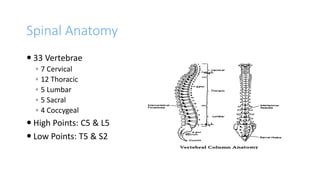
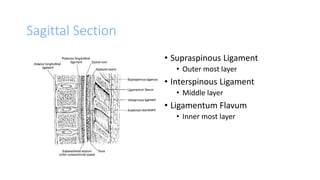
This document provides an overview of epidural anesthesia, including spinal anatomy, the epidural space, techniques for administering epidural anesthesia, indications and contraindications. Key points include:
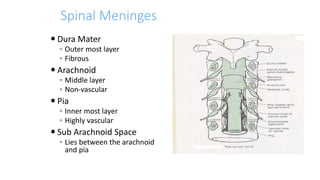
- Epidural anesthesia involves injecting anesthetic into the epidural space surrounding the spinal meninges.
- The epidural space is located using the loss of resistance technique, then a test dose is administered before further doses. An epidural catheter may be inserted.
- Epidural anesthesia can be used for surgeries involving the abdomen, thorax or neck. It provides postoperative and chronic pain management. Contraindications include increased intracranial pressure and coagulopathies. Complications include failed or high