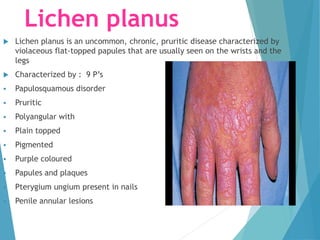
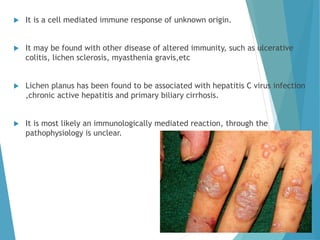
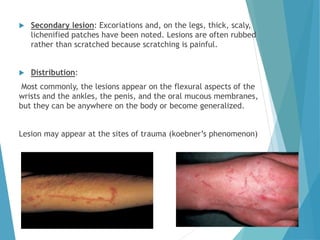
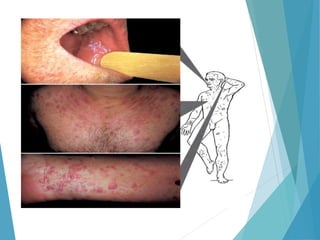
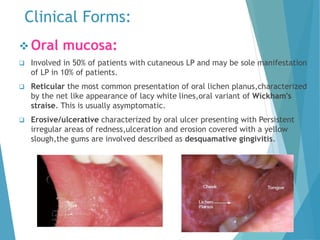
Lichen planus is a chronic inflammatory skin condition that causes itchy, purple-colored papules and plaques. It is thought to be an autoimmune reaction targeting skin cells. The lesions typically appear on the wrists, legs, and oral mucosa. On microscopy, distinctive saw-tooth shaped keratinocytes (Civatte bodies) and band-like inflammatory infiltrate are seen. Treatment involves topical corticosteroids and immunomodulators. While usually self-limiting, lichen planus can lead to scarring and has a small risk of malignant transformation, especially in oral lesions.





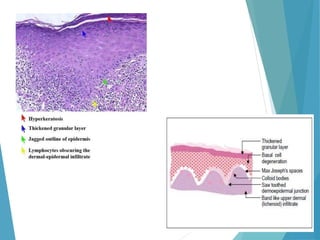
![Histopathology:
Distinguishing histopathologic features of lichen planus include the
following:
Hyperkeratotic epidermis with irregular acanthosis and focal thickening
in the granular layer
Degenerative keratinocytes (colloid or Civatte bodies) in the lower
epidermis; in addition to apoptotic keratinocytes, colloid bodies are
composed of globular deposits of IgM (occasionally immunoglobulin G
[IgG] or immunoglobulin A [IgA]) and complement
Linear or shaggy deposits of fibrin and fibrinogen in the basement
membrane zone
In the upper dermis, a bandlike infiltrate of lymphocytic (primarily
helper T) and histiocytic cells with many Langerhans cells](https://image.slidesharecdn.com/lp-160610182350/85/Lichen-planus-18-320.jpg)