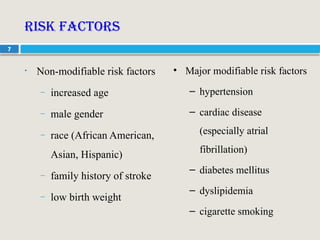
The document provides a comprehensive overview of stroke, including its definition, types (ischemic and hemorrhagic), epidemiology, risk factors, pathophysiology, clinical presentation, diagnostic tests, and treatment approaches. It emphasizes the importance of rapid diagnosis and appropriate interventions to reduce neurological injury and long-term disability. The treatment strategies include both pharmacological options and non-pharmacological methods depending on the type of stroke.