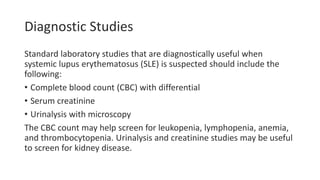
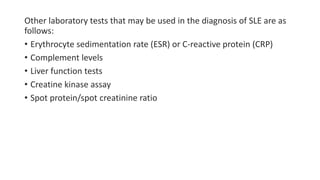
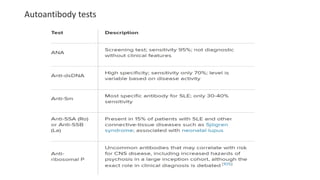
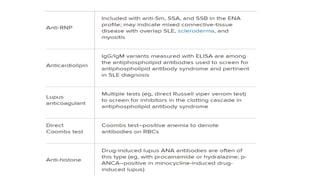
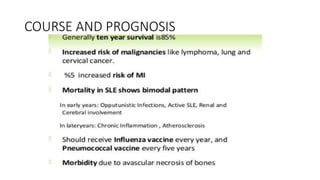
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that can affect various organs in the body. Common symptoms include fatigue, joint pain, rashes, and kidney problems. It is caused by genetic and environmental factors that lead to abnormal immune responses against the body's own tissues. Diagnosis involves evaluating clinical features along with blood tests to detect autoantibodies. Treatment depends on the specific organs involved but may include medications to suppress the immune system.



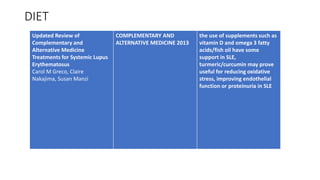
![Gastrointestinal
• Infectious causes (bacterial, viral [eg, CMV]), because of
immunosuppression.
• Nausea and dyspepsia are common symptoms in patients with active
SLE.
• Peptic ulcer disease is a common complication, especially in SLE
patients treated with nonsteroidal anti-inflammatory agents (NSAIDs)
and glucocorticoids.
• Occasionally, abdominal pain in active SLE may be directly related to
active lupus, including peritonitis, pancreatitis, mesenteric vasculitis,
and bowel infarction.
• Rarely, lupus enteritis may be the initial manifestation of SLE.
• Jaundice due to autoimmune hepatobiliary disease may also occur.](https://image.slidesharecdn.com/slecd-210711051133/85/Systemic-lupus-erythmatosus-27-320.jpg)

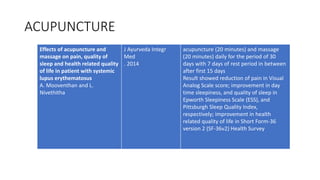
![Integrated Yoga Practice in
Cardiac Rehabilitation Program: A
Randomized Control Trial
J Altern Complement Med
. 2020
yoga-practicing group showed significant
reduction in depression (Cardiac
Depression Scale [CDS], U = 71, p value =
0.0), anxiety (Hamilton Anxiety Rating
Scale [HAM-A], U = 128, p value = 0.0),
and a significant increase in quality of life
(QOL) scores (Duke Activity Status Index
[DASI], U = 146, p value = 0.0; and
metabolic equivalents (METs), U =
136, p value = 0.0) at 3 months
compared to control.](https://image.slidesharecdn.com/slecd-210711051133/85/Systemic-lupus-erythmatosus-65-320.jpg)