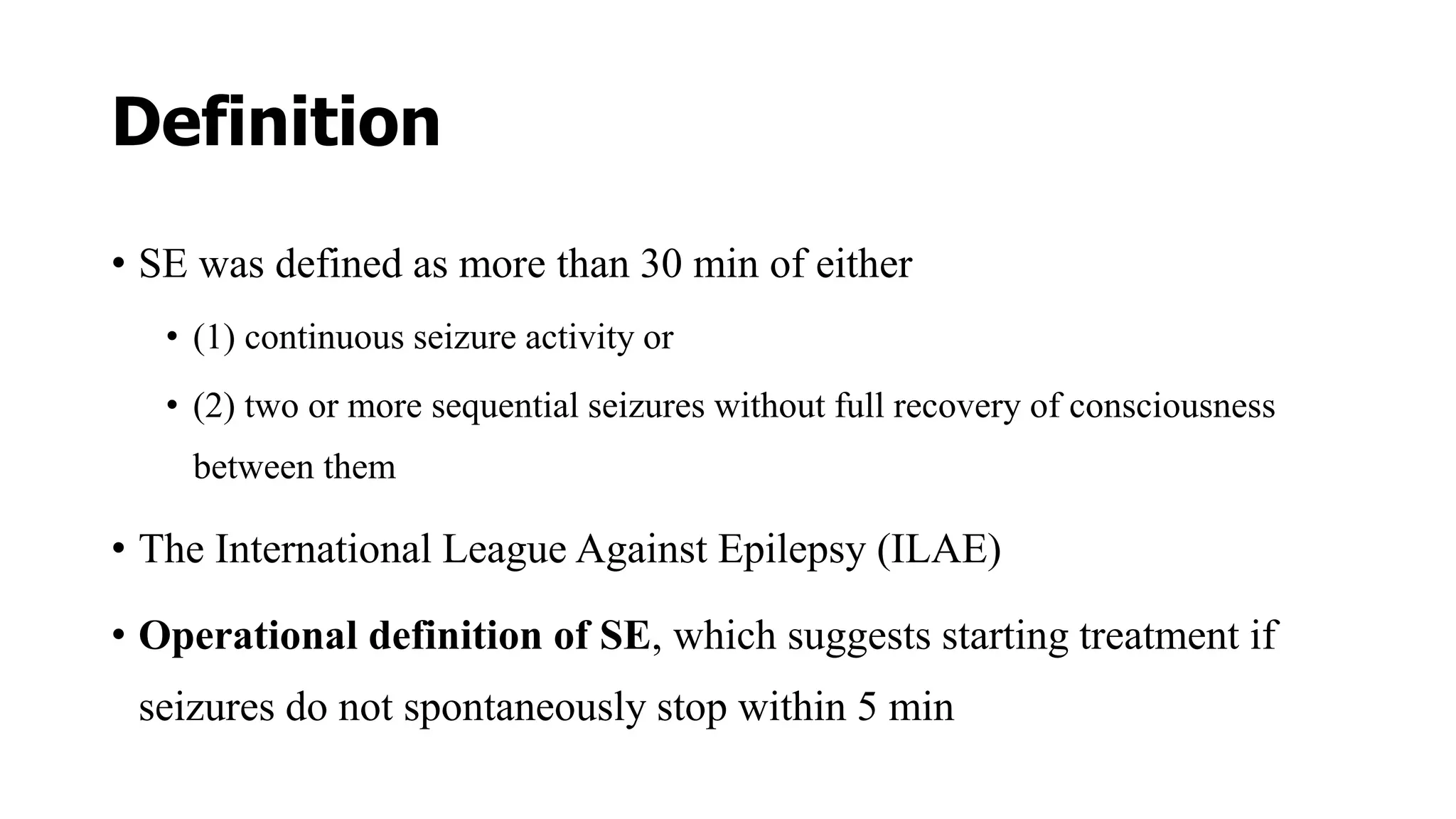
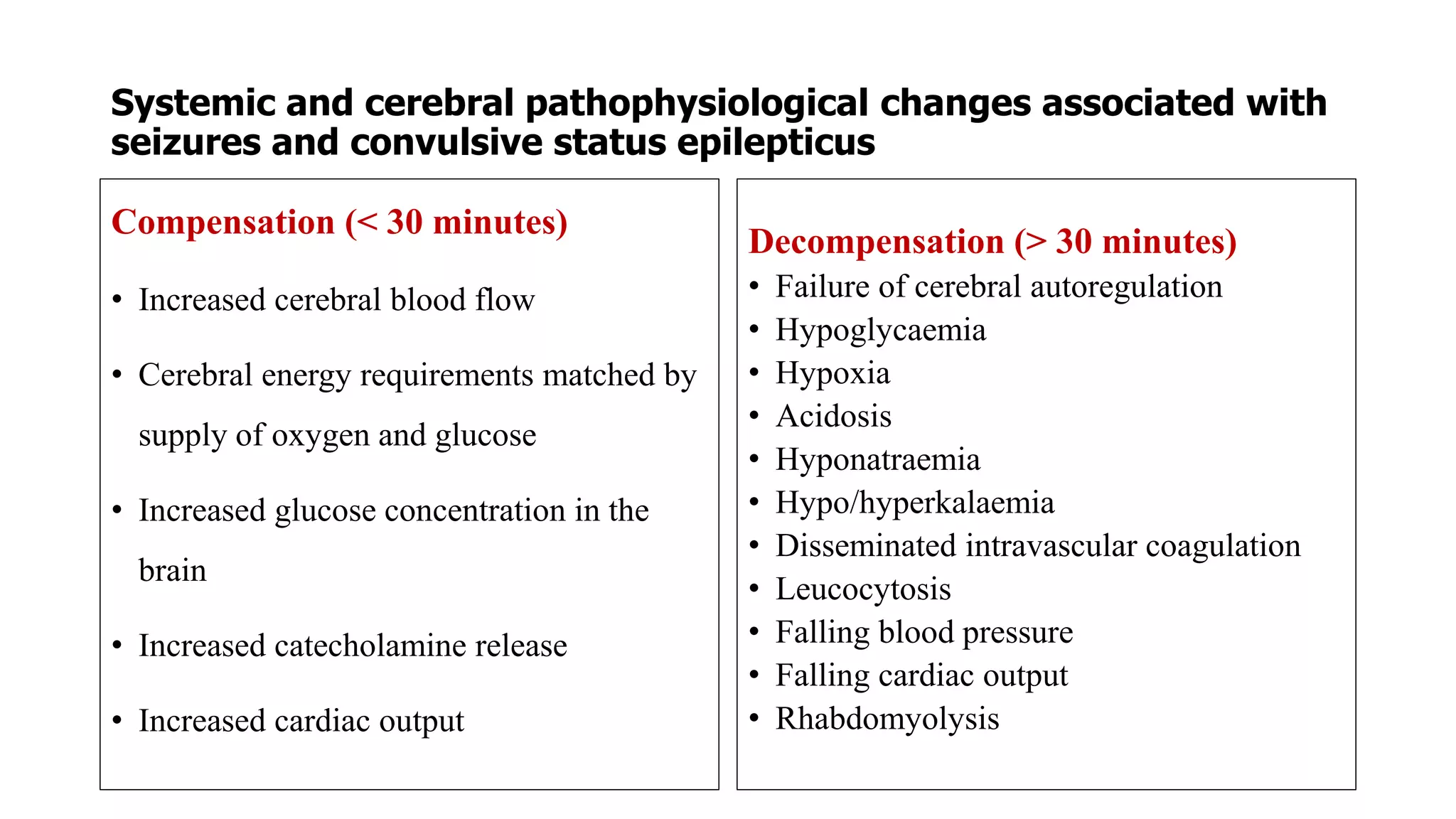
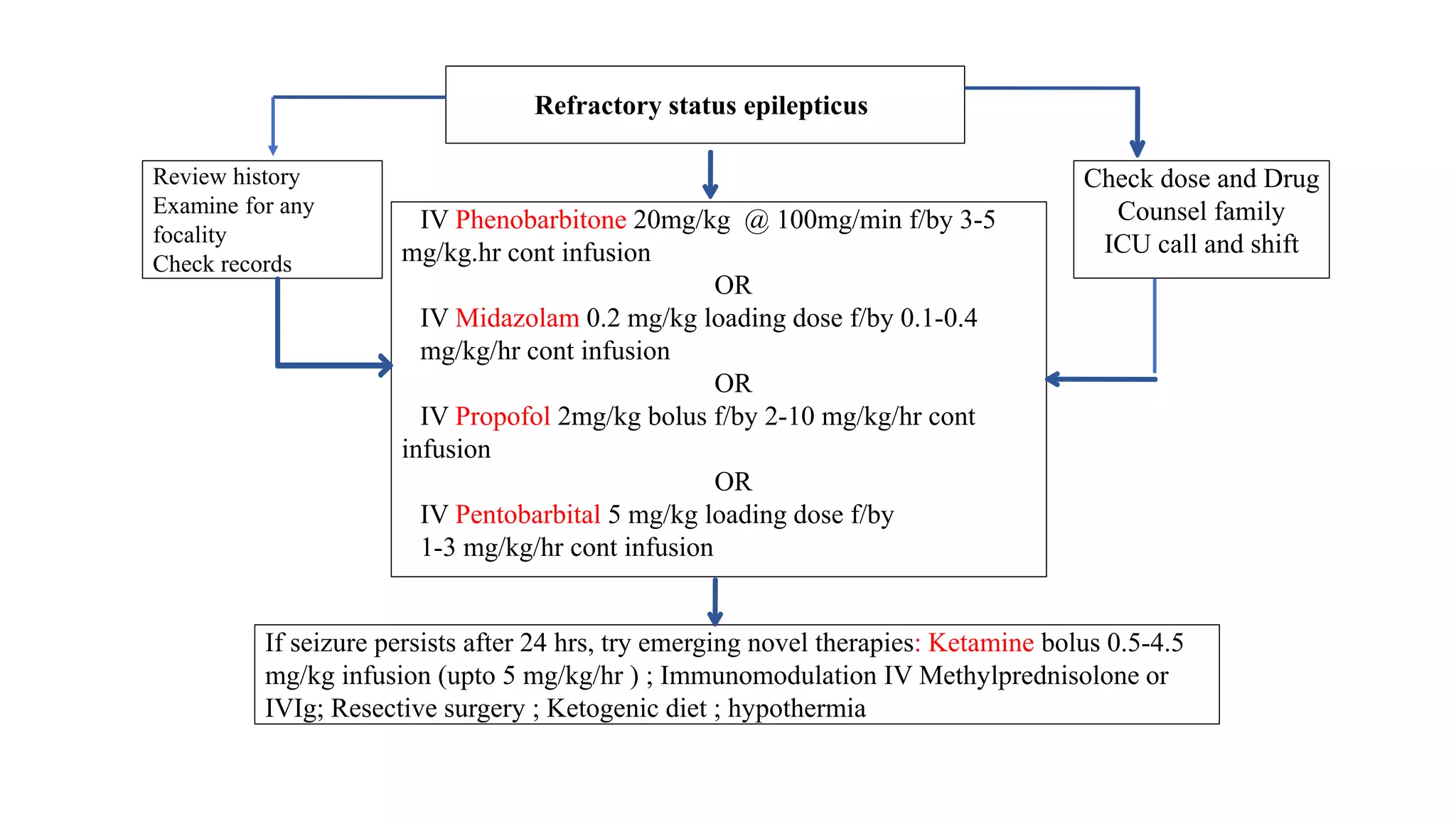
Status epilepticus (SE) refers to prolonged or repeated seizures without recovery between seizures. It is a medical emergency associated with high morbidity and mortality if not treated promptly. The initial treatment for SE involves benzodiazepines like lorazepam or diazepam. If seizures continue, second line drugs like fosphenytoin or valproate are used. For refractory SE, anesthetic drugs like midazolam, propofol or pentobarbital may be needed. Timely treatment is important to prevent neuronal injury, with outcomes worsening the longer seizures continue untreated.