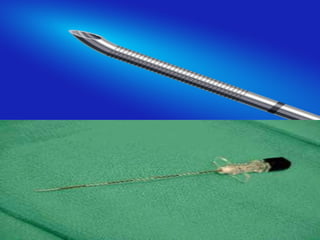
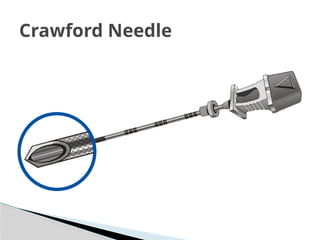
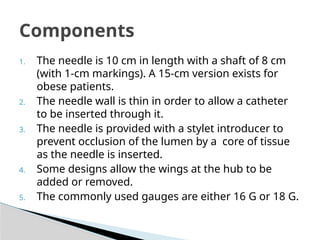
The document details the characteristics and uses of epidural needles, primarily the Tuohy and Crawford needles, along with their mechanisms, components, and safety features. It emphasizes the significance of proper catheter placement and the risks associated with accidental dural puncture. Additionally, it discusses the design of epidural kits, including features of catheters and filters used to ensure effective and safe epidural anesthesia.