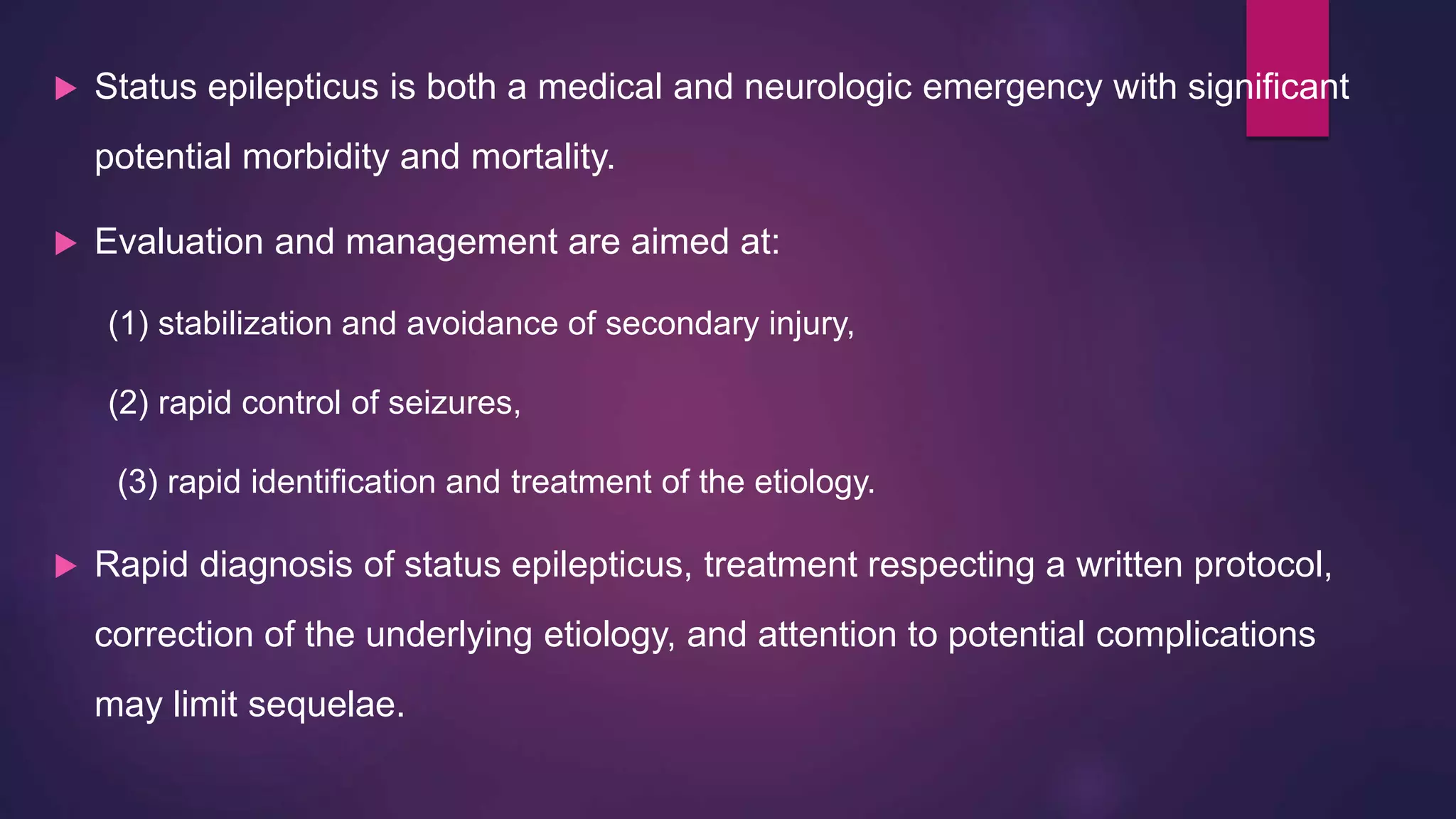
A 31-year-old male presented with a fever for one week and seizures and altered sensorium for three days. He experienced generalized tonic-clonic seizures that were initially uncontrolled. Imaging showed findings suggestive of viral or autoimmune encephalitis. Refractory status epilepticus was diagnosed and treated with high doses of multiple antiepileptic drugs, including lacosamide, which eventually controlled the seizures. Status epilepticus is defined as a seizure that persists for a sufficient length of time or is repeated frequently enough that recovery between attacks does not occur. The pathophysiology involves reductions in inhibitory GABA receptors and increases in excitatory glutamate receptors over time.

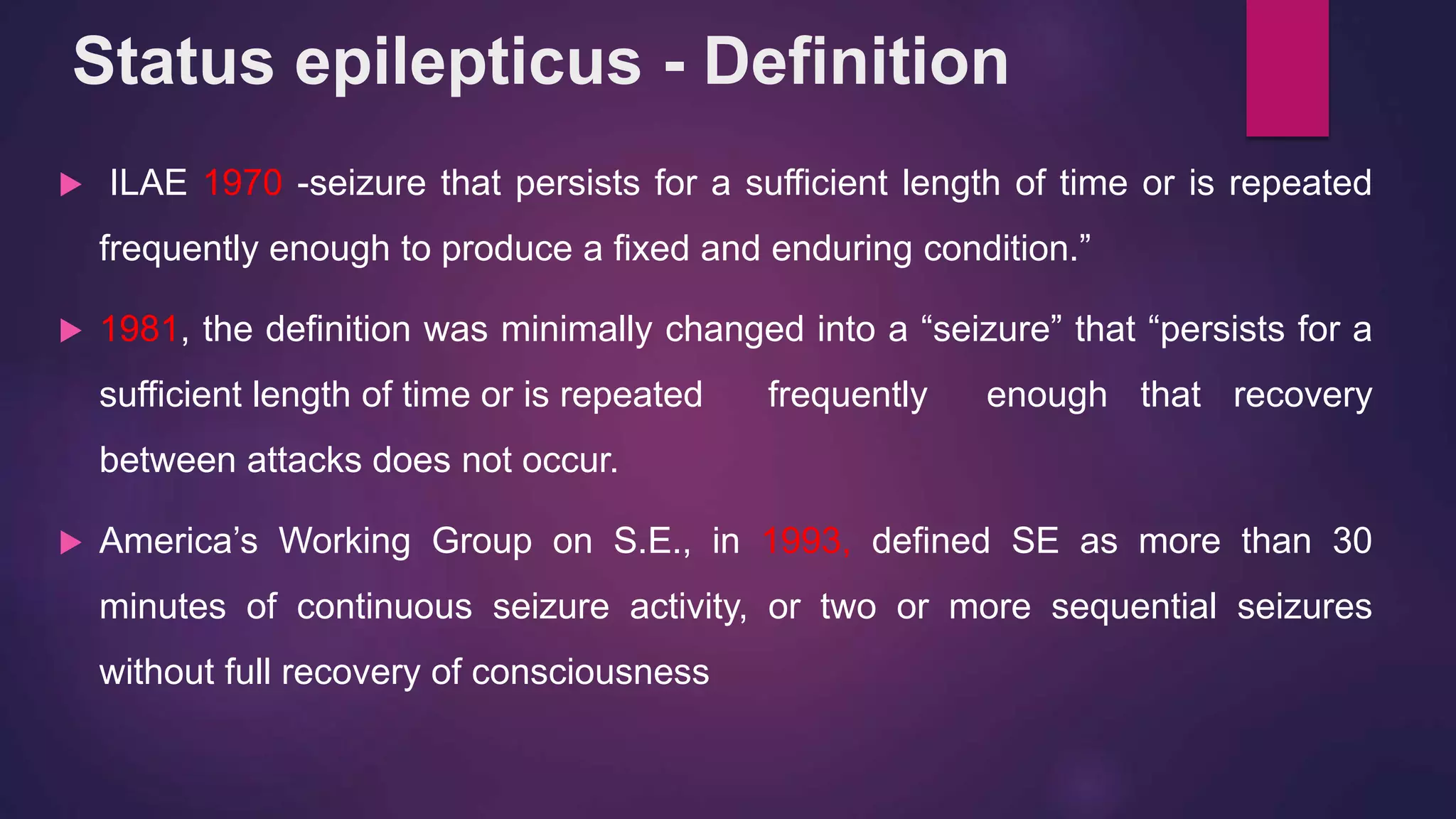
![The ILAE Core Group on Classification group suggested the
operational definition for SE in adults and children more than five years a)
Two or more discrete seizures without restoration of consciousness or
b) Seizure lasting for more than five minutes (patients > 5 years
conceptual definition,
“Generalized, convulsive status epilepticus refers to a condition in which there
is failure of the “normal” factors that serve to terminate a typical GTCS
[generalized tonic–clonic seizures].
Status epilepticus - Definition](https://image.slidesharecdn.com/sunithaepilepsyfinal-190918094917/75/status-epilepticus-presentation-8-2048.jpg)