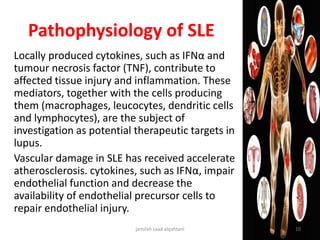
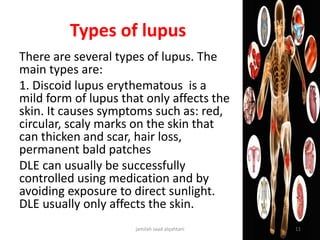
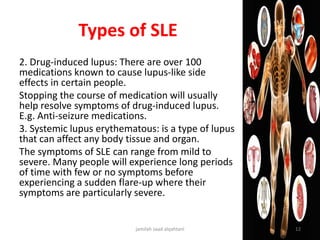
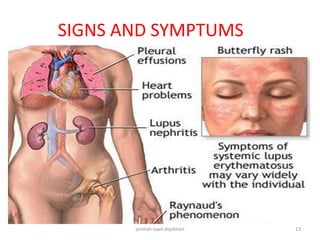
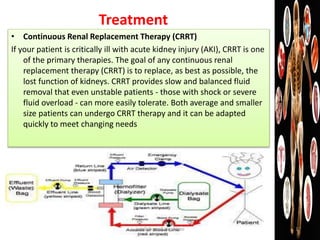
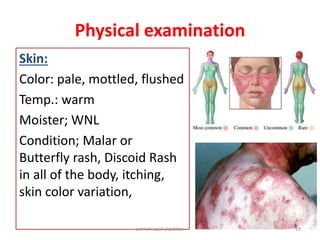
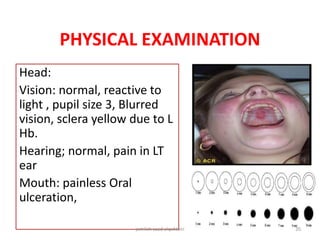
The document presents a case study of a 41-year-old Saudi female patient diagnosed with systemic lupus erythematosus (SLE) and chronic kidney disease (CKD), detailing her treatment journey including plasmapheresis and renal biopsy. It discusses SLE's pathophysiology, types, diagnostic criteria, and ongoing management therapies such as continuous renal replacement therapy. Additionally, it outlines pharmacological treatments, symptomatology, and nursing care approaches tailored to managing chronic pain, activity intolerance, and cardiac output issues related to SLE.
![Diagnosis of lupus
The following are 11 criteria used for diagnosing systemic
lupus erythematosus:
1. Malar (over the cheeks of the face) "butterfly" rash
2. Discoid skin rash (patchy redness with
hyperpigmentation and hypopigmentation that can
cause scarring)
3. Photosensitivity (skin rash in reaction to sunlight
[ultraviolet light] exposure)
4. Mucous membrane ulcers (spontaneous sores or ulcers
of the lining of the mouth, nose, or throat)
5. Arthritis (two or more swollen, tender joints of the
extremities)
6. Pleuritis or pericarditis (inflammation of the lining tissue
around the heart or lungs, usually associated with chest
pain upon breathing or changes of body position)
7. Kidney abnormalities (abnormal amounts of urine
protein or clumps of cellular elements called casts
detectable with a urinalysis)
jamilah saad alqahtani 14](https://image.slidesharecdn.com/sle-180509082035/85/Systemic-Lupus-Erythematous-SLE-14-320.jpg)
![Diagnosis of lupus
8. Brain irritation (manifested by seizures
[convulsions] and/or psychosis, referred
to as "lupus cerebritis")
9. Blood-count abnormalities: low (WBC)
or red (RBC), or platelet count on routine
complete blood count testing)
10. Immunologic disorder
11. Antinuclear antibody (positive ANA
antibody testing [antinuclear antibodies
in the blood])
jamilah saad alqahtani 15](https://image.slidesharecdn.com/sle-180509082035/85/Systemic-Lupus-Erythematous-SLE-15-320.jpg)
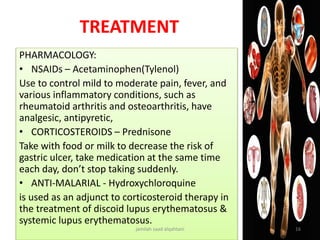
![Treatment
• Plasmaphersis:
Plasmapheresis is a term used to refer to a broad range of procedures in which extracorporeal
separation of blood components results in a filtered plasma product.[1, 2] The filtering of plasma
from whole blood can be accomplished via centrifugation or semipermeable membranes.[3]
Centrifugation takes advantage of the different specific gravities inherent to various blood
products such as red cells, white cells, platelets, and plasma.[4] Membrane plasma separation uses
differences in particle size to filter plasma from the cellular components of blood.[3]
• Traditionally, in the United States, most plasmapheresis takes place using automated centrifuge-
based technology.[5] In certain instances, in particular in patients already undergoing hemodialysis,
plasmapheresis can be carried out using semipermeable membranes to filter plasma.[4]
• In therapeutic plasma exchange, using an automated centrifuge, filtered plasma is discarded and
red blood cells along with replacement colloid such as donor plasma or albumin is returned to the
patient. In membrane plasma filtration, secondary membrane plasma fractionation can selectively
remove undesired macromolecules, which then allows for return of the processed plasma to the
patient instead of donor plasma or albumin. Examples of secondary membrane plasma
fractionation include cascade filtration,[6] thermofiltration, cryofiltration,[7] and low-density
lipoprotein pheresis
jamilah saad alqahtani 18](https://image.slidesharecdn.com/sle-180509082035/85/Systemic-Lupus-Erythematous-SLE-18-320.jpg)
![CRANIAL NERVE (CN) FUNCTION
CN I – olfactory [√ ] intact [ ] impaired [ ] unknown
CN’s II-III-IV-VI– optic, oculomotor, trochlear,
abducens (eye exam)
CN V– trigeminal (facial sensory & jaw motor) [√]
intact [ ] impaired
CN VII - Facial (symmetry in face expressions & taste)
[√] intact [ ] impaired
CN VIII – Acoustic (hearing exam)
CN IX – Glossopharyngeal (taste at back of tongue) [√
] intact [ ] impaired
CN X - Vagus (palate movement, “ah” and vocal motor
[√] intact [ ] impaired
CN XI – Spinal Accessory (head motion & shrug) [√]
intact [ ] impaired
CN XII – Hypoglossal (tongue position & motor) [√ ]
intact [ ] impaired
SENSORY FUNCTION
Touch [√ ] intact [ ] impaired
jamilah saad alqahtani 22](https://image.slidesharecdn.com/sle-180509082035/85/Systemic-Lupus-Erythematous-SLE-22-320.jpg)
![1987 ACR Classification Criteria for Rheumatoid Arthritis
Patients must have four of the seven criteria:
• Morning stiffness lasting at least 1 hour*
• Swelling in three or more joints*
• Swelling in hand joints*
• Symmetric joint swelling*
• Erosions or decalcification on x-ray of hand
• Rheumatoid nodules
• Abnormal serum rheumatoid factor
*must be present at least six weeks
MOTOR FUNCTION
[ ] impaired coordination [√ ] fine motor skills impaired due to deformity in
the metaphalengeal
[ ] balance maintained while standing with eyes closed [√ ] loss of balance
immediate
REFLEXES
patellar reflex: [ ] 0: no response [√] 1+ low (normal with slight contraction
[ ] 2+ normal, visible muscle twitch and extension of lower leg [ ] 3+ brisker
than normal [ ] 4+ hyperactive, very brisk
jamilah saad alqahtani 23](https://image.slidesharecdn.com/sle-180509082035/85/Systemic-Lupus-Erythematous-SLE-23-320.jpg)
![Respiratory
Auscultated breath sounds:
[√] vesicular sounds at periphery
[√] bronchovesicular sounds between
scapulae or 1st – 2nd intercostal space
lateral to sternum
[√] bronchial sounds over trachea
jamilah saad alqahtani 25](https://image.slidesharecdn.com/sle-180509082035/85/Systemic-Lupus-Erythematous-SLE-25-320.jpg)
![Gastrointestinal
[√ ] constipation: enema given
[√ ] distention
Bowel Sounds:
[√ ] Present in all quadrants
[√ ] poor appetite or loss of
appetite
jamilah saad alqahtani 26](https://image.slidesharecdn.com/sle-180509082035/85/Systemic-Lupus-Erythematous-SLE-26-320.jpg)