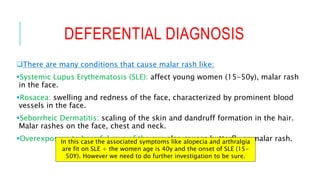
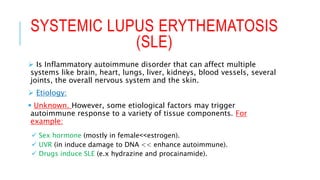
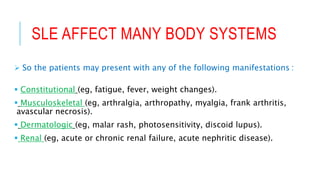
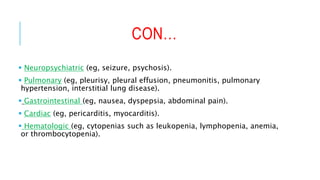
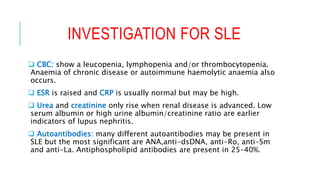
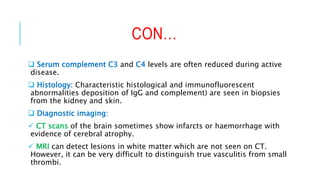
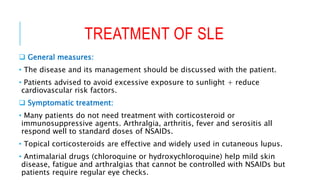
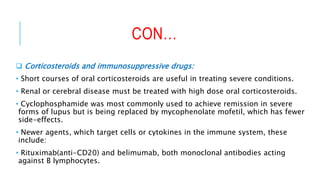
The document discusses a clinical case of a 40-year-old woman presenting with a butterfly rash, arthralgia, alopecia, and fatigue, suggesting a potential diagnosis of systemic lupus erythematosus (SLE). It outlines the involvement of various organs by SLE, necessary laboratory tests for diagnosis, initial therapeutic measures, and advice for patient follow-ups if no other organ involvement is noted. The treatment options include general measures, symptomatic treatments, corticosteroids for severe conditions, and newer agents targeting immune system cells.


![REFERENCE
Kumar and Clark’s Clinical medicine, eight edition, page (536-
537).
Shahedi, SLEWorkup: Laboratory Studies, Imaging Studies,
Procedures. [online] Emedicine.medscape.com.
https://www.hxbenefit.com/malar-rash-butterfly-rash-pictures-causes-
and-treatment.html](https://image.slidesharecdn.com/vignetteb-170527174031/85/Systemic-lupus-erythematosus-SLE-20-320.jpg)