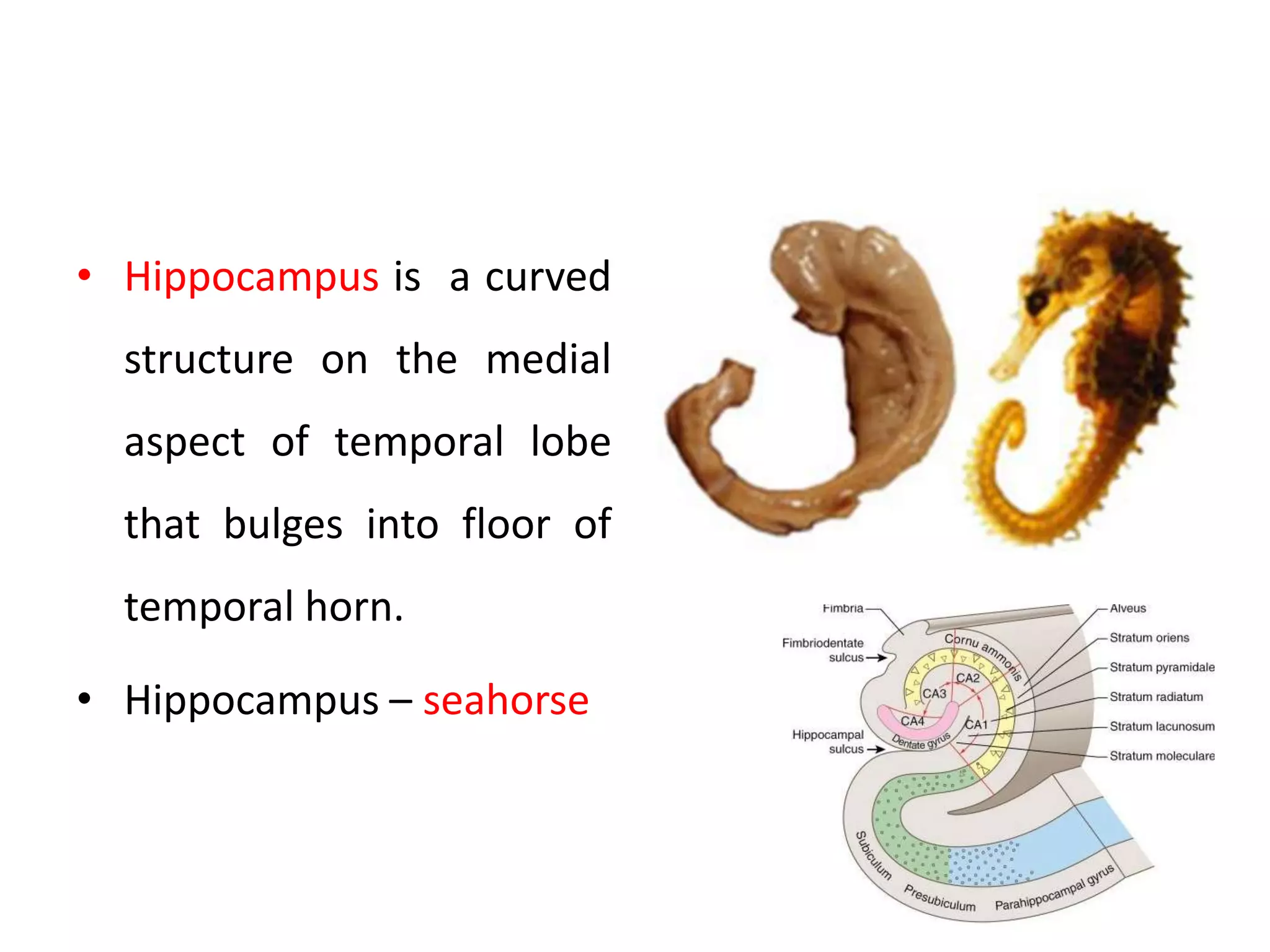
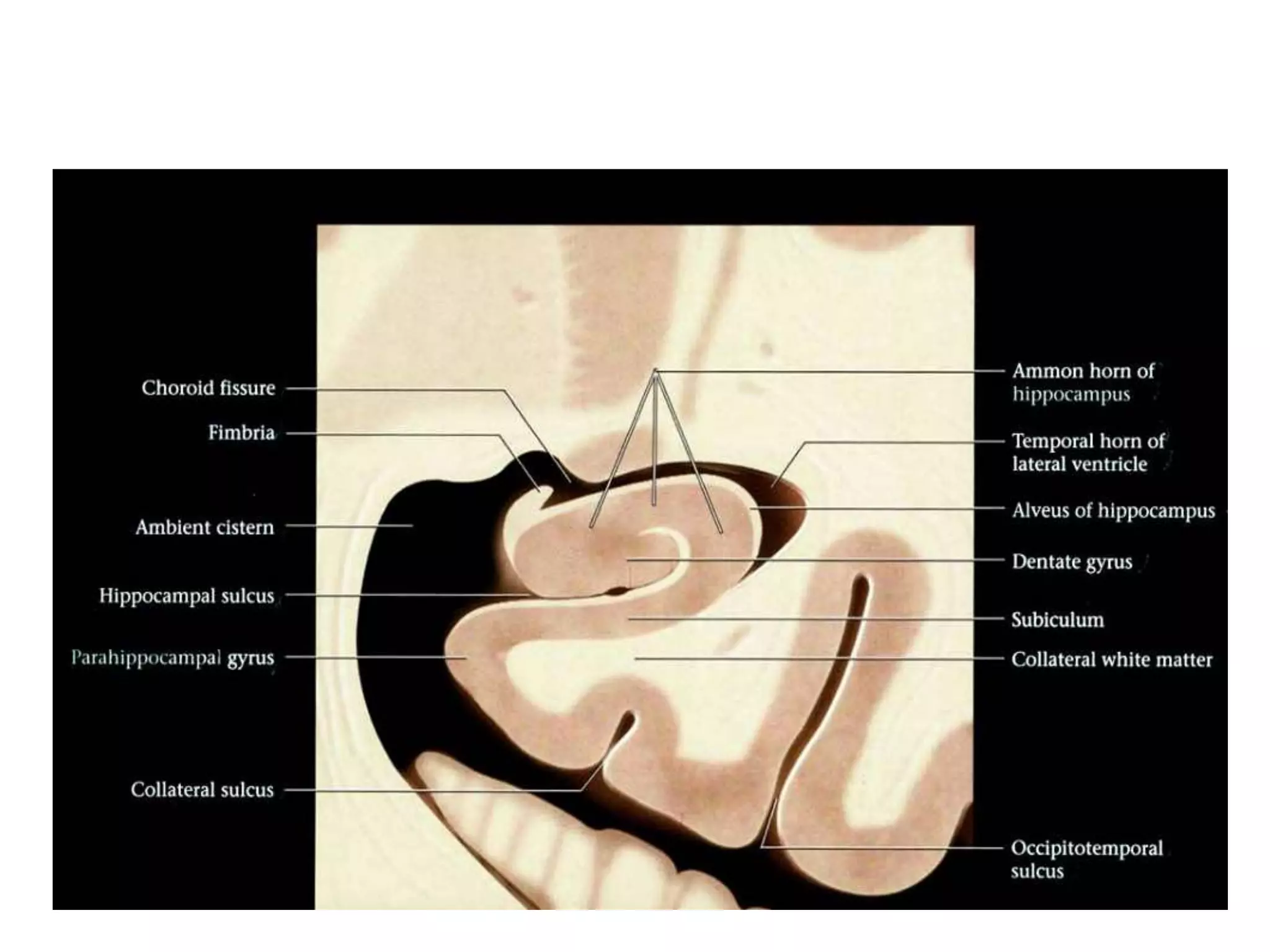
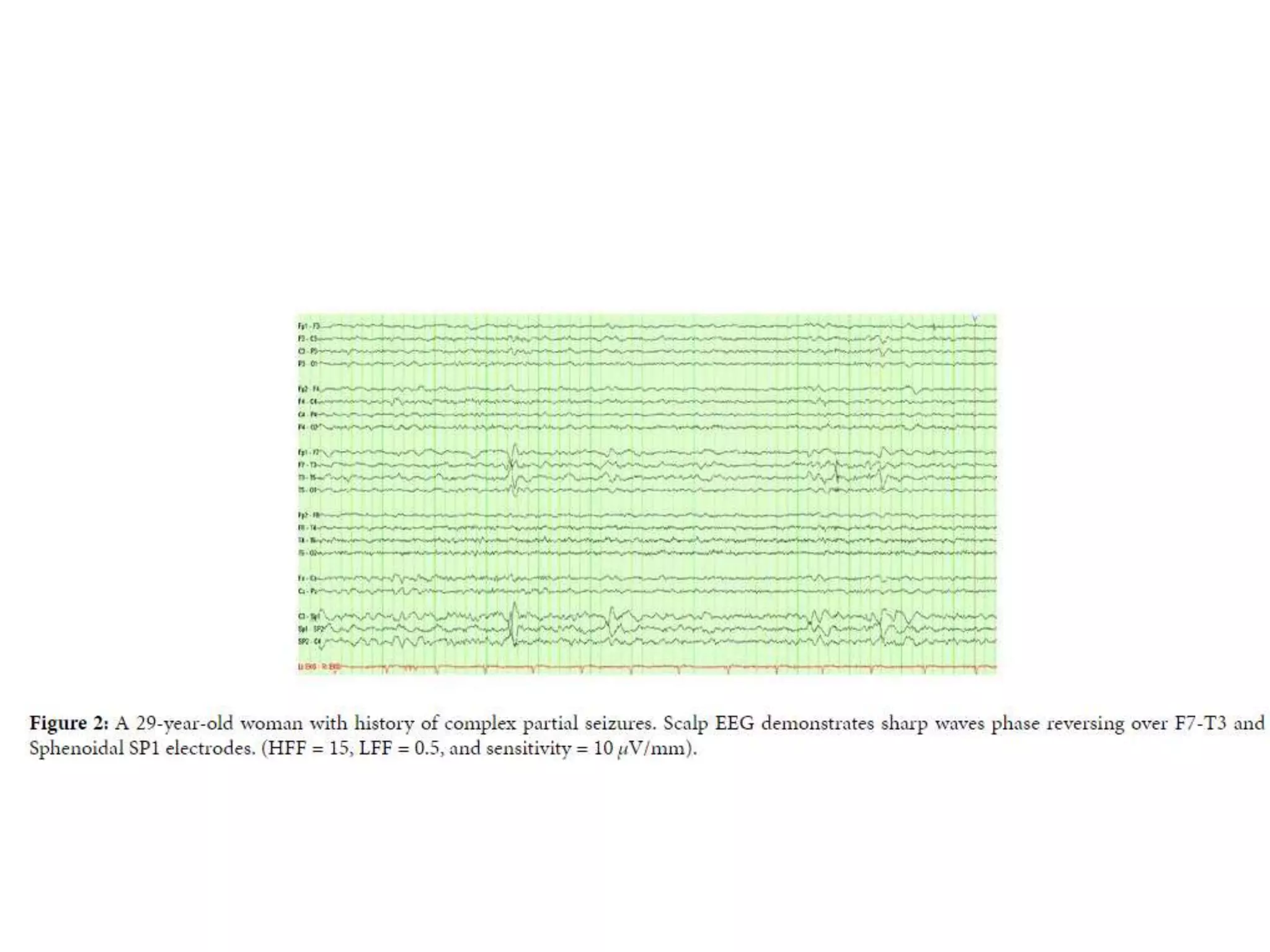
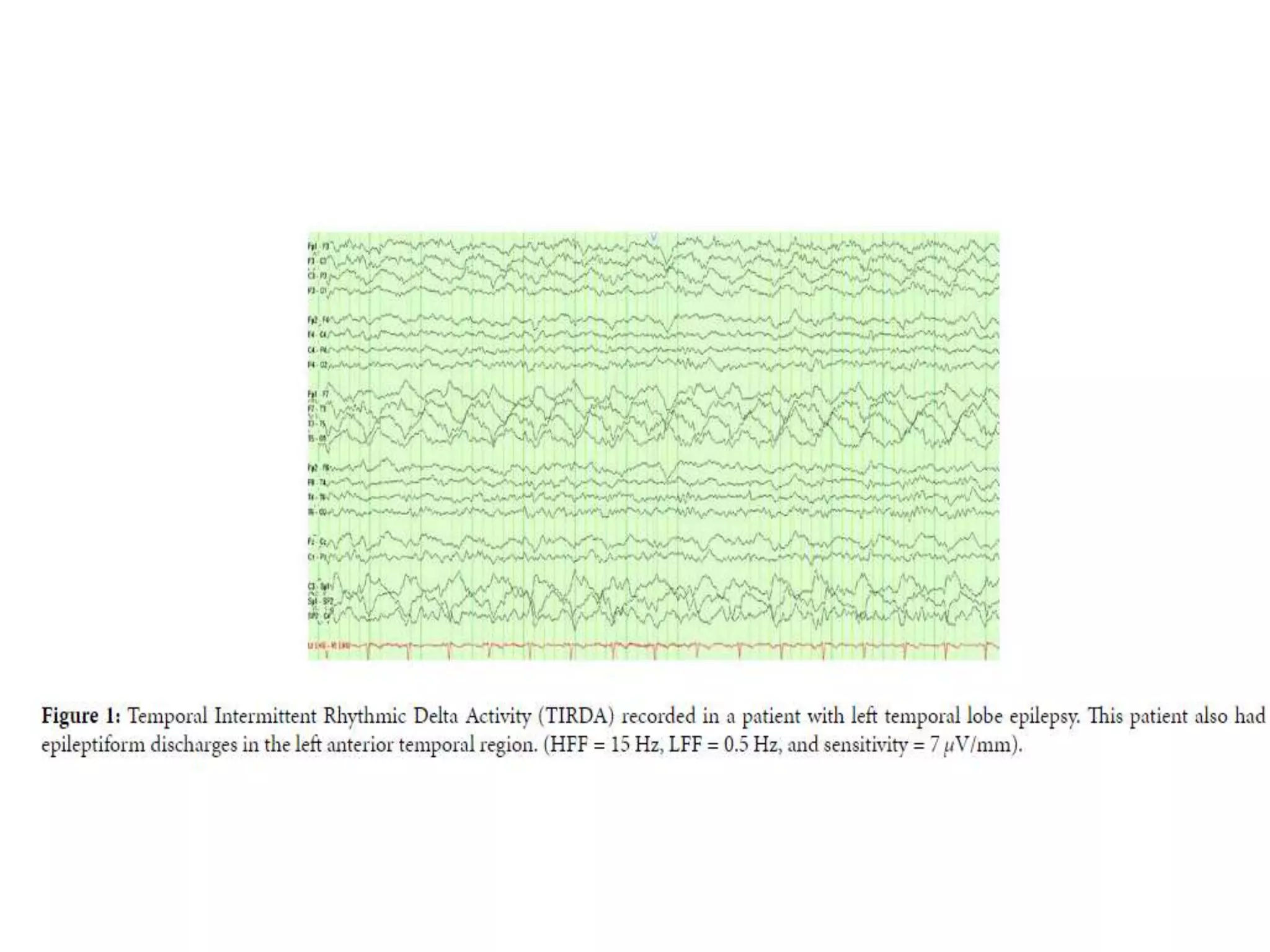
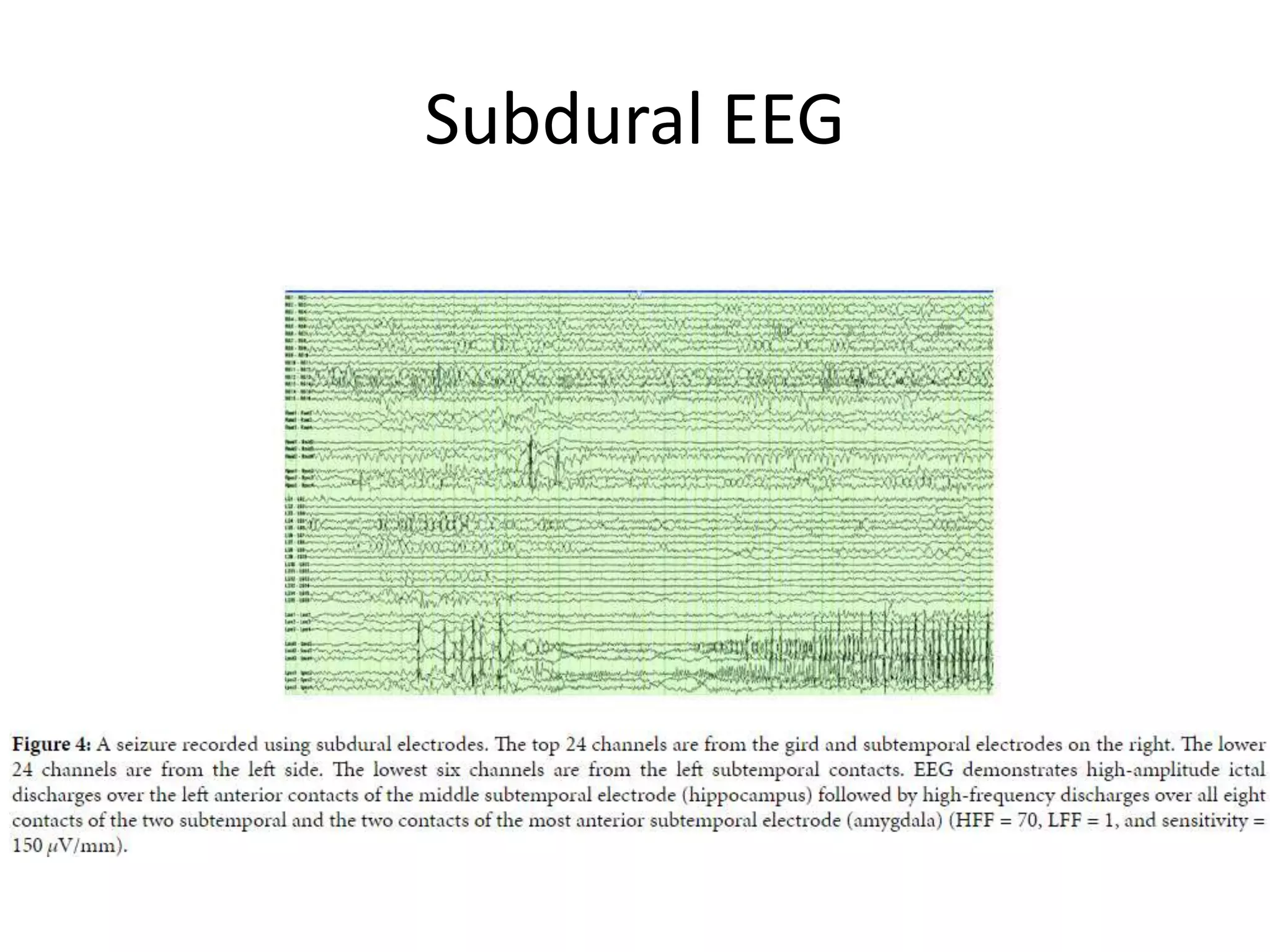
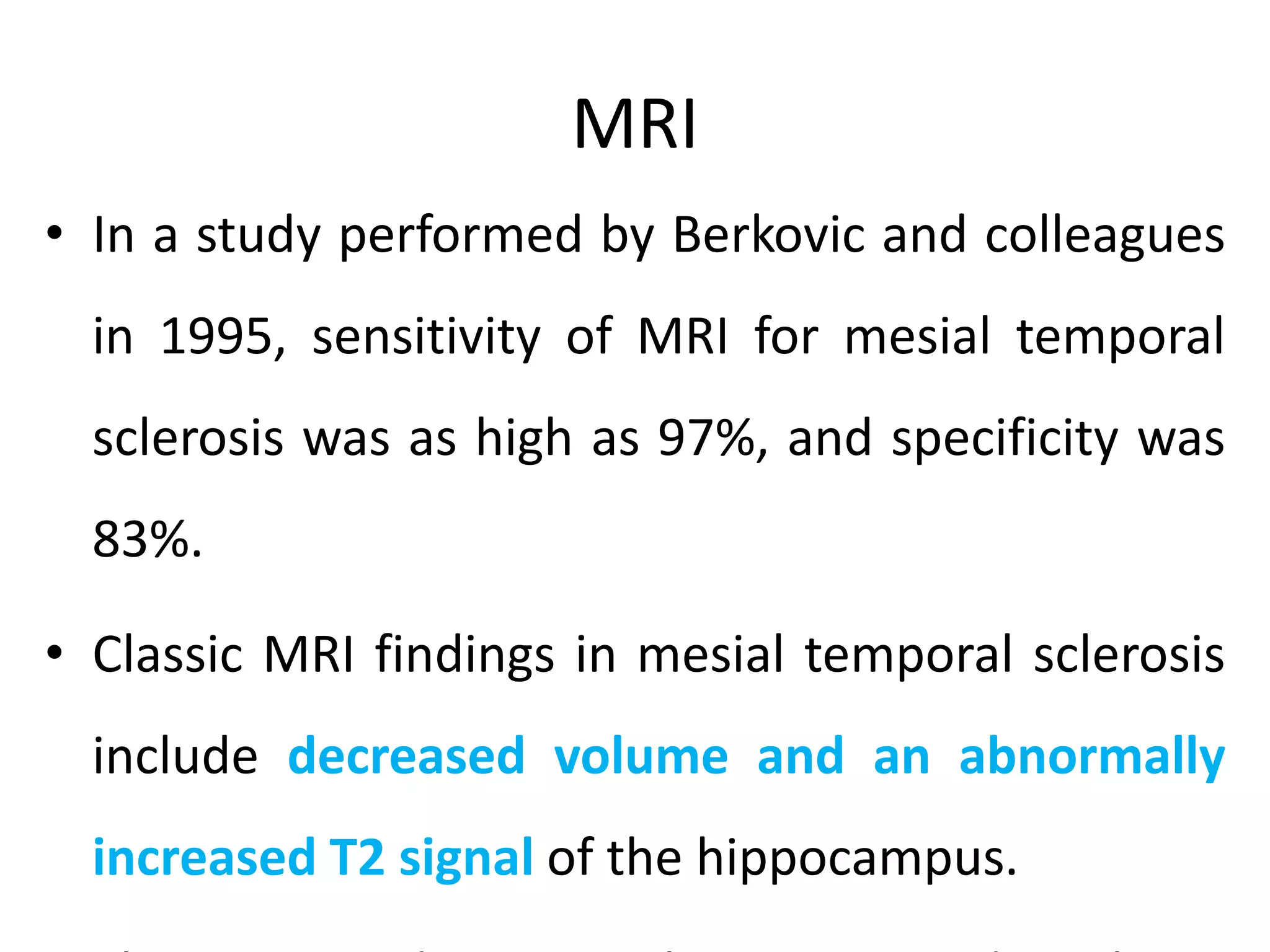
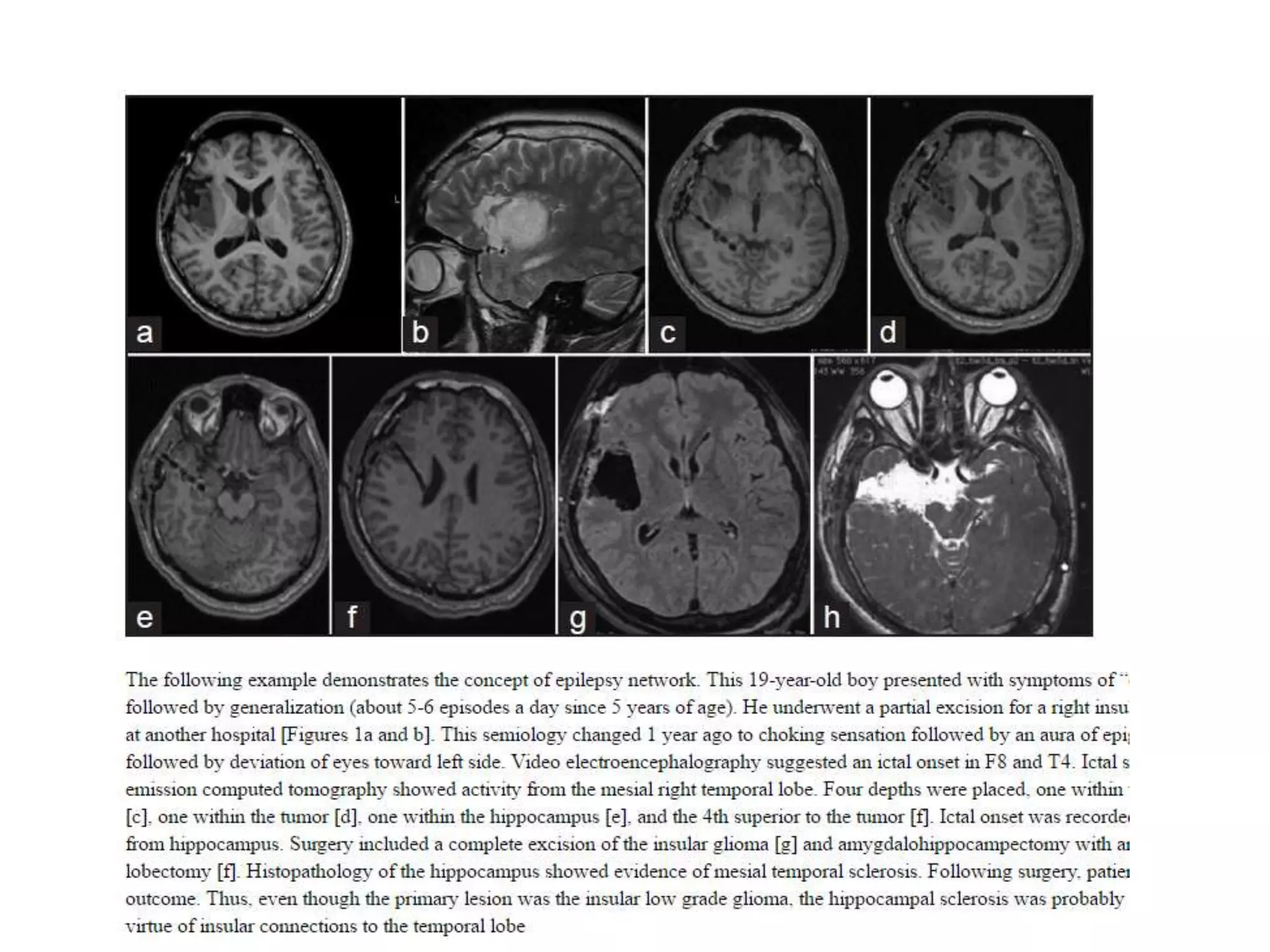
Mesial temporal lobe epilepsy involves seizures originating in the mesial temporal lobe structures like the hippocampus and amygdala. Key features of mesial temporal lobe epilepsy include focal seizures with impaired awareness that involve automatisms and psychic symptoms. Diagnosis involves EEGs that may show interictal temporal sharp waves, spikes or slow waves as well as postictal changes that can lateralize the seizure onset. Resection of the epileptogenic mesial temporal lobe structures is an effective treatment for drug-resistant mesial temporal lobe epilepsy.