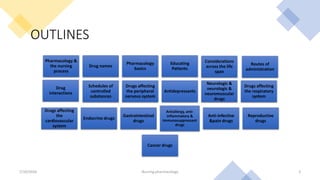
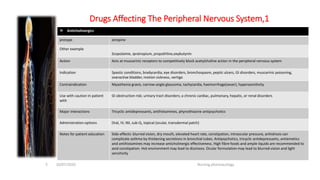
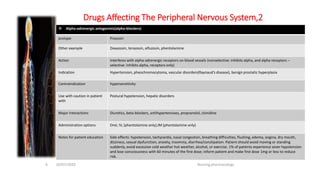
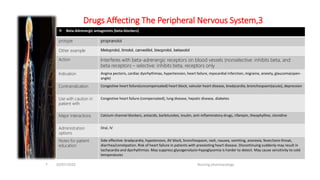
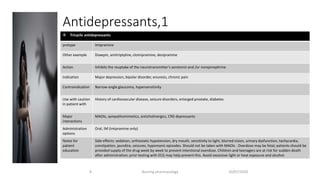
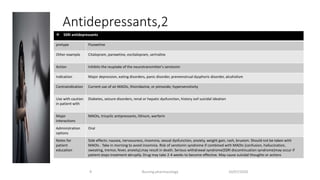
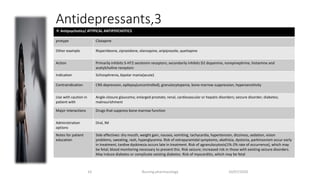
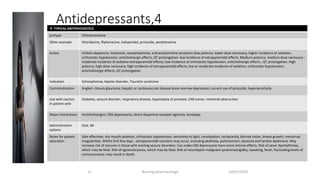
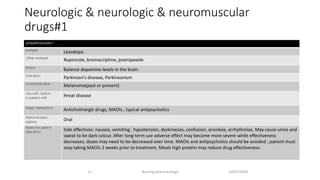
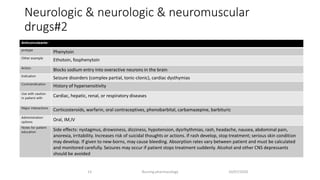
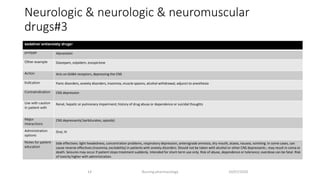
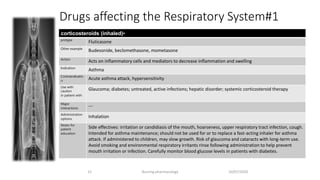
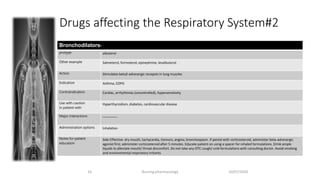
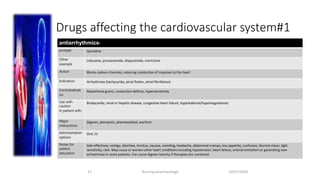
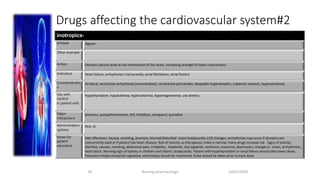
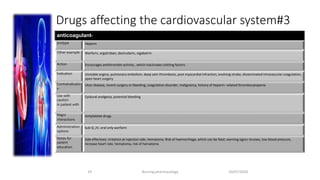
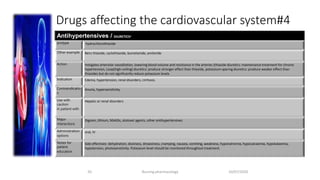
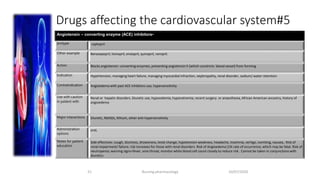
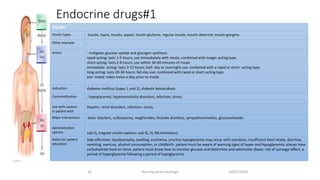
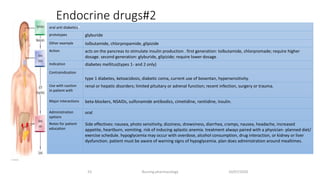
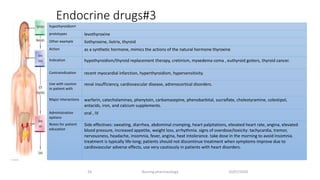
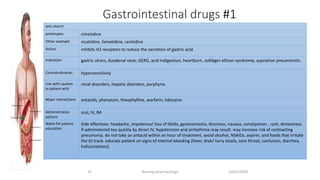
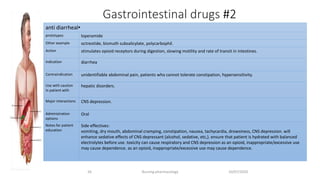
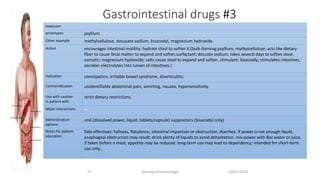
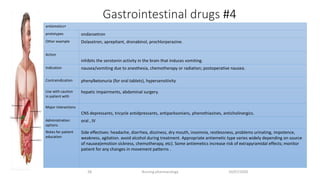
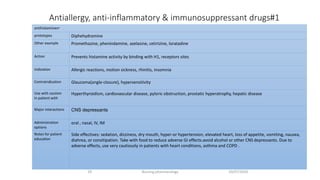
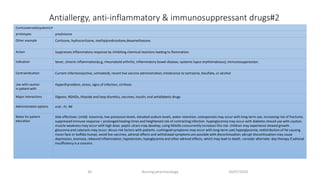
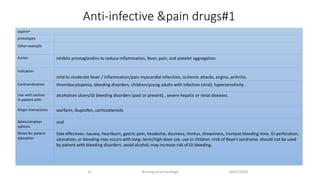
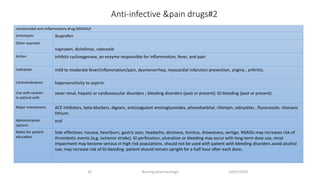
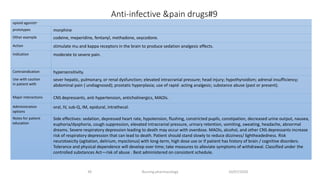
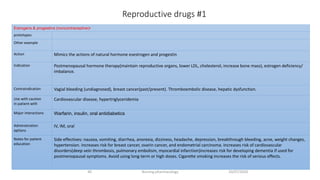
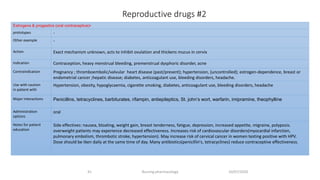
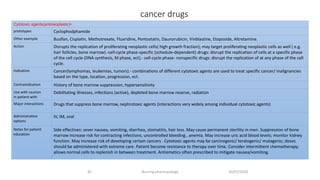
The document discusses various drug classes relevant to nursing pharmacology, including their prototype drugs, actions, indications, contraindications, interactions, and side effects. It covers drugs affecting the peripheral nervous system, antidepressants, antipsychotics, and medications for respiratory, cardiovascular, and neurologic conditions, emphasizing the importance of detailed drug knowledge for safe nursing practice. Patient education and precautions for administering these medications are also highlighted throughout the material.