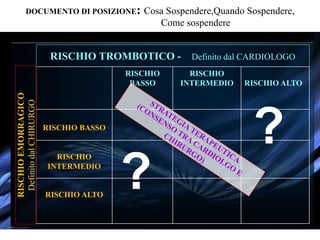
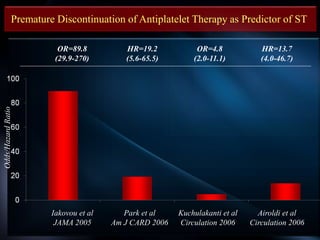
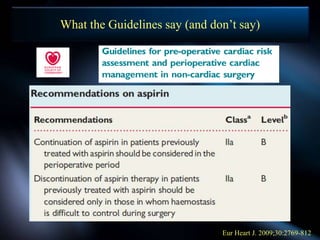
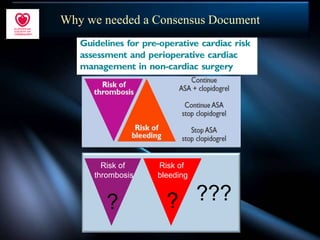
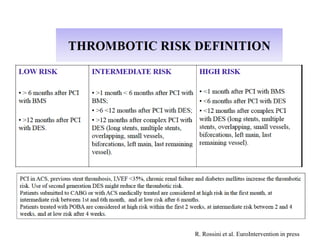
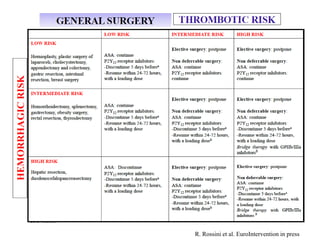
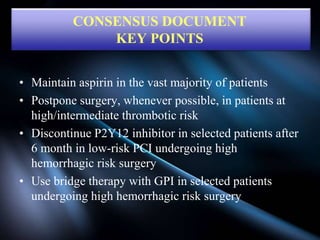
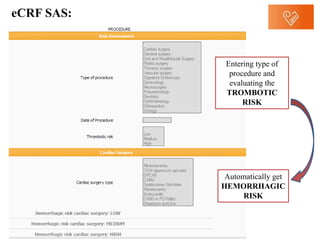
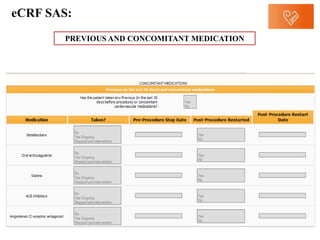
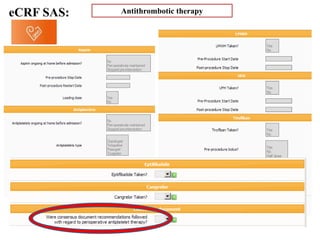
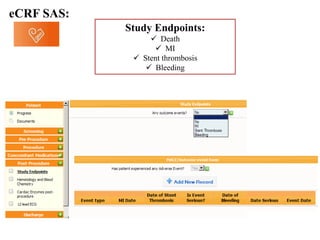
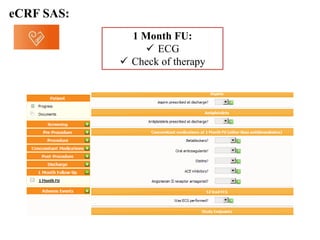
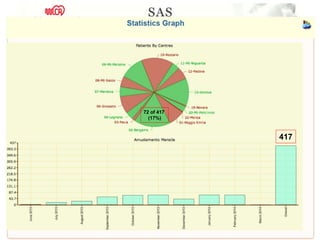
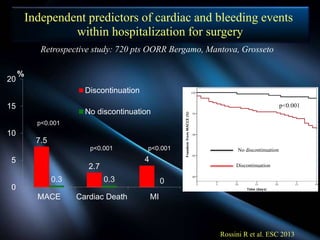
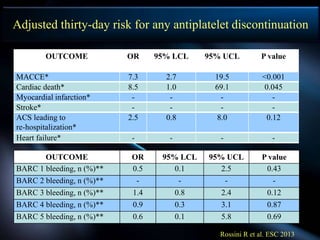
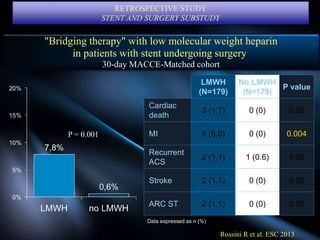
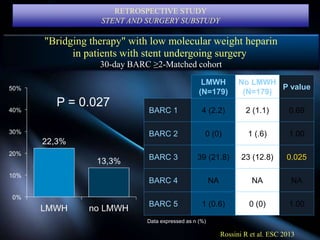
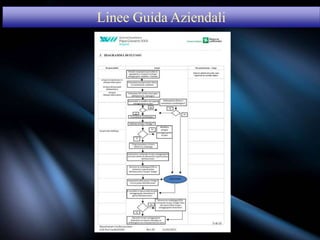
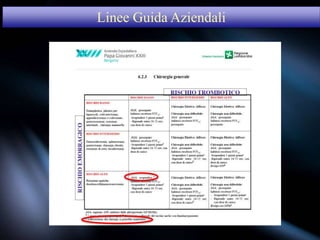
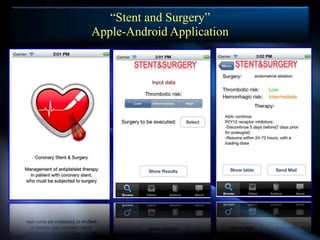
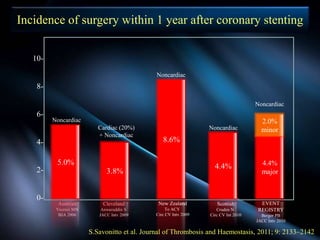
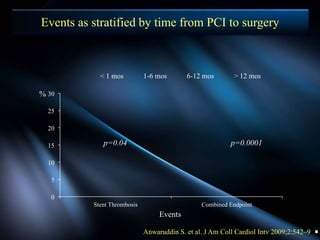
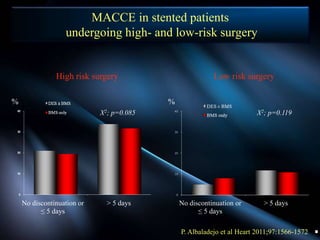
This document contains guidelines and proposals for operational models from GISE-ANMCO-SIAARTI on the topic of coronary stents and surgery. It includes a protocol, results from position papers, consensus documents, studies on risk stratification and perioperative management of antiplatelet therapy, as well as proposals for apps and regional guidelines. The key points are to maintain aspirin in most patients, postpone high risk surgery if possible, discontinue P2Y12 inhibitors after 6 months only for low risk PCI, and use bridging LMWH in selected high risk cases.