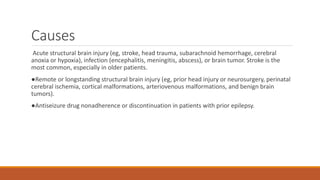
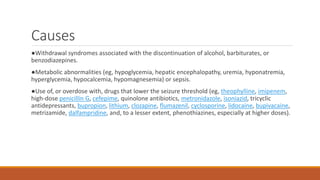
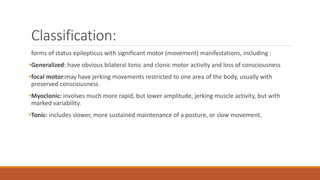
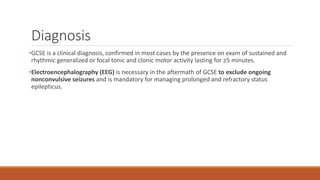
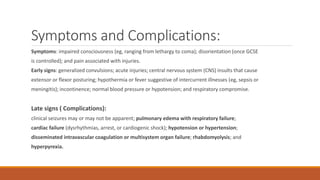
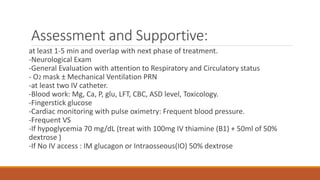
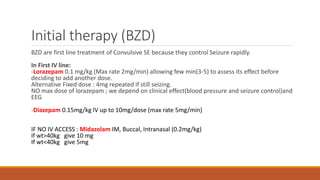
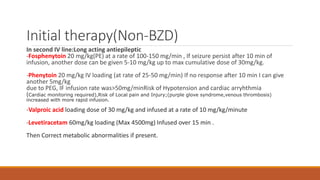
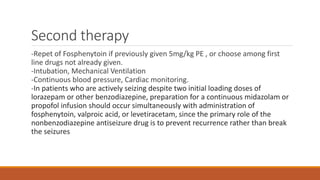
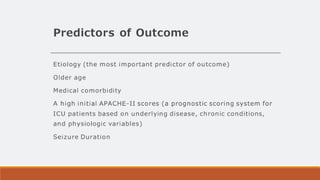
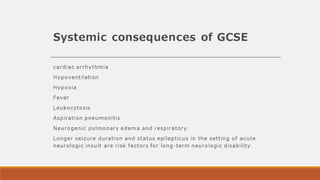
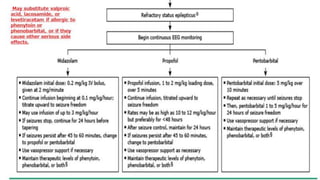
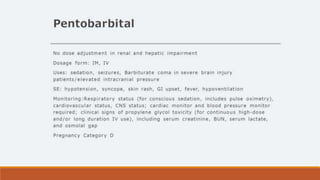
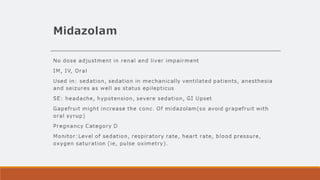
Status epilepticus is a medical emergency characterized by continuous seizures for ≥5 minutes or ≥2 discrete seizures without recovery of consciousness. It can be caused by various factors including acute brain injuries, infections, drug withdrawal, and metabolic abnormalities, with treatment starting promptly after a few minutes of seizure activity. Management includes immediate benzodiazepines, potential intubation and ventilation, and the use of long-acting antiepileptic drugs for long-term control.