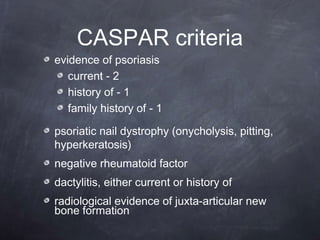
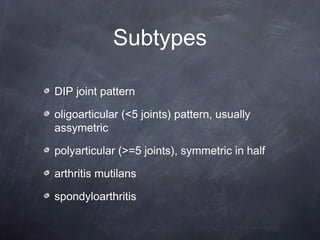
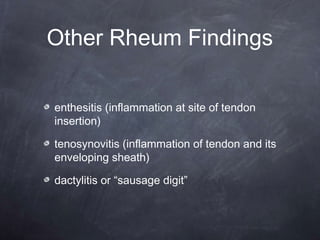
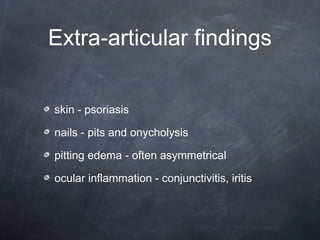
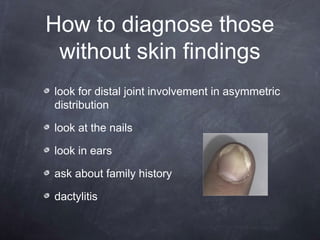
Psoriatic arthritis is an inflammatory arthritis associated with psoriasis that is usually seronegative. It affects between 0.04-1.2% of the population equally in men and women, with peak age of onset between 30-55 years. It is characterized by distal joint involvement in an asymmetric distribution, nail changes like pits and onycholysis, and dactylitis. Diagnosis is based on evidence of psoriasis, negative rheumatoid factor, and radiological evidence of new bone formation near joints. While initially thought to be more benign than rheumatoid arthritis, progression of clinical damage occurs over time in most patients despite treatment.