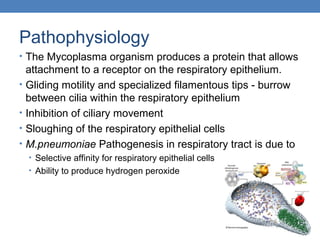
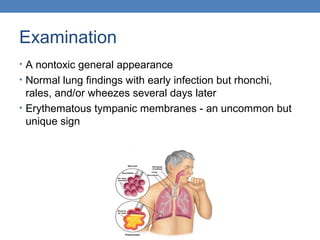
Mycoplasma pneumoniae is the smallest free-living organism that causes pneumonia in humans. It lacks a cell wall and resides extracellularly in the respiratory tract. Common symptoms include fever, cough, headache, and sore throat. Examination may reveal rhonchi or rales in the lungs. Diagnosis is confirmed through PCR testing of respiratory samples, though this is not used in clinical practice. Treatment involves antibiotics like erythromycin, clarithromycin, or azithromycin for 7-10 days.