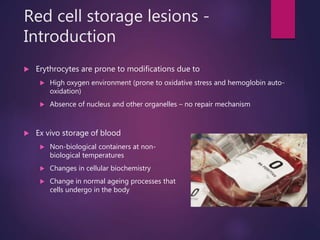
The document discusses storage lesions in red blood cells and platelets, outlining the biochemical and biomechanical changes that occur during ex vivo preservation, which ultimately reduce their functionality and survival. Key factors include oxidative stress, metabolic alterations, and membrane integrity issues that arise from storage conditions, leading to adverse effects post-transfusion. Strategies to mitigate these storage lesions include optimizing storage solutions, conditions, and potential rejuvenation techniques.











![Biomechanical effects
Membrane changes occur in parallel with metabolic changes
RBC shape maintenance -> dependent on [ATP]
Shape changes due to ATP depletion
Echinocytes/burr cells
Greek – sea urchin
Disk shaped cells with projections on the membrane
reversible
Sphero-echinocytes
With further depletion of total ATP and ADP pool
spherical red cells with thorny projections
decreased surface to volume ratio and deformability -> reduce RBC
post-transfusion survival
Irreversible change
Microvesiculation occurs from the tips of echinocytic spines](https://image.slidesharecdn.com/storagelesions-170117170618/85/Red-cell-and-platelet-storage-lesions-and-their-effect-in-transfusion-practise-13-320.jpg)































