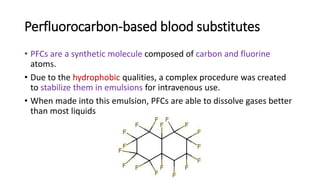
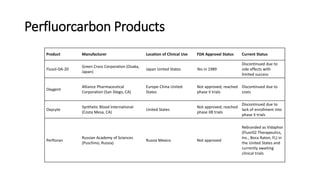
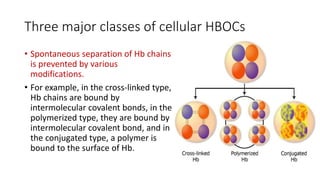
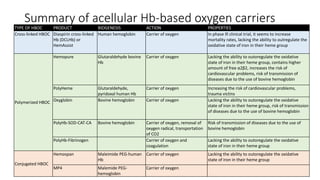
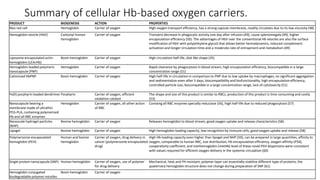
Artificial blood substitutes, also called oxygen therapeutic agents (OTAs), have been in development for decades using two main approaches: perfluorocarbon-based substitutes and hemoglobin-based carriers. Currently, there are no FDA-approved OTAs due to toxicities. Promising new developments include stem cell-derived red blood cells, which could provide an unlimited source with high similarity to natural red blood cells. Future studies may focus on producing safe and effective red blood cells from differentiated stem cells.