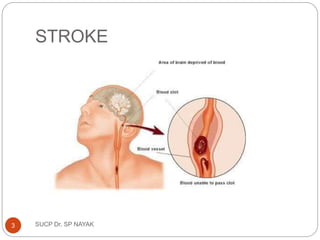
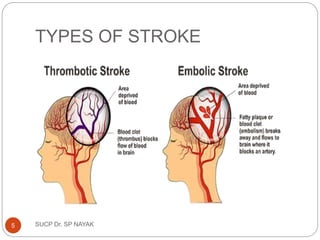
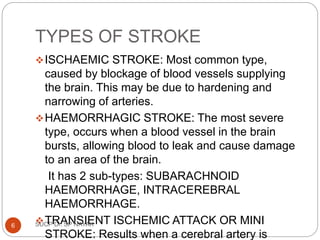
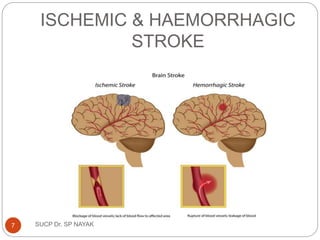
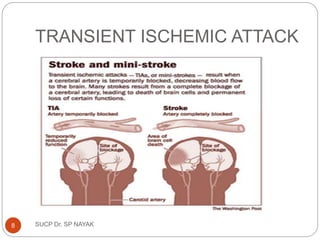
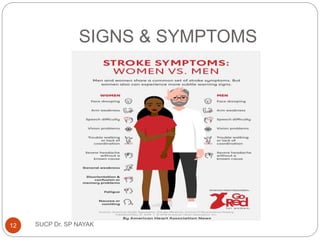
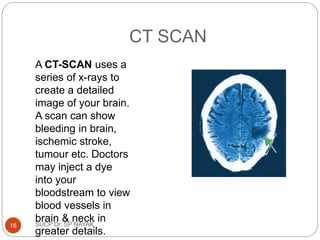
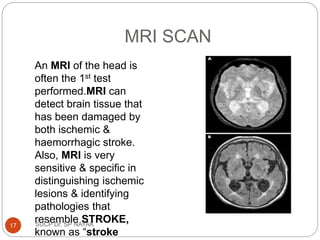
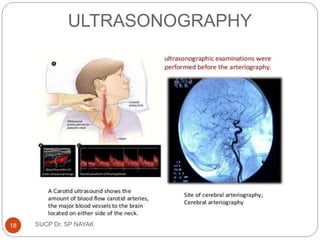
The document presents a comprehensive overview of strokes, including their definition, types (ischemic, hemorrhagic, and transient ischemic attacks), risk factors, and pathophysiology. It outlines the clinical presentation, complications, diagnostic methods, treatment goals, and both non-pharmacologic and pharmacologic therapies for managing strokes. Additionally, it discusses patient counseling and preventive measures to reduce the risk of stroke.