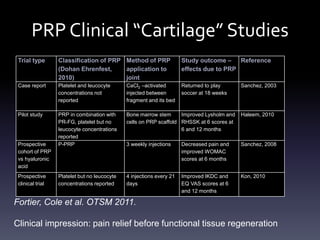
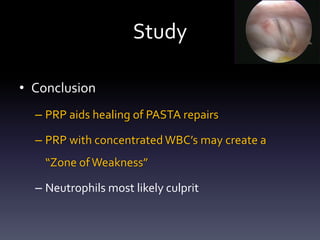
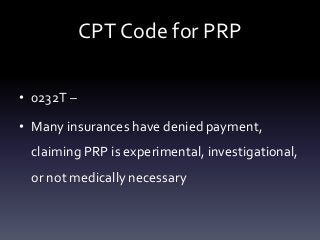
This document provides information about platelet-rich plasma (PRP) and its use in orthopedic applications. It discusses:
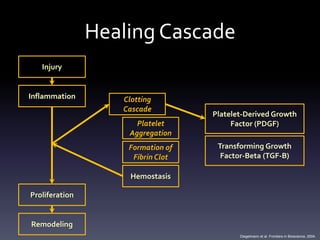
1) The basic science behind PRP, including the clotting cascade and platelet function. Platelets release growth factors that promote healing when they aggregate at the site of injury.
2) How PRP is created by concentrating the platelet fraction that is separated after centrifugation of blood. There is no consensus on the optimal platelet concentration.
3) The two main types of PRP systems - buffy coat systems and plasma based systems. Buffy coat systems require more steps but produce a higher platelet concentration, while plasma based systems are simpler.
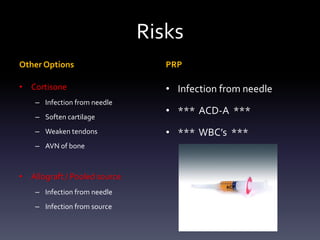
4) Potential risks of PR




![Platelet Function
• Dose-Response relationship of [Platelets] to
– Proliferation of human adult MSC’s
• Mesenchymal stem cells
– Proliferation of fibroblasts
– Production of type I collagen
• MSC proliferation directly related to PDGF release by α
granules from platelets](https://image.slidesharecdn.com/platelet-richplasmaaug2012-120811172404-phpapp02/85/Platelet-Rich-Plasma-7-320.jpg)

![Consensus?
• Marx states PRP = 1,000,000 platelets/uL
• Anitua claims PRP = 300,000 platelets/uL
• Others discuss 3 – 5 fold increase [platelet] > baseline
• What level needed to improve healing?
– Weibrich suggests that each individual requires a different platelet
concentration ratio
– Graziani found 2.5x to be ideal level for osteoblast & fibroblast
proliferation. Greater levels reduced response Marx et al, J Oral Maxillofac Surg, 2004.
Marx et al, Imp Dent, 2001.
Anitua et al, Thromb Haemost, 2004.
Marx et al, Bone Engineering, 2000.
Kevy et al, J Extra Corpor Technol, 2004.
Gonshor, Int J Periodontics Restorative Dent, 2002.
Weibrich, J Craniomaxillofac Surg, 2002.
Graziani et al, Clin Oml Impl Res, 2006](https://image.slidesharecdn.com/platelet-richplasmaaug2012-120811172404-phpapp02/85/Platelet-Rich-Plasma-9-320.jpg)