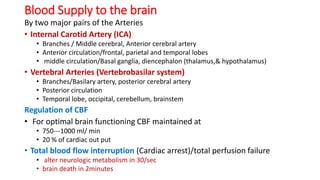
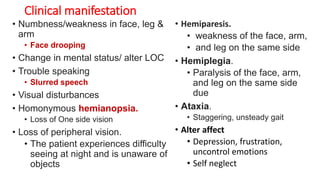
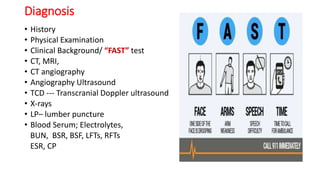
Stroke occurs when blood flow to the brain is interrupted, depriving brain cells of oxygen and nutrients. It is a leading cause of death and disability. The main types are ischemic (caused by clots) and hemorrhagic (caused by bleeding). Risk factors include age, gender, hypertension, heart disease, diabetes, and lifestyle factors like smoking and obesity. Symptoms depend on the affected area of the brain but may include weakness, trouble speaking, vision issues, and altered mental status. Diagnosis involves medical history, exam, and tests like CT/MRI. Treatment focuses on prevention for those at risk and management of acute issues like blood pressure as well as rehabilitation. Lifestyle changes and controlling underlying conditions can help