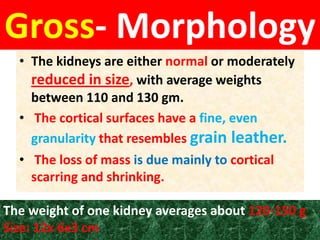
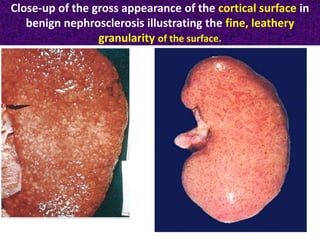
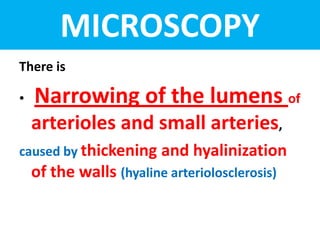
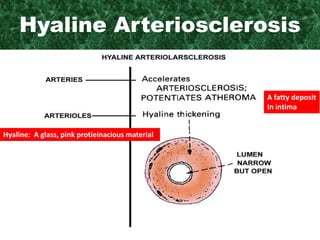
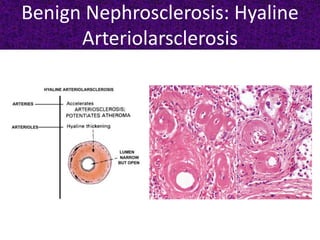
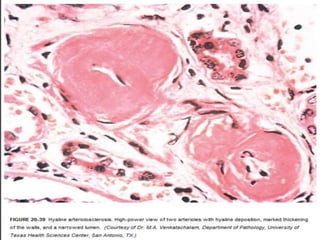
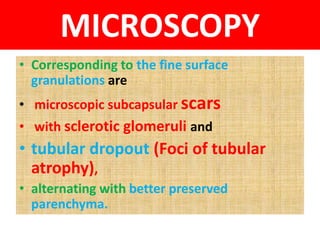
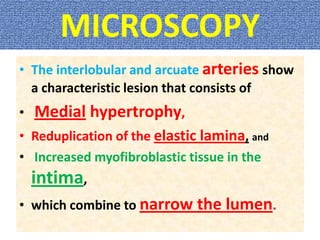
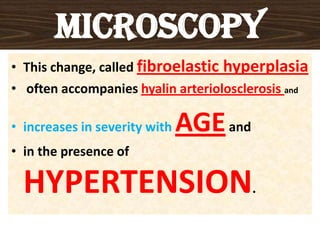
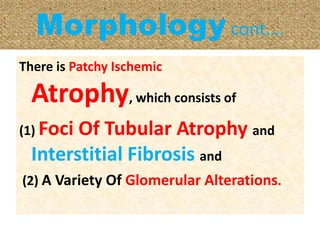
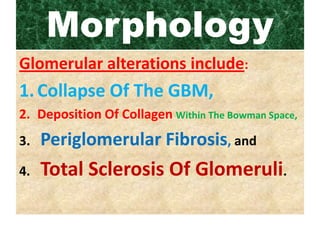
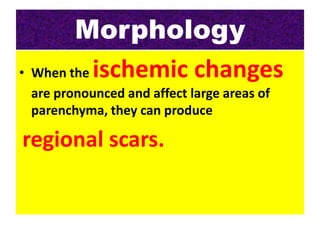
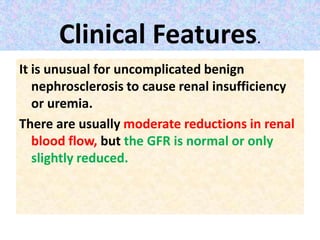
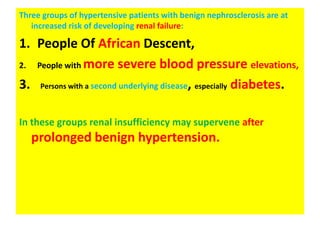
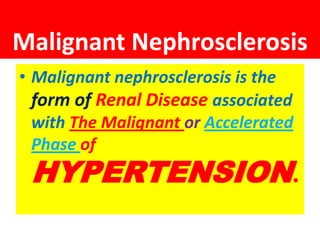
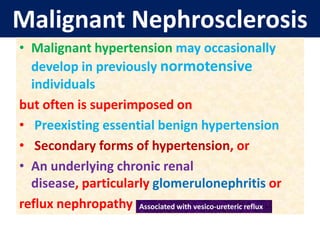
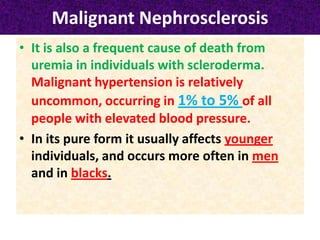
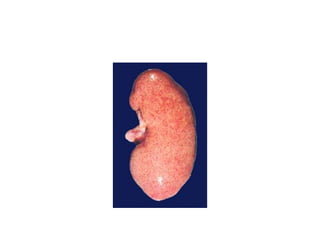
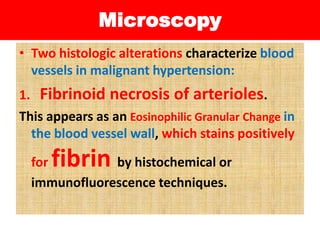
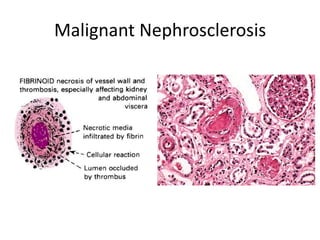
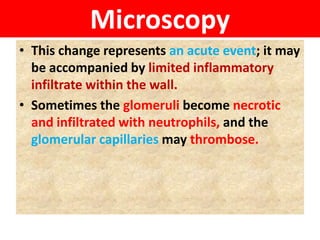
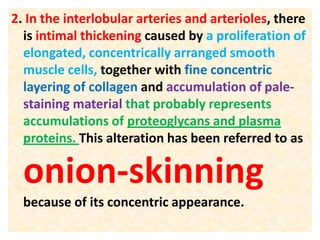
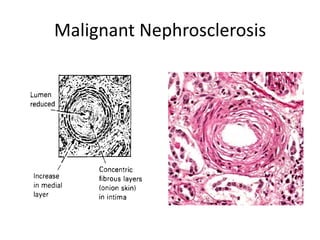
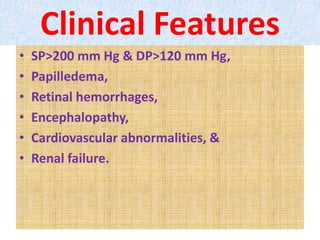
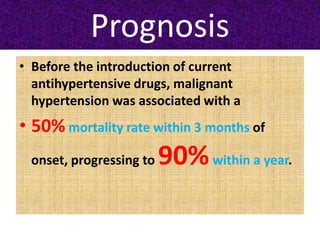
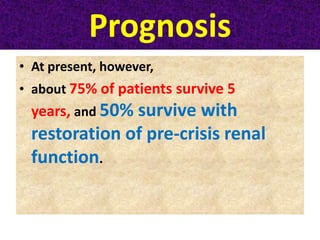
This document discusses two types of nephrosclerosis: benign and malignant. Benign nephrosclerosis is caused by thickening of renal arterioles over time from aging, hypertension, or diabetes. It can cause scarring and loss of renal function. Malignant nephrosclerosis involves a worsening of hypertension that damages renal vessels, causing ischemia and sudden loss of function. The pathology involves fibrinoid necrosis and intimal thickening of arteries. Aggressive treatment of high blood pressure is needed to prevent permanent kidney damage in malignant nephrosclerosis.