go on to develop systemic sclerosis or any other disease related to the Raynaud’s. This is called primary Raynaud’s (as opposed to secondary Raynaud’s when it is related to an underlying condition). Patients with primary Raynaud’s will have normal nailfold capillaries. If the nailfold capillaries are abnormal, the risk of going on to develop systemic sclerosis or another connective tissue disease is much greater.
- 17. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL LABORATORY: 1. ANA: Are the most frequently detected Not specific for SCL. Seen in up to 10% normal people. >95% of SCL patients Anticentromere – o 20—40% of patients with SCL. o Associated specifically with CREST ,sever digital ischemia and ulceration ,digital loss o Can be found in patient with PBC and sjogrens syndrome. Antitopoisomerase I (( antiSCL 70 )) 20---40% of patient with SCL Typically have diffuse skin changes ,ILD ,and worse prognosis Africans Americans Highly specific for SCL. Anti –RNP I II III (( RNA polymerase )) Associated with diffuse skin changes ,cardiac ,renal involvement and increased mortality. Anti U3 RNP ---antifibrillarian ----8% lung disease ,diffuse Anti U1 RNP ---------------------------5% MCTD Anti TH/TO ---------------------------- 1—5% limited cutaneous ,lung 2. Baseline kidney and liver function, CBC, ESR and CRP 3. LUNG INVOLVEMENT: Recommendations for Screening and Detection of SSc-Associated PAH--- A. Initial SSc Screening Evaluation: FT with DLCO (high) Transthoracic echocardiogram (TTE) (high) NT- Pro BNP (mod) DETECT algorithm if DLCO% < 60% and >3 yrs disease duration (mod) B. Frequency of Noninvasive Tests TTE annually as screening (low); if new signs or symptoms develop (high) PFT with DLCO annually as screening (low qual); if new signs or symptoms develop (low) NT-Pro BNP if new signs of symptoms develop (low) ECHO OR RIGHT HEART CATHETERIZATION--- Recommendations for Screening and Detection of SSC-Associated PAH General Evidence-based Guidelines: 1) All patients with SSc should be screened for PAH . 2) All SSc and scleroderma-spectrum patients with a positive non-invasive screen should be referred for RHC . 3) RHC is mandatory for diagnosis of PAH.
- 18. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL TREATMENT: There is no cure for systemic sclerosis. However, there are treatments that ameliorate symptoms and prolong organ and patient survival. These treatments are instituted on a case-by-case basis, depending on the specific disease manifestations in an individual patient. Care of patients with systemic sclerosis requires an understanding of the potential complications of the disease and close monitoring, so treatment can be started early. BASICS IN TREATMENT--- No effective therapy for underlying disease process Treatment is targeted to specific organs involved Early recognition of internal organ involvement and aggressive treatment improve quality of life and increases survival time. Successful management of patients with SSc requires an understanding of the potential complications of the disease, close monitoring, and early institution of targeted therapies . Treatment of Raynaud’s Phenomenon: A cornerstone of management of Raynaud’s is patient education to achieve behavioral modification. All patients with Raynaud’s should be instructed to maintain a warm core body temperature and to avoid extreme temperature changes. They also should be counseled to avoid certain factors that can aggravate Raynaud’s, particularly smoking. Use of certain drugs like decongestants and repeated trauma should also be avoided. If pharmacologic intervention is necessary, the first line class of drugs is calcium channel blockers. This class of drugs is by far the most commonly used in the treatment of Raynaud’s, although their effectiveness is variable. If calcium channel blockers are ineffective or not tolerated, there are other classes of drugs frequently used, also with varying effectiveness. Behavioral Maintain warm core body temperature Avoidance of smoking, sympathomimetic drugs (decongestants), and repeated trauma/vibration of the hands and fingers Pharmacologic First line: Long-acting calcium channel blockers (amlodipine, nifedipine) Selective serotonin reuptake inhibitors (fluoxetine) Phosphodiesterase-5 inhibitors (sildenafil) Angiotensin II receptor blockers (losartan) Topical nitrates α 1-adrenergic receptor antagonists (prazosin) • Raynaud’s • Pulmonary arterial hypertension • Scleroderma renal crisis Vascular • Interstitial lung disease • Cutaneous/Musculoskeletal Immune suppressors/anti- inflammatories • Gastroesophageal reflux • GI dysmotilitySymptomatic
- 19. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL Treatment of Severe Raynaud’s and Digital Ulcers: Severe, digit-threatening Raynaud’s requires the use of potent vasodilating drugs. Most of these medications require intravenous or injection administration and carry significant side effects. They are also quite costly. Potent vasodilators Intravenous prostaglandin (iloprost, epoprostenol) Endothelin antagonist (bosentan) Treatment of Pulmonary Arterial Hypertension: cGMP cAMP Vasoconstriction and proliferation Endothelin receptor A Exogenous nitric oxideEndothelin-receptor antagonists Endothelin receptor B Phosphodiesterase type 5 inhibitor Vasodilation and antiproliferation Phosphodi esterase type 5 Vasodilation and antiproliferation Prostacyclin derivatives Nitric Oxide Endothelin-1 Pre-proendothelin L-arginine Prostaglandin I2 L-citrulline Nitric Oxide Pathway Endothelin Pathway Prostacyclin Pathway Endothelial cells Proendothelin Endothelial cells Arachidonic acid Smooth muscle cells Prostacyclin (prostaglandin I2) Smooth muscle cells Prostacyclins Epoprostenol, Treprostinil Iloprost (inhaled) PDE-5 Inhibitors Sildenafil, Tadalafil SGC Stimulator Riociguat Endothelin Receptor Antagonists Bosentan, Ambrisentan , Macitentan Adapted from Humbert M et al. N Engl J Med. 2004;351:1425-1436. Many of the same vasodilating drugs that are used in severe Raynaud’s are also used to treat pulmonary arterial hypertension. Typically the prostaglandin analogues are used as first line treatment in PAH and carry the burden of requiring continuous IV or subcutaneous infusion. An inhaled prostacyclin (iloprost) is available – this requires administration up to 9 times daily. Potent vasodilators Parenteral prostaglandins (epoprostenol) Inhaled prostacyclin (iloprost) Endothelin receptor antagonist (bosentan) Phosphodiesterase inhibitors (sildenafil) Treatment of Scleroderma Renal Crisis It is important for you to be familiar with the management of scleroderma renal crisis. Remember, early recognition is critical. Patients at high risk for SRC require home blood pressure monitoring. Evaluation of kidney function and red blood count should be done at any sign concerning for development of SRC. If SRC does develop, an ACE-inhibitor should be started immediately and titrated up to the maximum dose as tolerated. The ACE- inhibitor should be continued even if the patient goes on to require dialysis. ACE-inhibitors have revolutioned care of SRC – what used to be a fatal complication now carries 1- and 5- year survival rates of >70% and 60%, respectively.
- 20. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL Close Monitoring! Home blood pressure readings daily If BP rises, evaluate for evidence of kidney damage/dysfunction (blood in urine and rise in creatinine) and new anemia Treatment ACE-INHIBITORS (Treat aggressively to maximum dose as tolerated) Dialysis if necessary (with continued Ace-inhibitor) Use of Ace-inhibitors has changed what used to be an almost universally fatal complication of SSc to one with 1-year survival >70%, 5-year survival 60% (and long-term renal survival is 50-80%) Treatment of Inflammatory Manifestations---- Interstitial lung disease is largely mediated by an intense inflammatory reaction and is treated with strong immunosuppressive drugs. Typically the initial treatment of ILD is cyclophosphamide in combination with glucocorticoids. If the lungs improve, then less potent agents can be substituted (such as azathioprine and mycophenolate mofetil). The treatment of ILD is suboptimal – some patients do not respond and treatments are potentially very toxic. Therefore, researchers are actively looking at more effective and less toxic approaches. Some of the investigational therapies include stem cell transplant and antibody-based therapies such as imatinib and rituximab. Interstitial Lung Disease Cyclophosphamide (+/- low-dose glucocorticoids) Azathioprine Mycophenolate mofetil Investigational approaches: hematopoetic stem cell transplant, imatinib, rituximab, tadalafil Cutaneous/Musculoskeletal Physical therapy Methotrexate Azathioprine Low-dose glucocorticoids – with caution because of risk of SRC Monitoring for Complications--- Treatment of patients with systemic sclerosis requires “anticipatory management” (ie close monitoring for early detection of disease complications). It is reasonable to perform transthoracic echocardiograms and pulmonary function tests up to once every year in these patients to screen for pulmonary arterial hypertension, even if they don’t complain of cardiopulmonary symptoms (as their functional status may be quite compromised). Likewise, pulmonary function tests in combination with chest CT scan should be done at regular intervals to assess for the presence of interstitial lung disease. In patients at risk of scleroderma renal crisis, home blood pressure monitoring is indicated as is regular testing of urine and blood. Consider annual transthoracic echocardiography and pulmonary function tests to screen for pulmonary arterial hypertension (more frequent screening if symptoms develop) Pulmonary function tests and high resolution chest CT to assess for interstitial lung disease In patients at high risk for scleroderma renal crisis - home blood pressure readings daily and regular testing of kidney function and urine
- 21. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL PROGNOSIS: The prognosis for patients diagnosed with systemic sclerosis is better now than it was 25 years ago, but the potential for significant morbidity and early mortality is still substantial. Several factors are associated with a poor prognosis Highlights ((summary of the talk)): Systemic sclerosis is a multisystem autoimmune disease characterized by inflammation, disordered connective tissue metabolism and functional and structural abnormalities in blood vessels, all contributing to progressive fibrosis of the skin and visceral organs. The primary target organs are skin, lungs, kidney, and gastrointestinal tract. The symptoms are quite varied but the most characteristic clinical features are Raynaud’s, skin tightening/fibrosis, interstitial lung disease, pulmonary arterial hypertension, scleroderma renal crisis, and GI tract dysmotility. Systemic sclerosis is a multisystem autoimmune disease characterized by inflammation, disordered connective tissue metabolism and functional and structural abnormalities in blood vessels, all contributing to progressive fibrosis of the skin and visceral organs Primary target organs: skin, lungs, kidney, GI tract Cardinal clinical features: Raynaud’s, skin tightening, interstitial lung disease, pulmonary arterial hypertension, scleroderma renal crisis, GI tract dysmotility Important aspects of management include: Close monitoring for complications (including home BP and close monitoring for lung involvement) Calcium channel blockers for Raynaud’s •dcSSc 40-60% at 10 years •lcSSc >70% at 10 years Overall survival: •Rapidly progressive skin involvement •Older age at disease onset •African- or Native-American race •Severe lung involvement •Large pericardial effusion •Proteinuria, hematuria, renal failure •Anemia •Elevated ESR •Abnormal ECG •Anti-Scl 70 (anti-topoisomerase) antibodies – increased risk of severe pulmonary fibrosis •Anti-RNA-polymerase antibodies – increased risk of scleroderma renal crisis Poor prognosis associated with:
- 22. SCLERODERMA 2016 DR MAGDI AWAD SASI LIBYAN MEDICAL BOARD 7 TH OCTOPER HOSPITAL Ace-inhibitors for scleroderma renal crisis Vasodilators for pulmonary arterial hypertension Immunosuppression for interstitial lung disease
