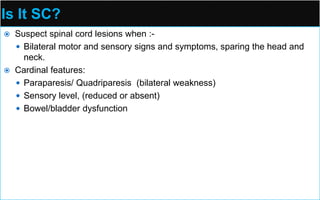
This document provides an overview of spinal cord anatomy and clinical assessment of spinal cord lesions. Key points include:
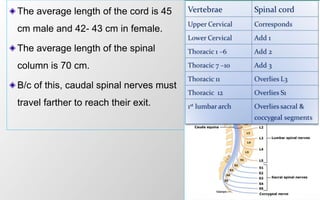
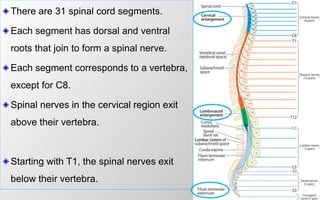
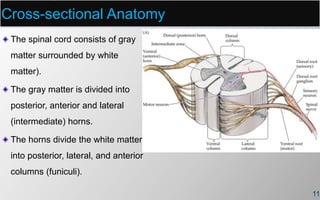
- The spinal cord extends from the foramen magnum to L1-L2 and is segmented into 31 pairs of spinal nerves.
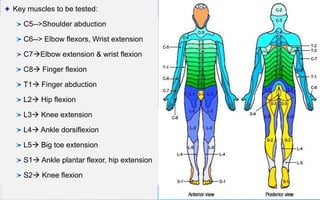
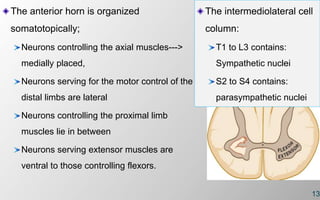
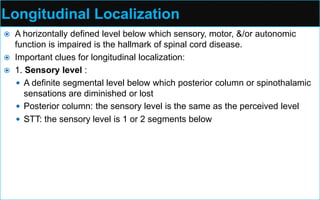
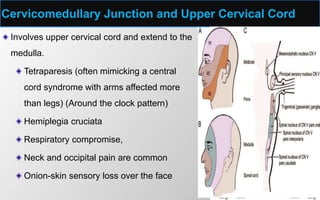
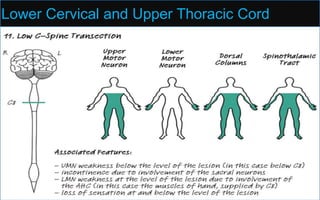
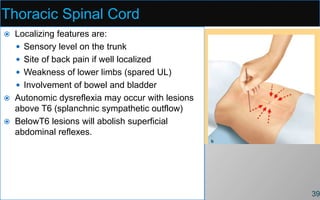
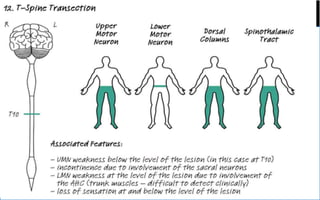
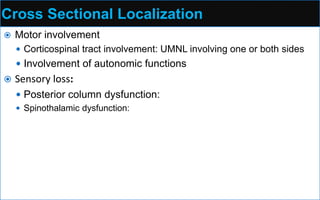
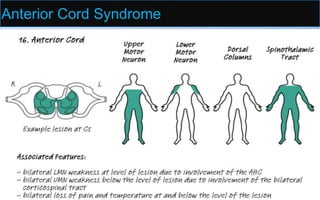
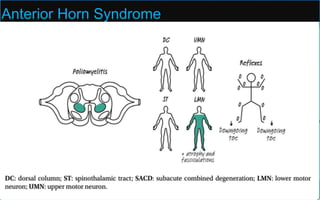
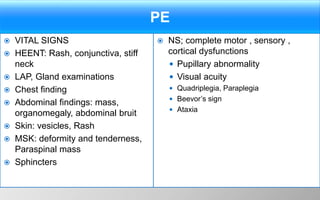
- Sensory and motor function can be localized based on dermatome and myotome patterns.
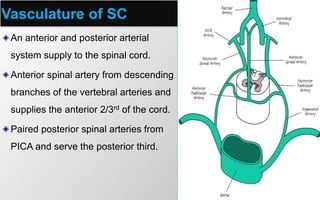
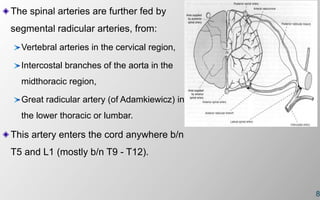
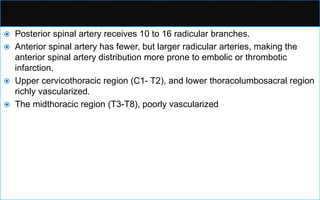
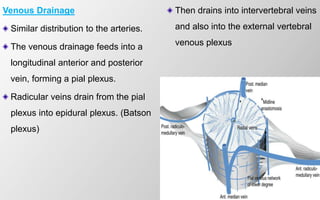
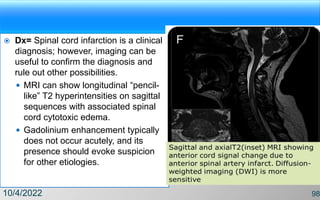
- Spinal cord blood supply comes from the anterior and posterior spinal arteries. The artery of Adamkiewicz is a critical radicular artery.
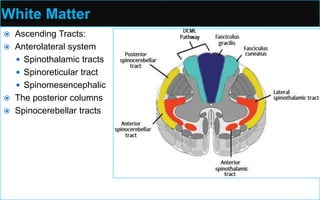
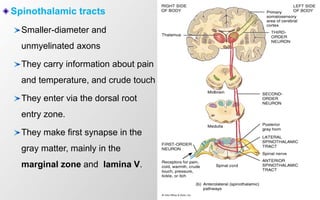
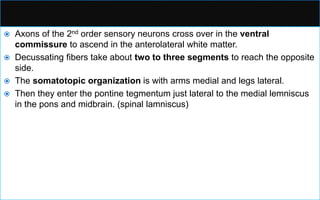
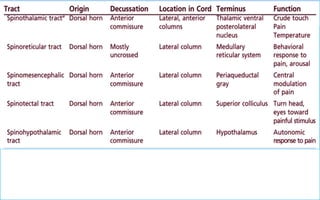
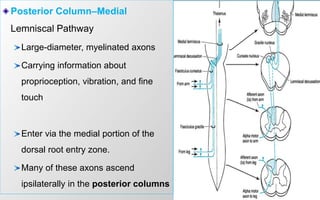
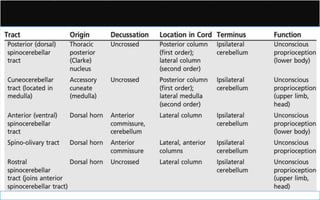
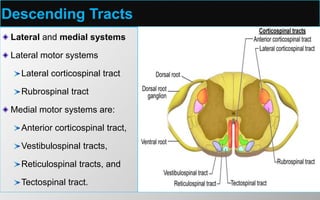
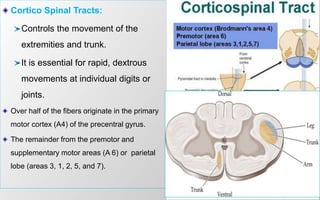
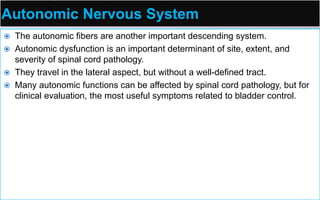
- Ascending tracts include the spinothalamic, posterior, and spinocerebellar tracts. Descending tracts include the corticospinal, rubrospinal, and reticulosp