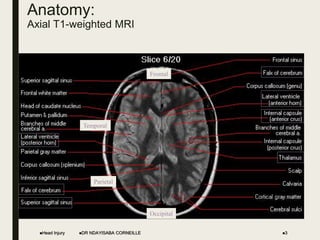
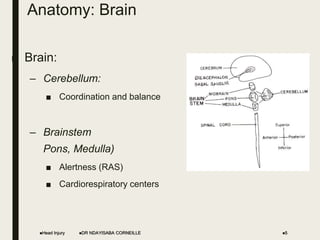
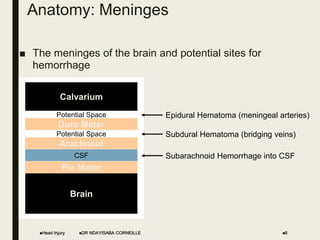
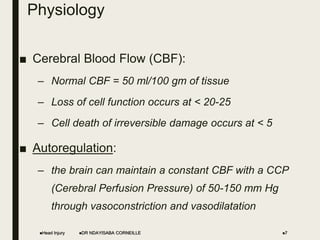
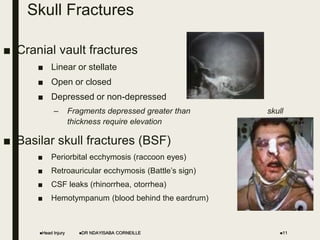
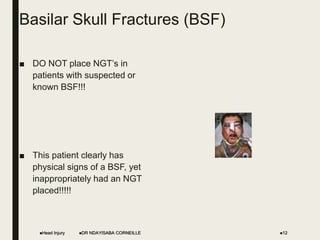
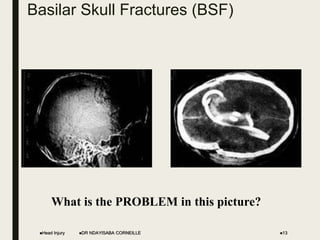
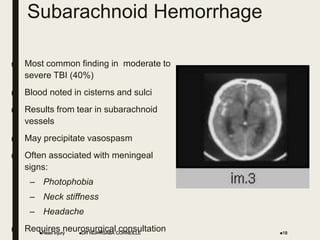
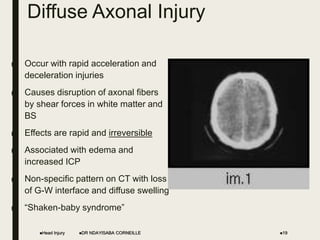
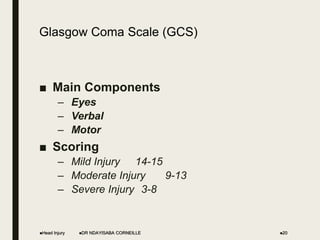
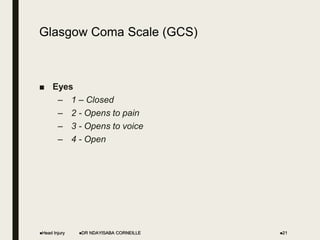
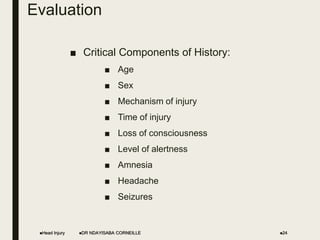
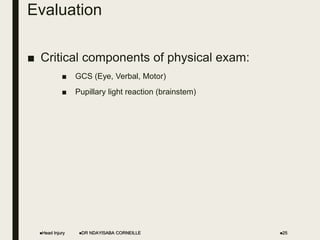
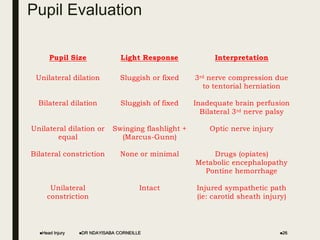
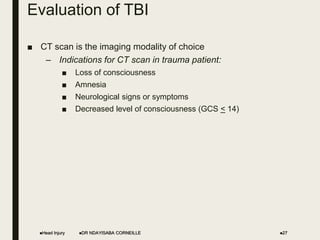
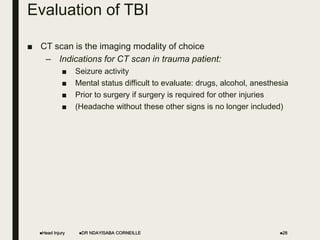
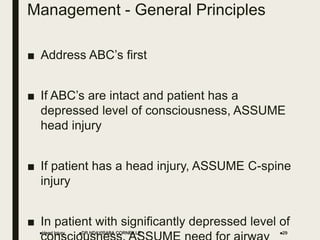
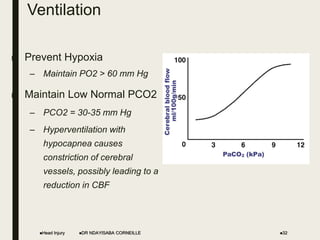
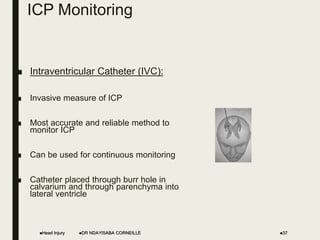
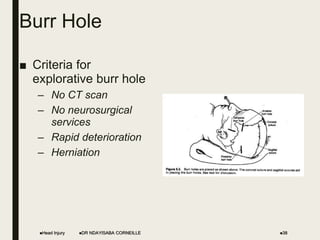
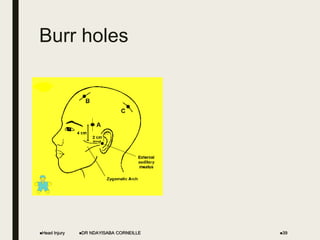
The document provides an overview of head injuries, including definitions, risk factors, and anatomy related to traumatic brain injury (TBI). It describes the classification, evaluation methods, and management strategies for TBI, emphasizing the importance of monitoring cerebral perfusion pressure and intracranial pressure. Critical treatment protocols are outlined, focusing on preventing secondary brain injury and the necessity of timely interventions.