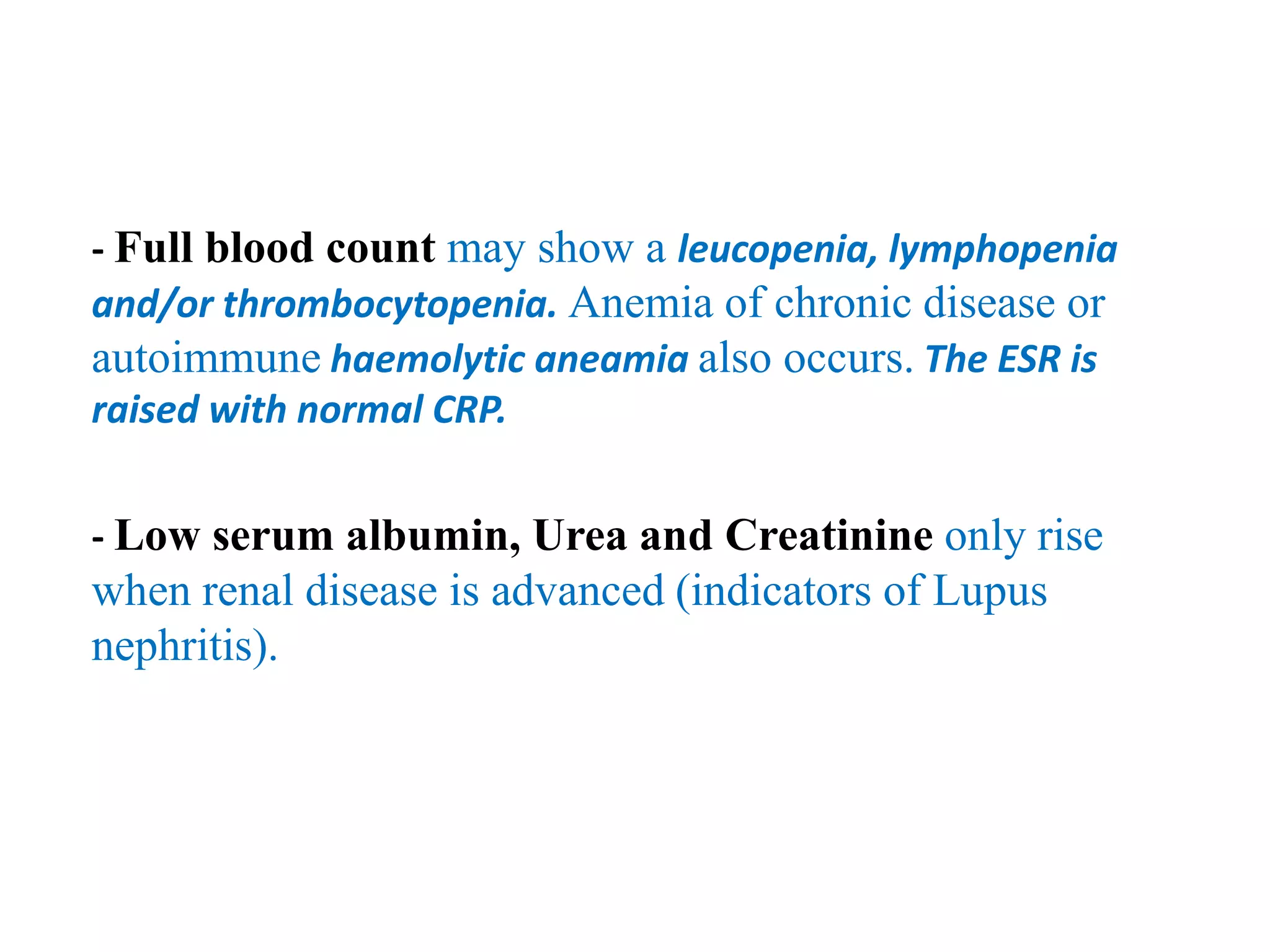
A 40-year-old woman presents with a butterfly rash on her face along with arthralgia, alopecia, and fatigue but no fever. The most likely diagnosis is systemic lupus erythematosus (SLE). SLE is a multi-system autoimmune disease that commonly involves the joints and skin and can also affect organs like the brain, heart, lungs, kidneys and more. Laboratory tests would include a complete blood count, serum chemistry, and autoantibody tests like ANA, anti-dsDNA, and anti-Sm. For mild cases, treatment would include topical corticosteroids, NSAIDs, and antimalarial drugs. Regular check-ups are advised to