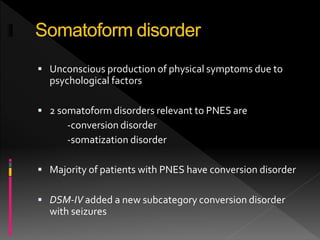
This document discusses psychogenic nonepileptic seizures (PNES). PNES are characterized by sudden disturbances in motor, sensory, cognitive or emotional functioning that mimic epileptic seizures but are caused by psychological factors rather than abnormal brain activity. The diagnosis of PNES is challenging and often delayed due to the diversity of presentations. Video EEG monitoring is the gold standard for diagnosis and should be performed when PNES is suspected to rule out epilepsy. Treatment involves delivering the diagnosis to patients and managing any underlying psychiatric conditions, usually through psychotherapy. Prognosis depends on factors like duration of illness, motivation for treatment and management of comorbid psychological issues.