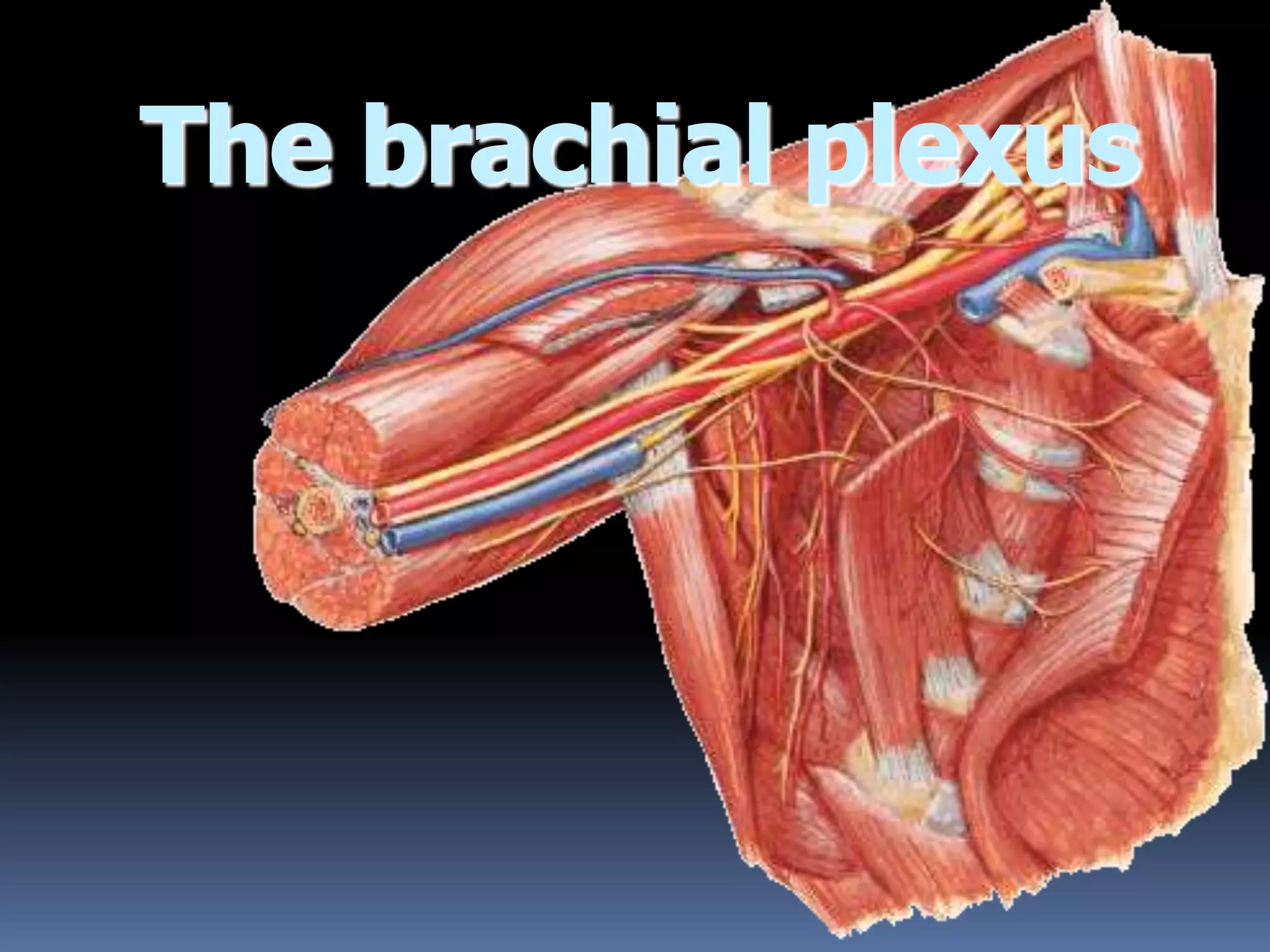
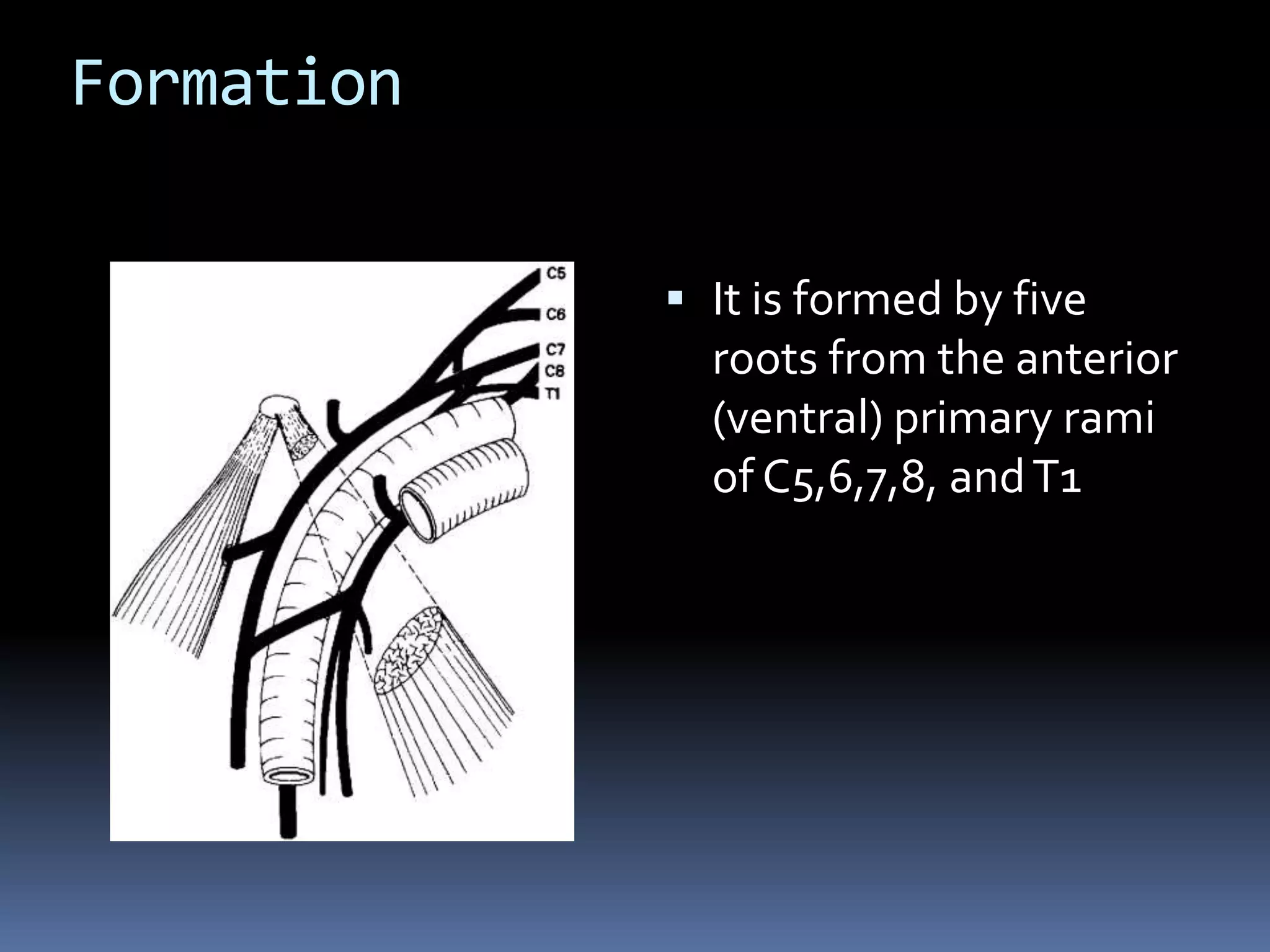
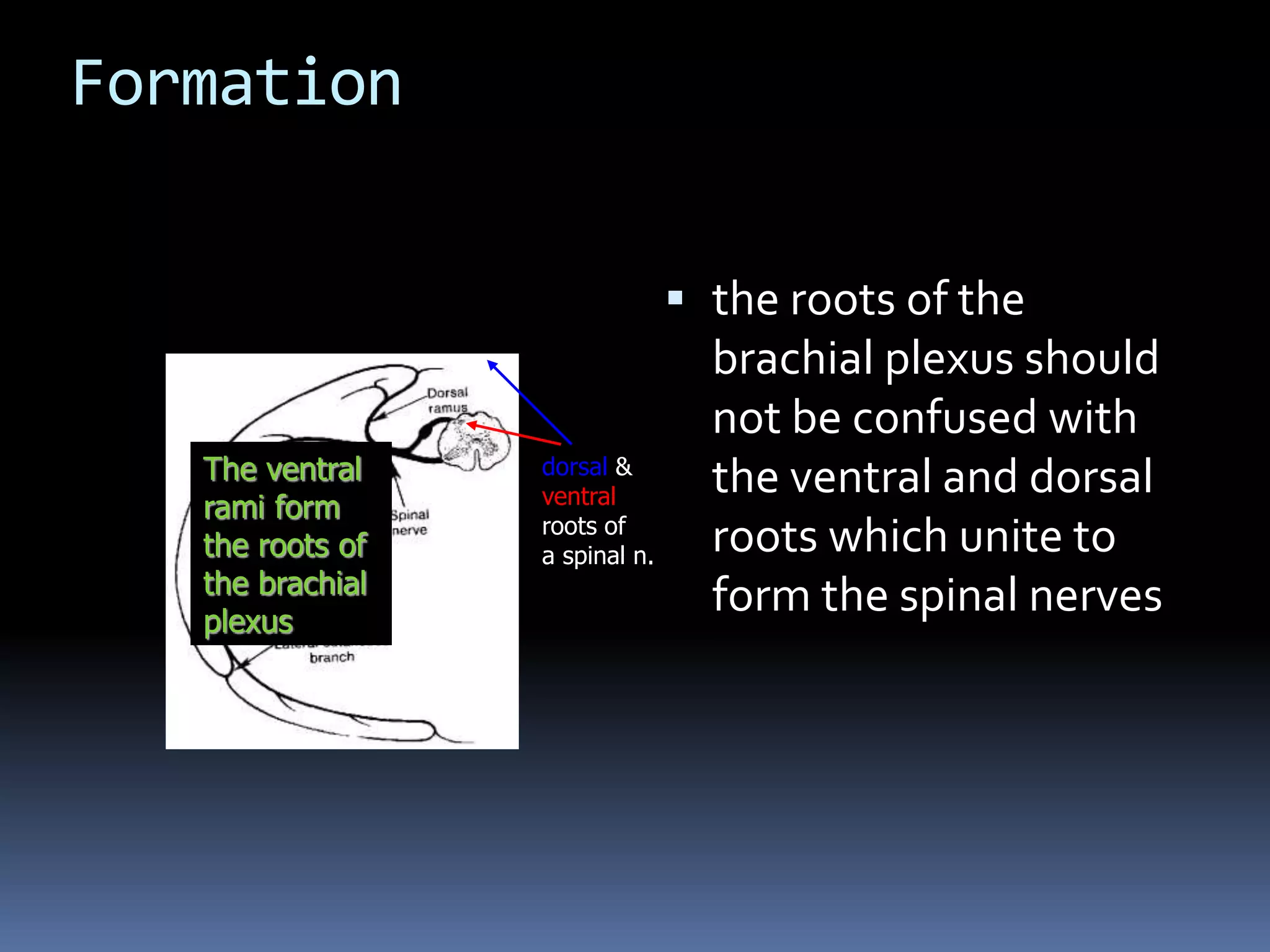
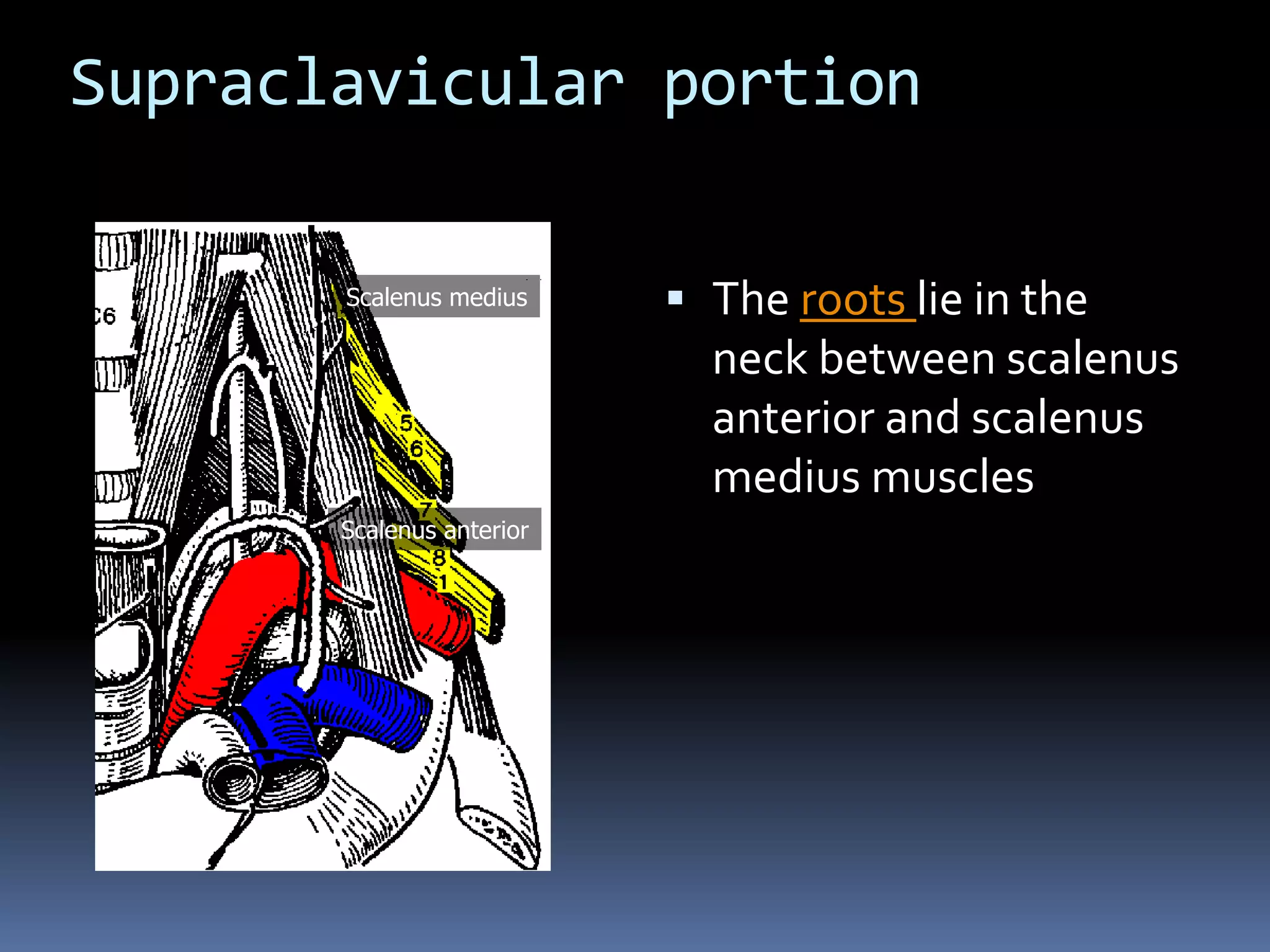
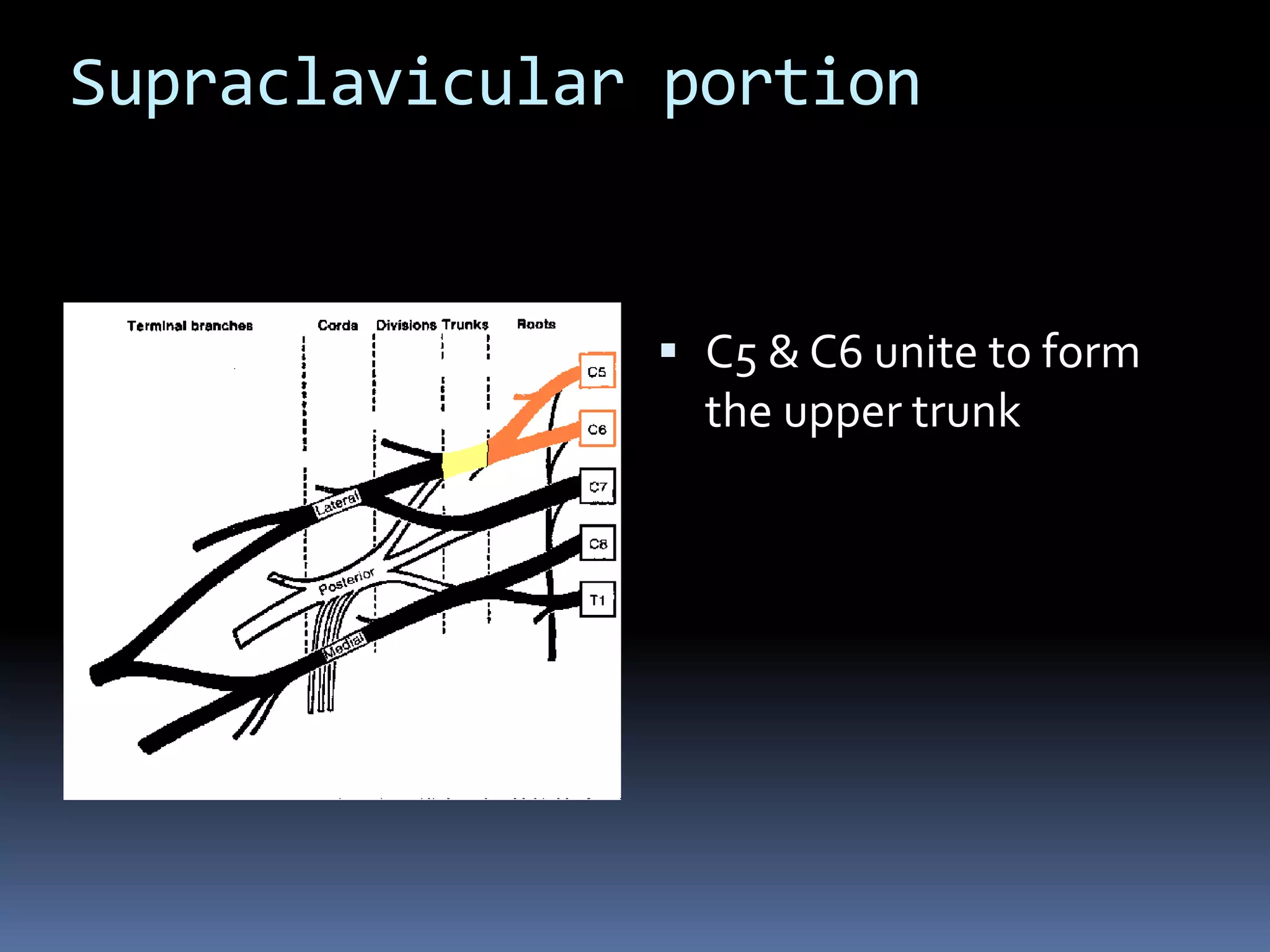
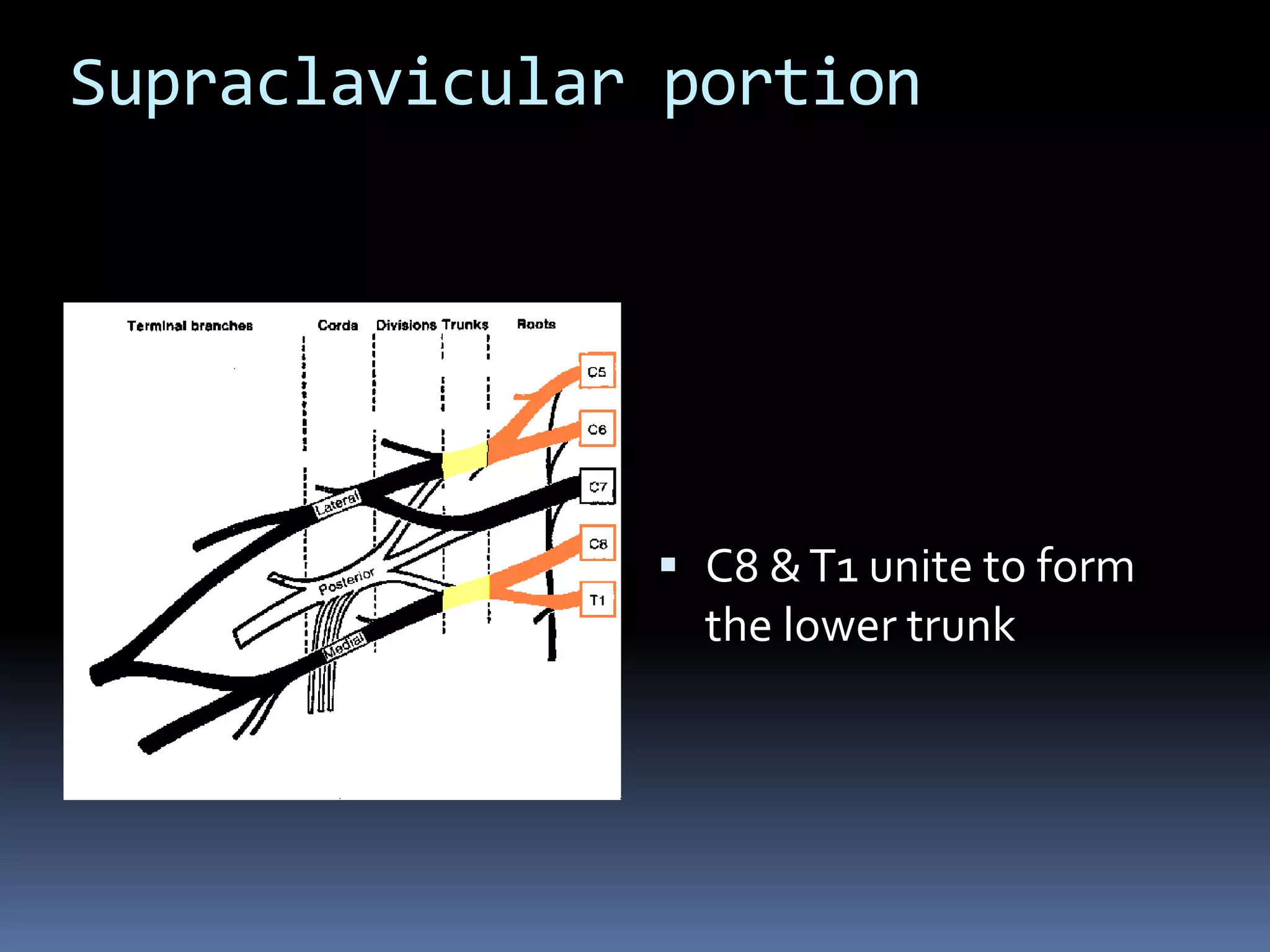
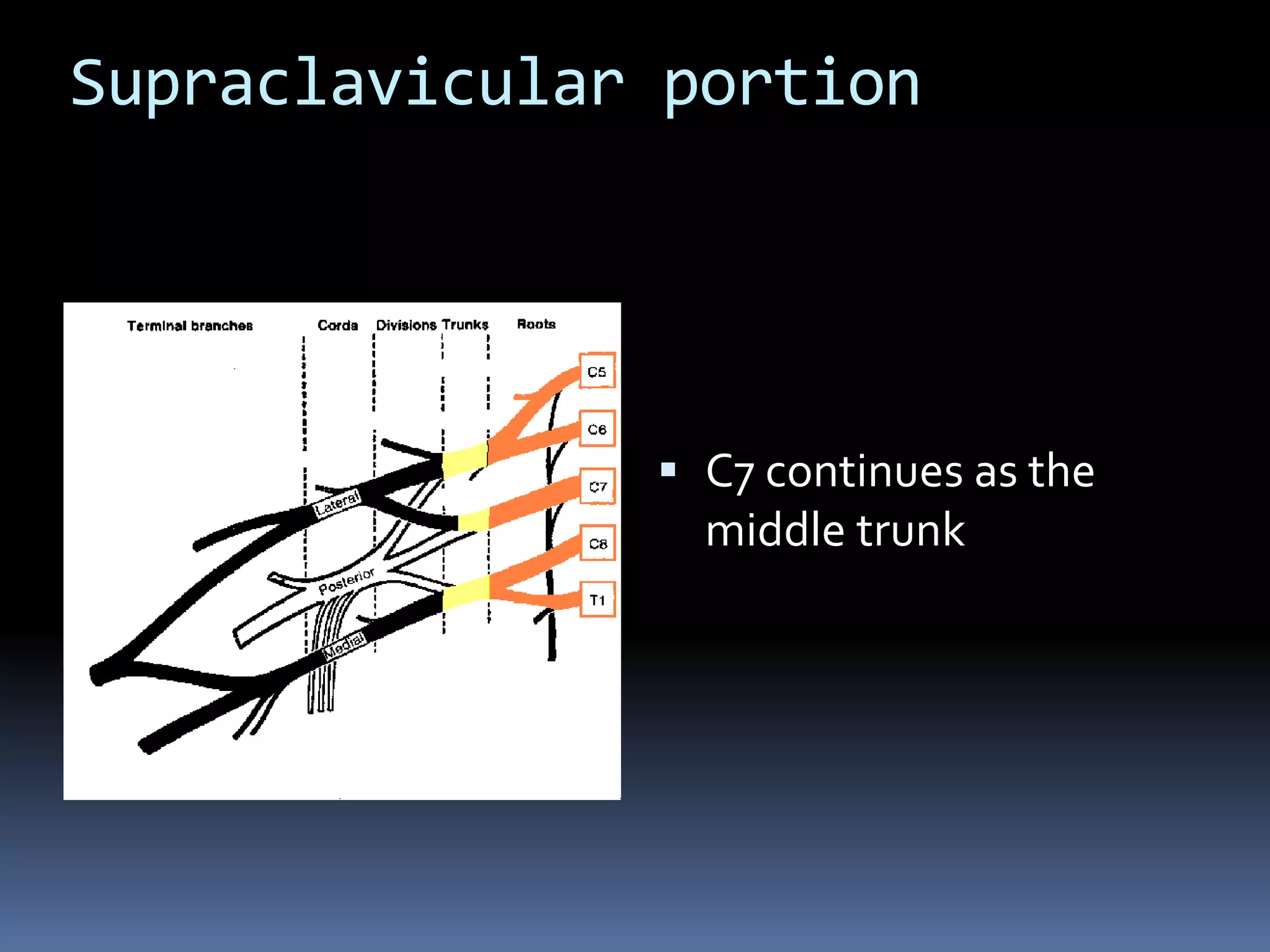
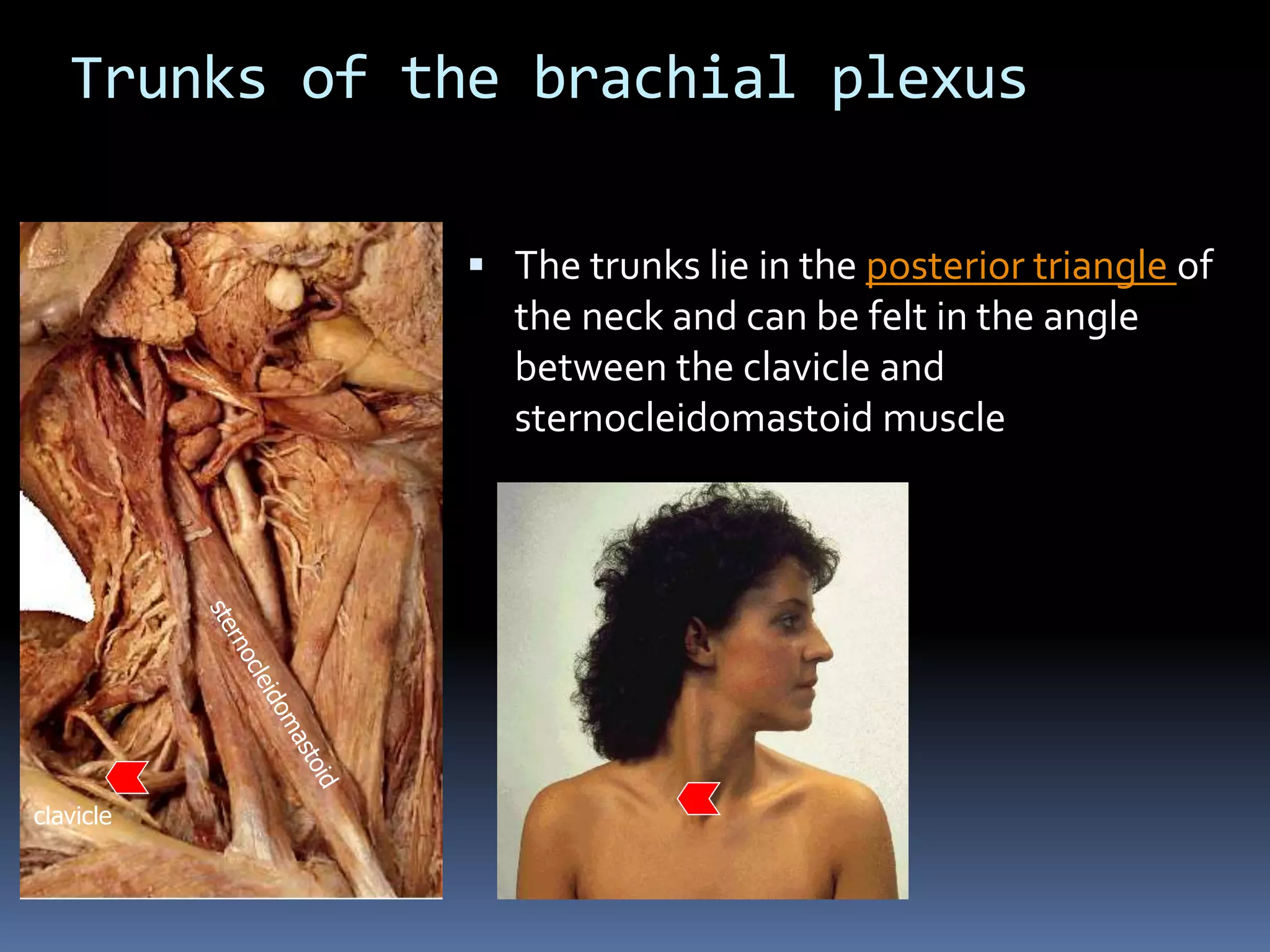
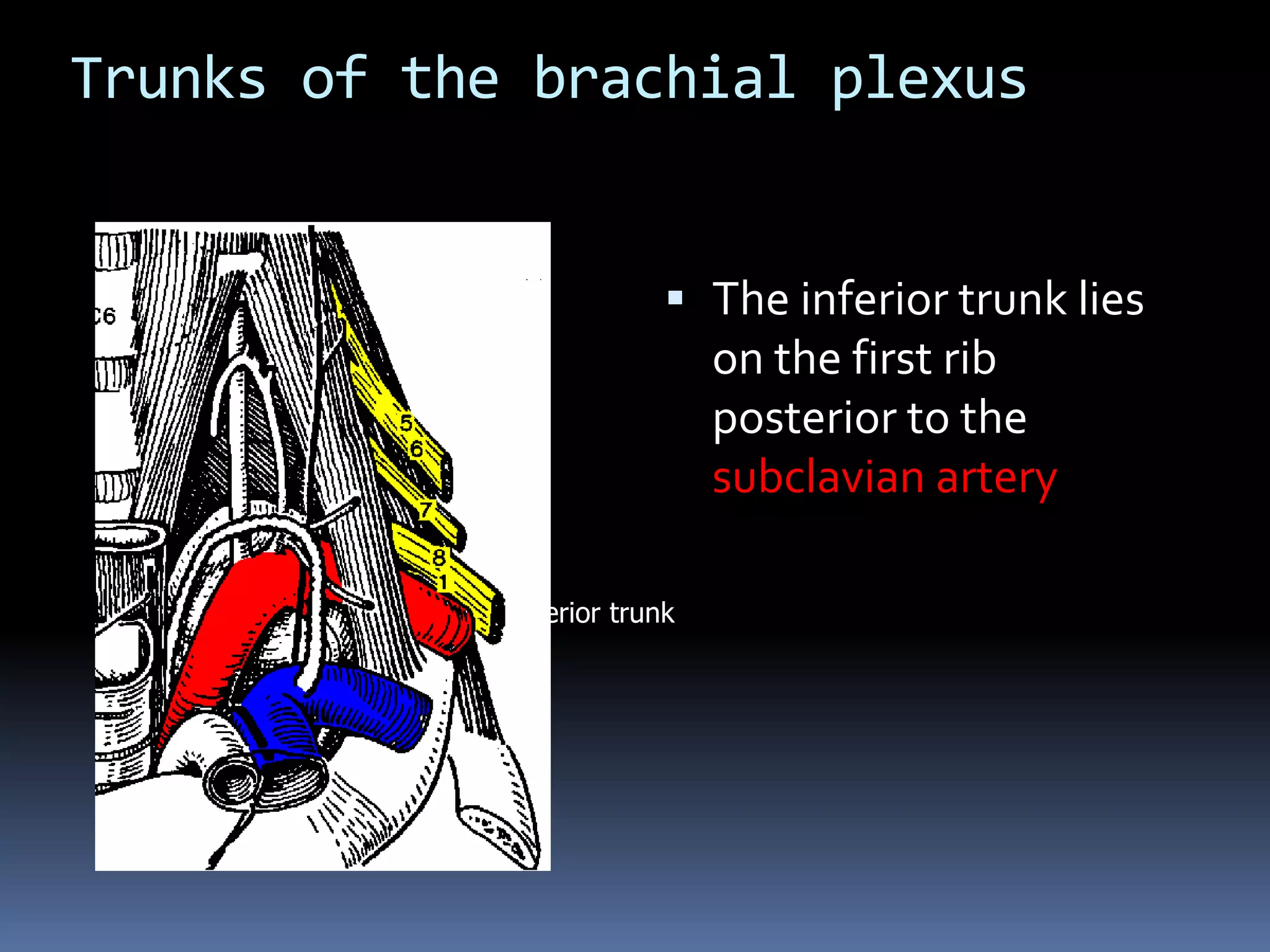
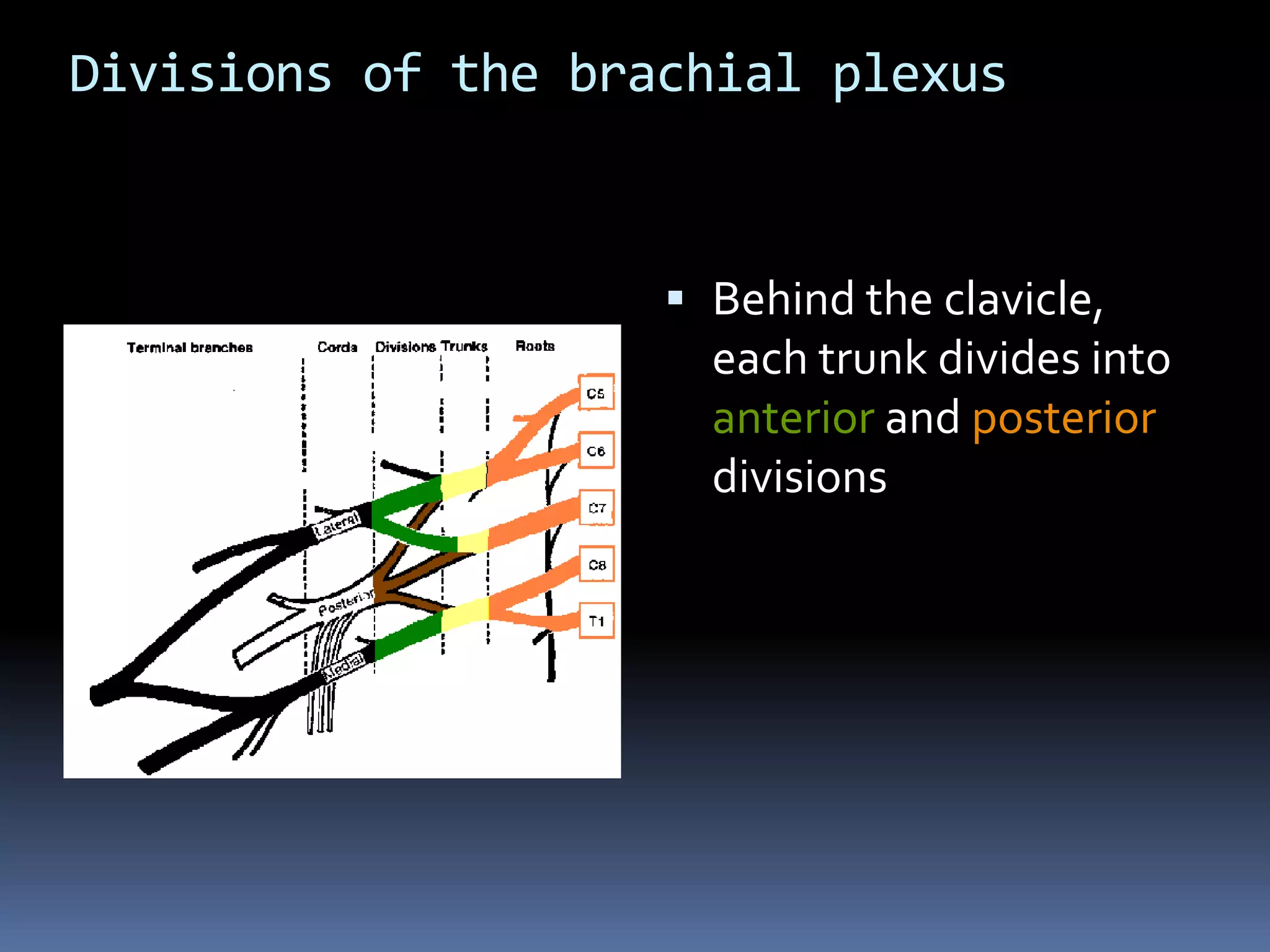
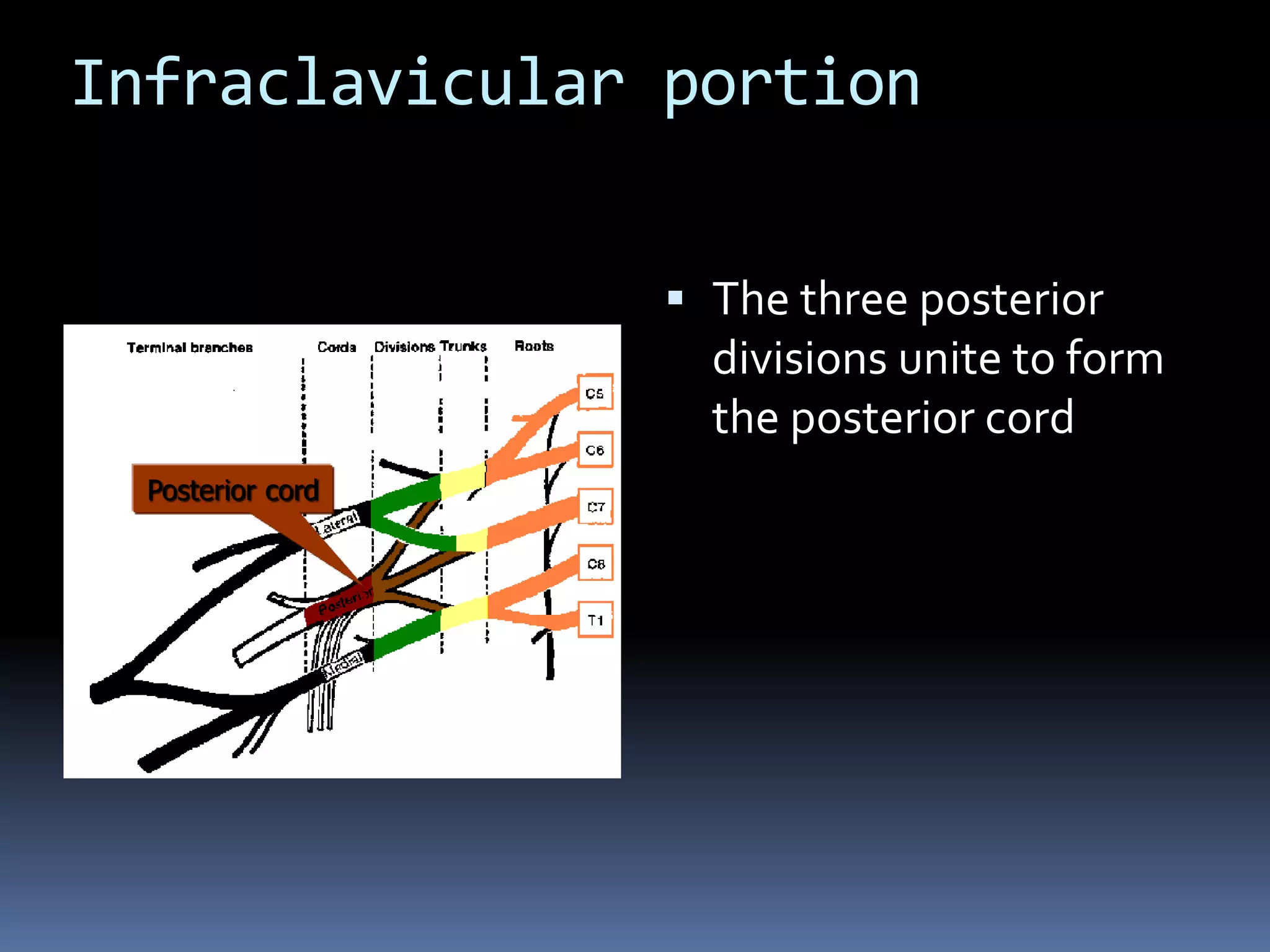
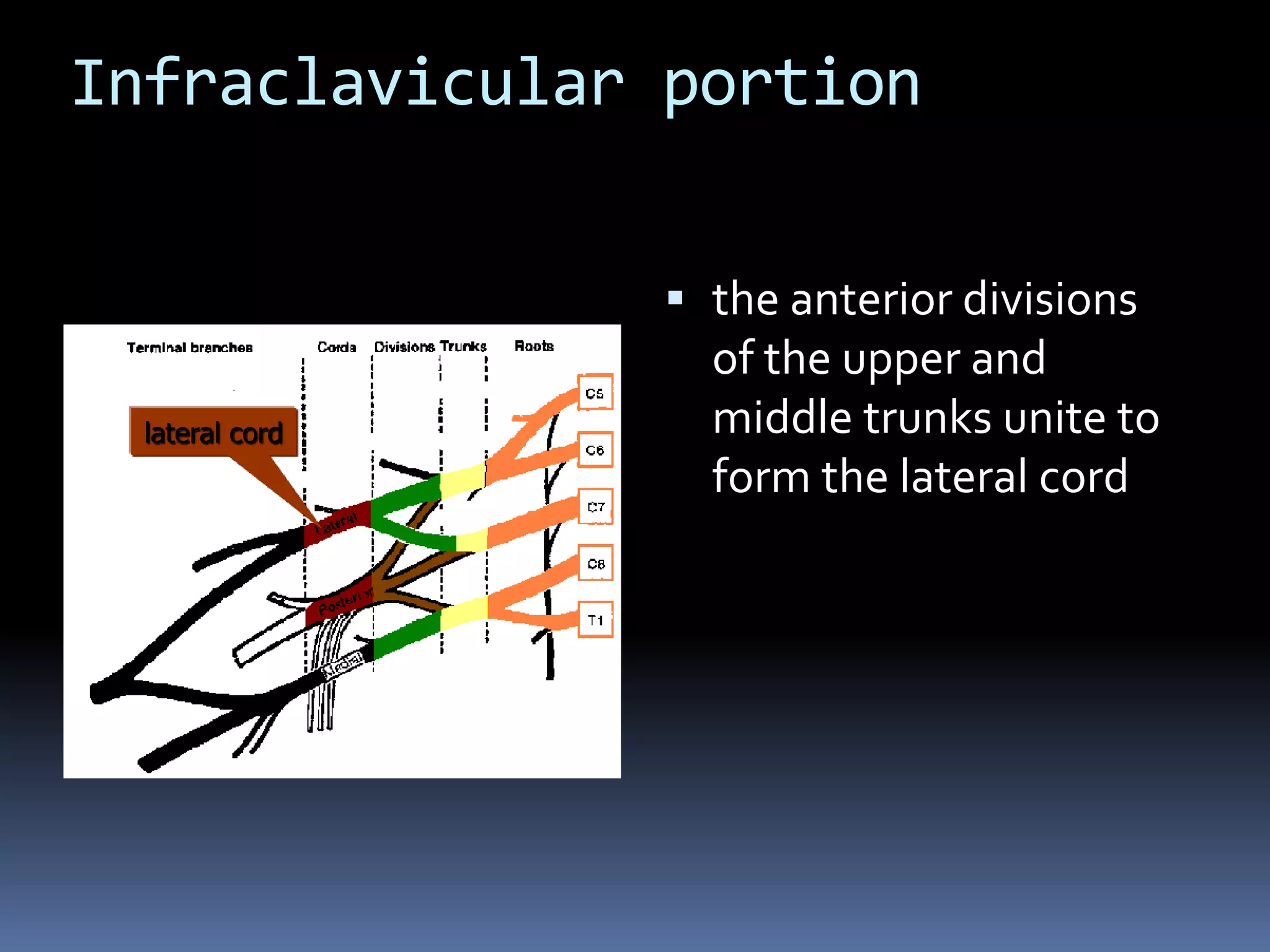
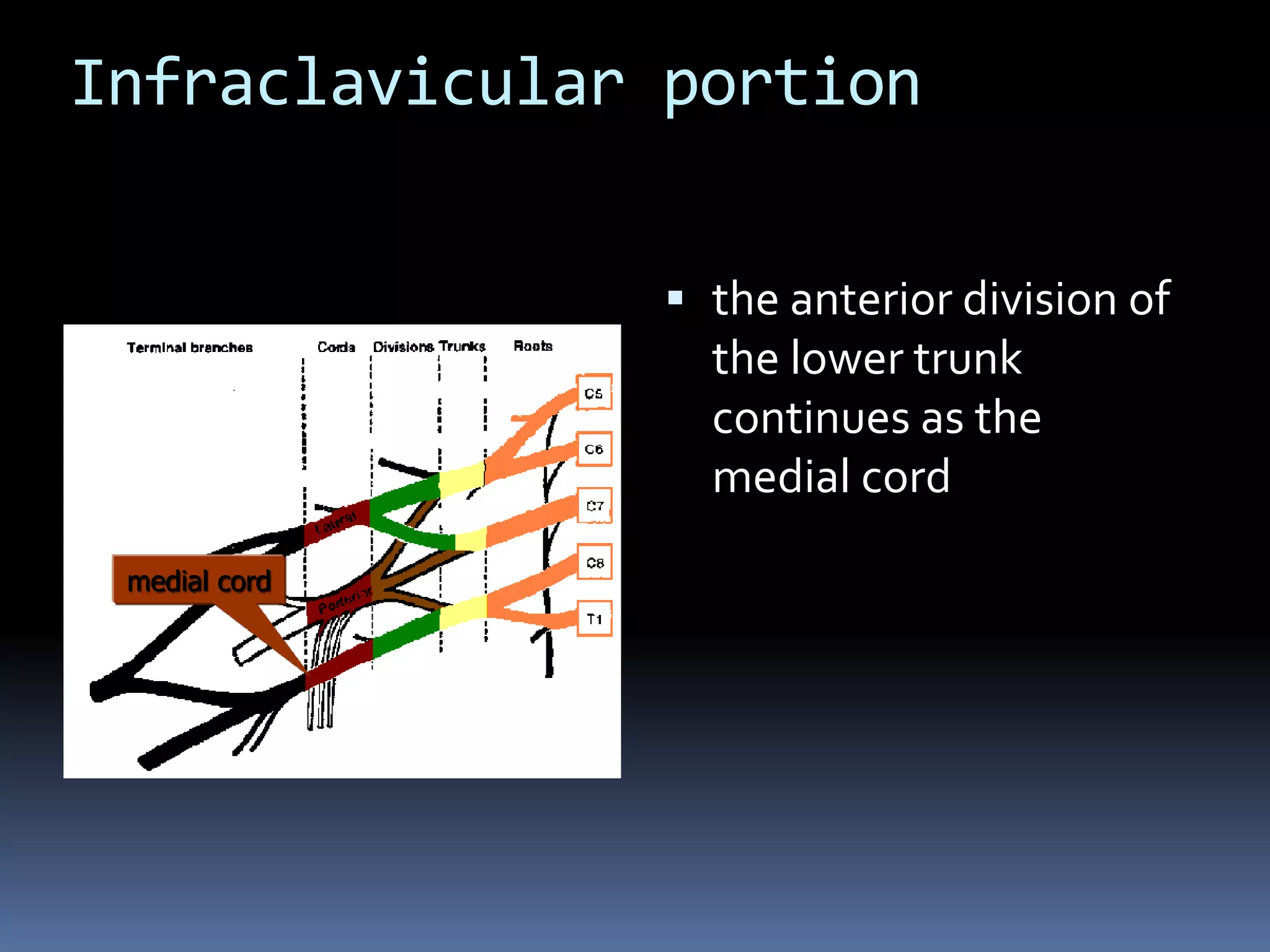
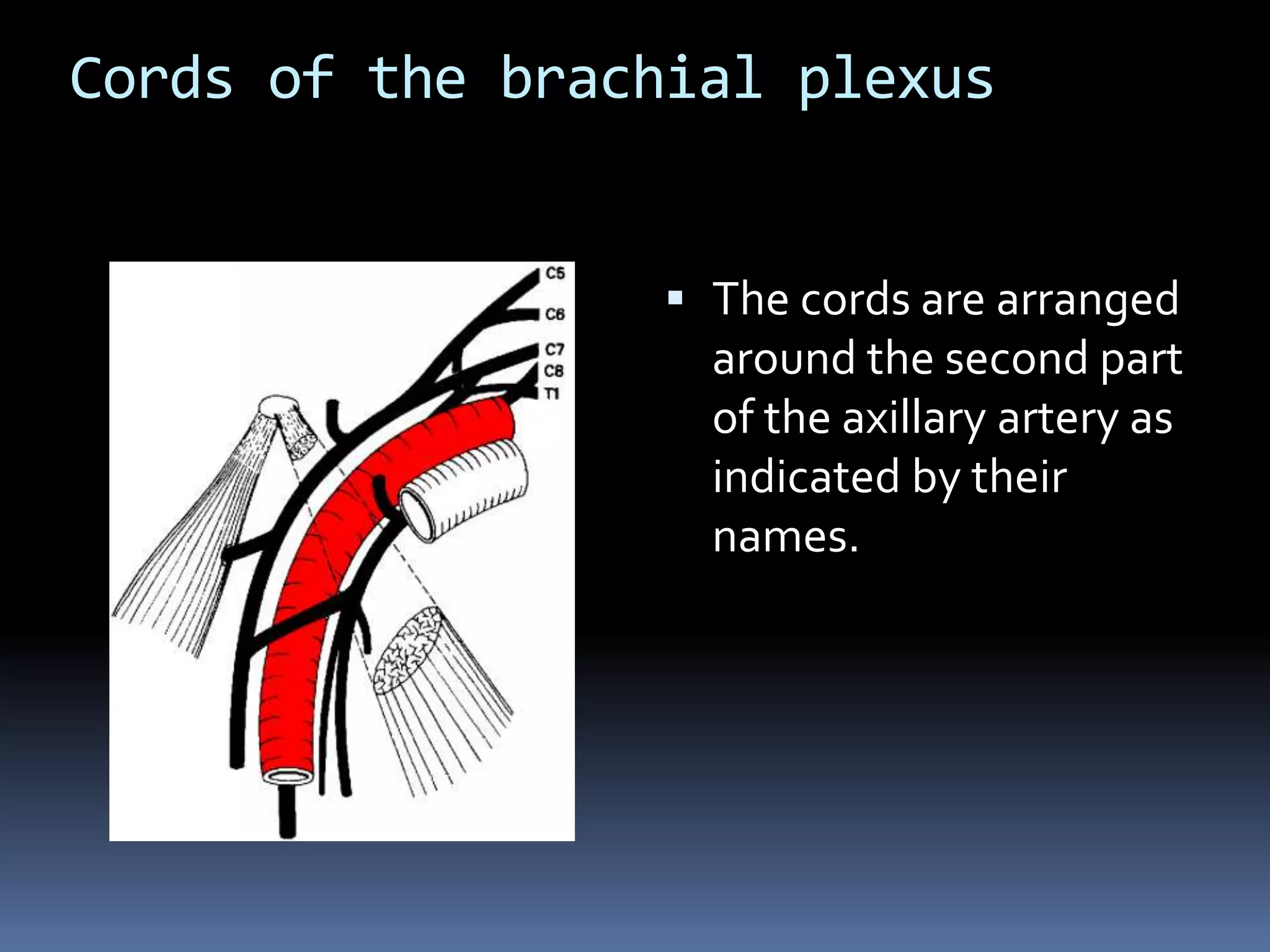
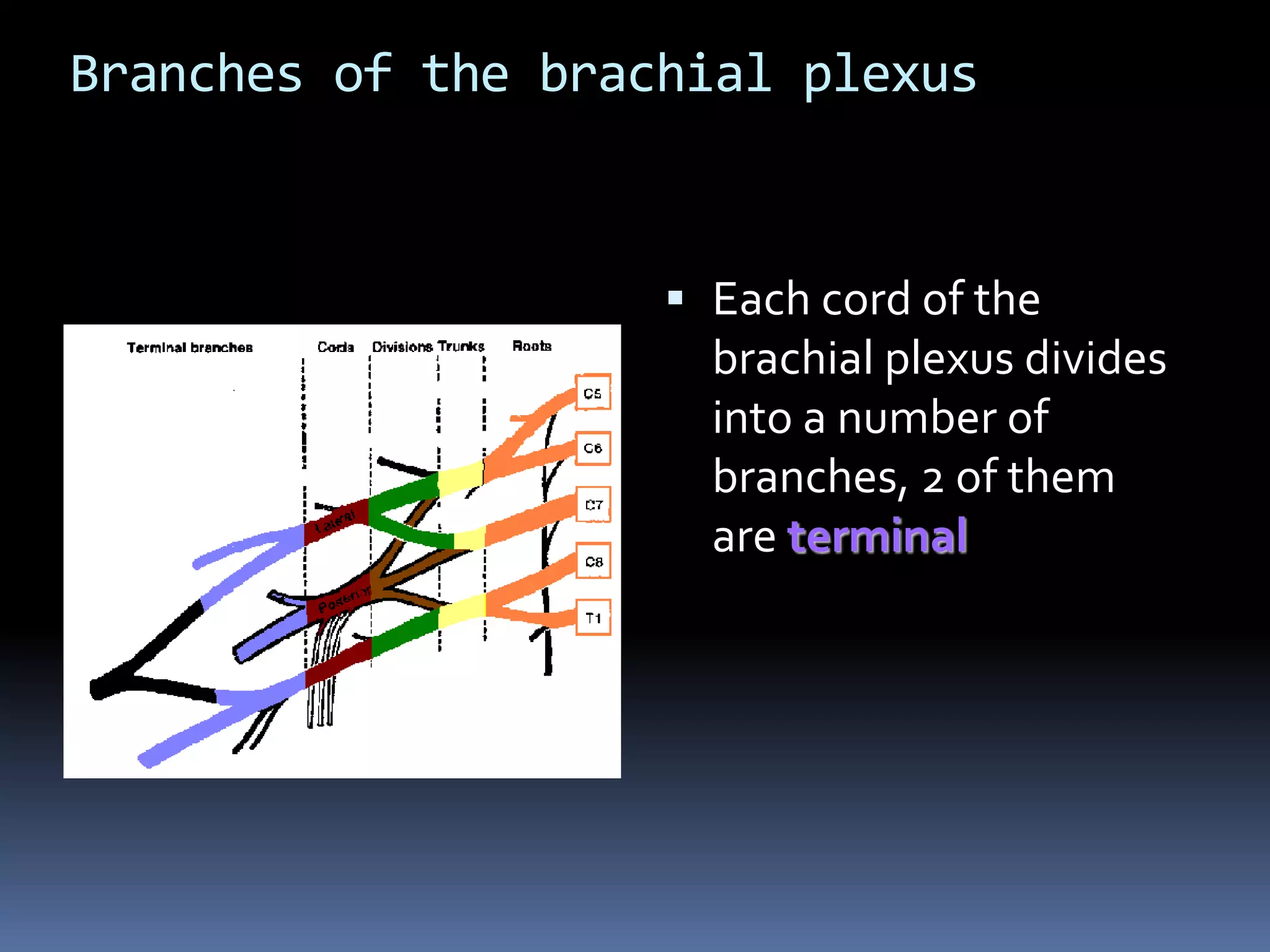
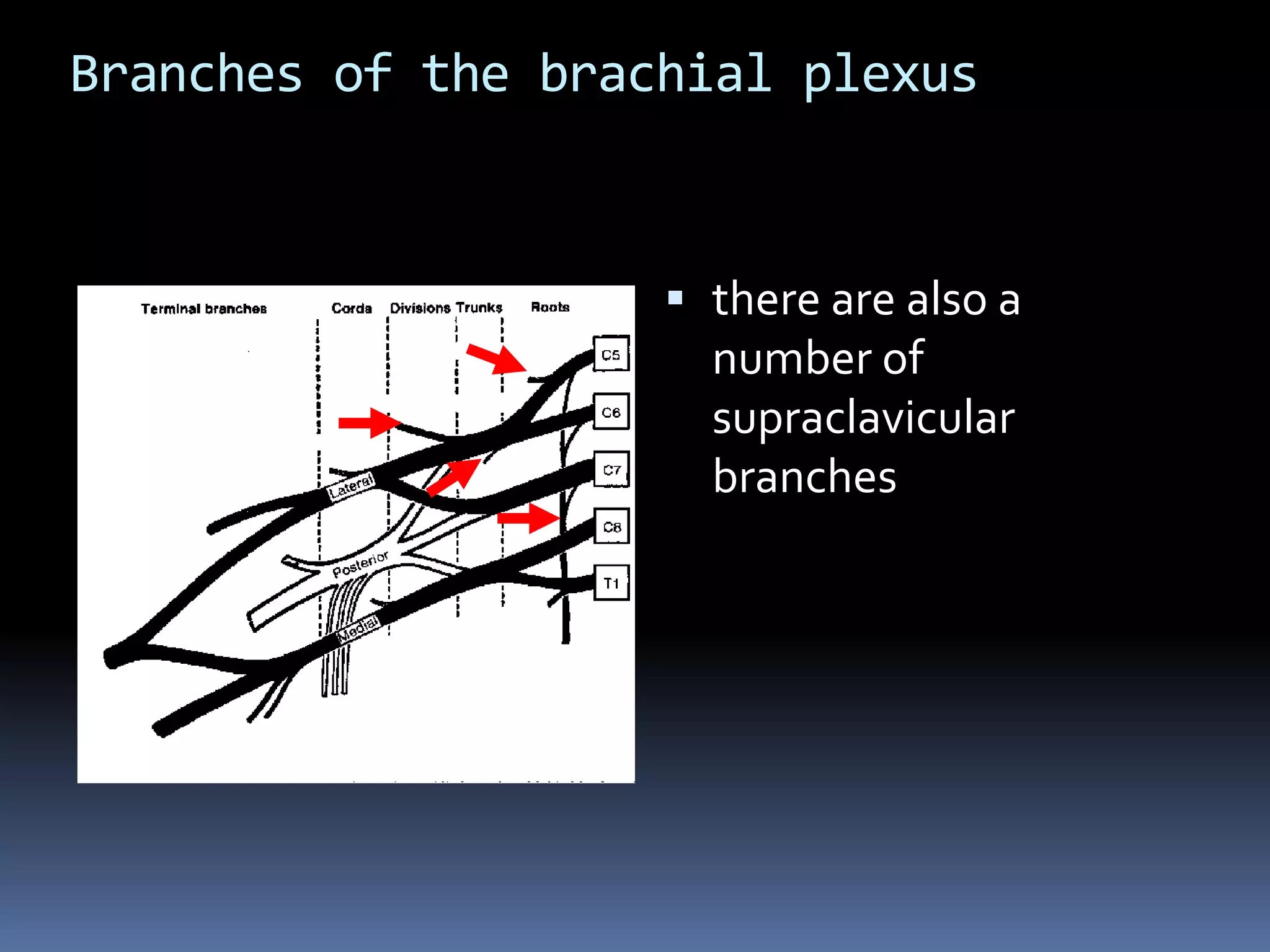
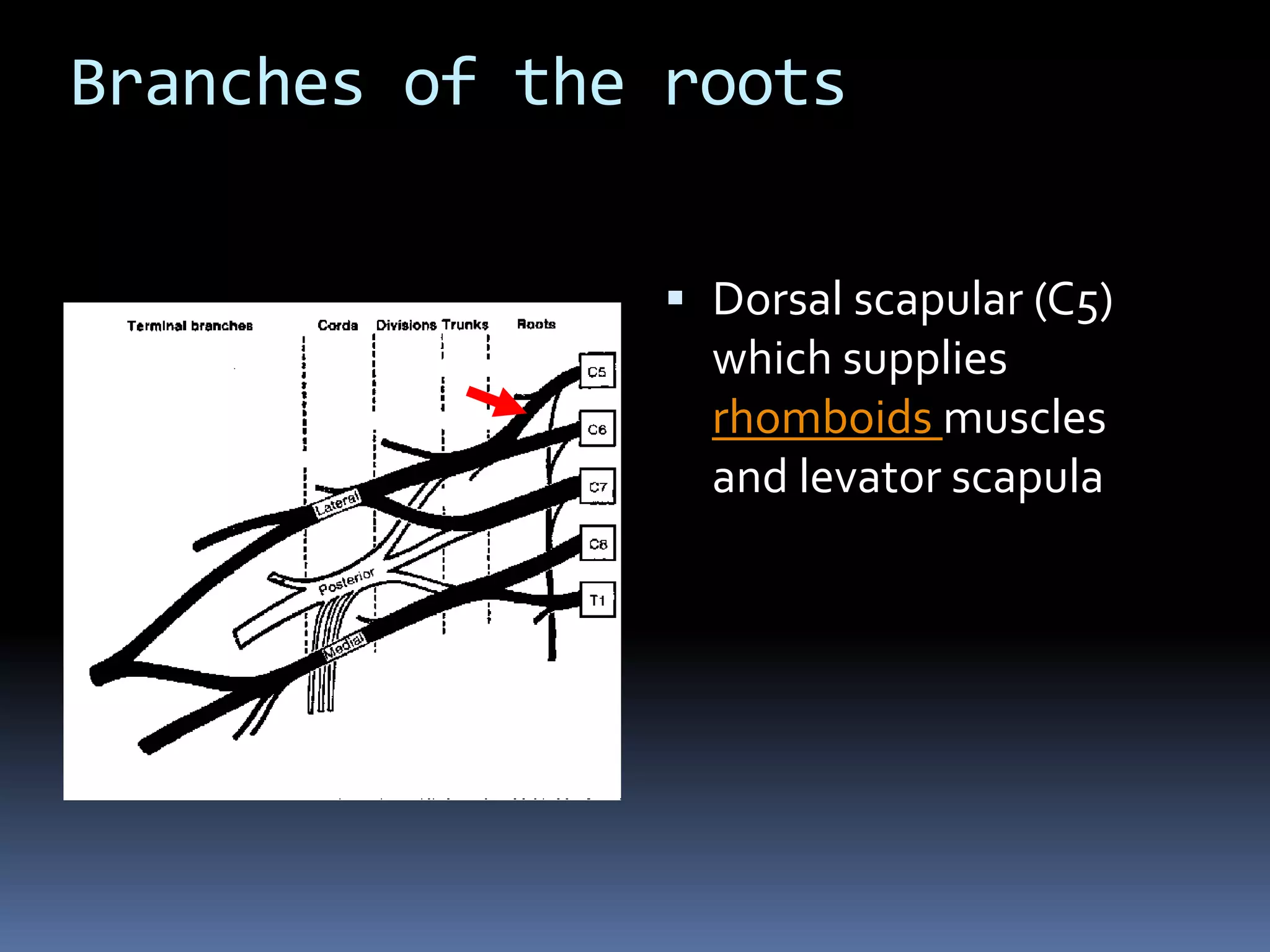
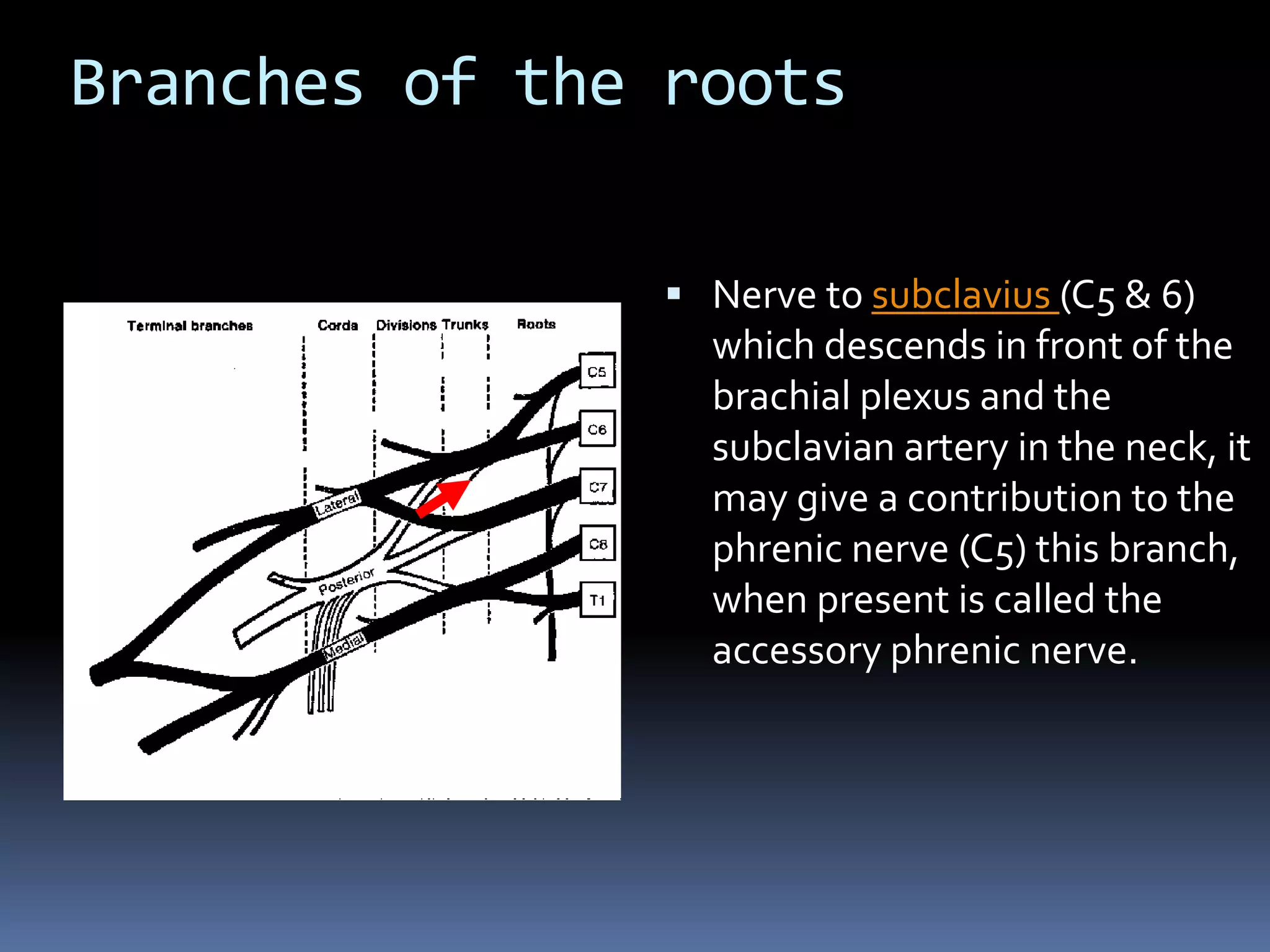
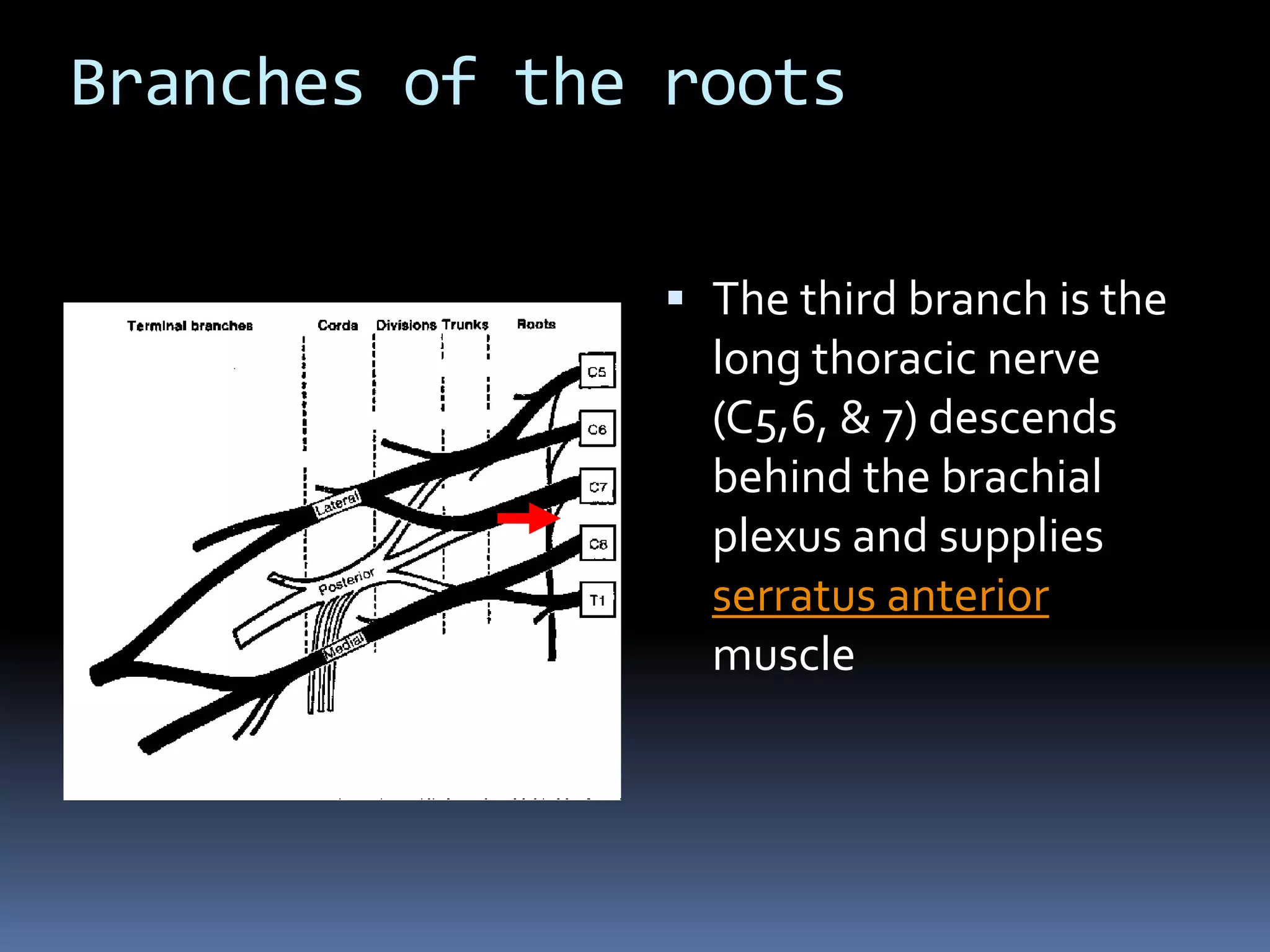
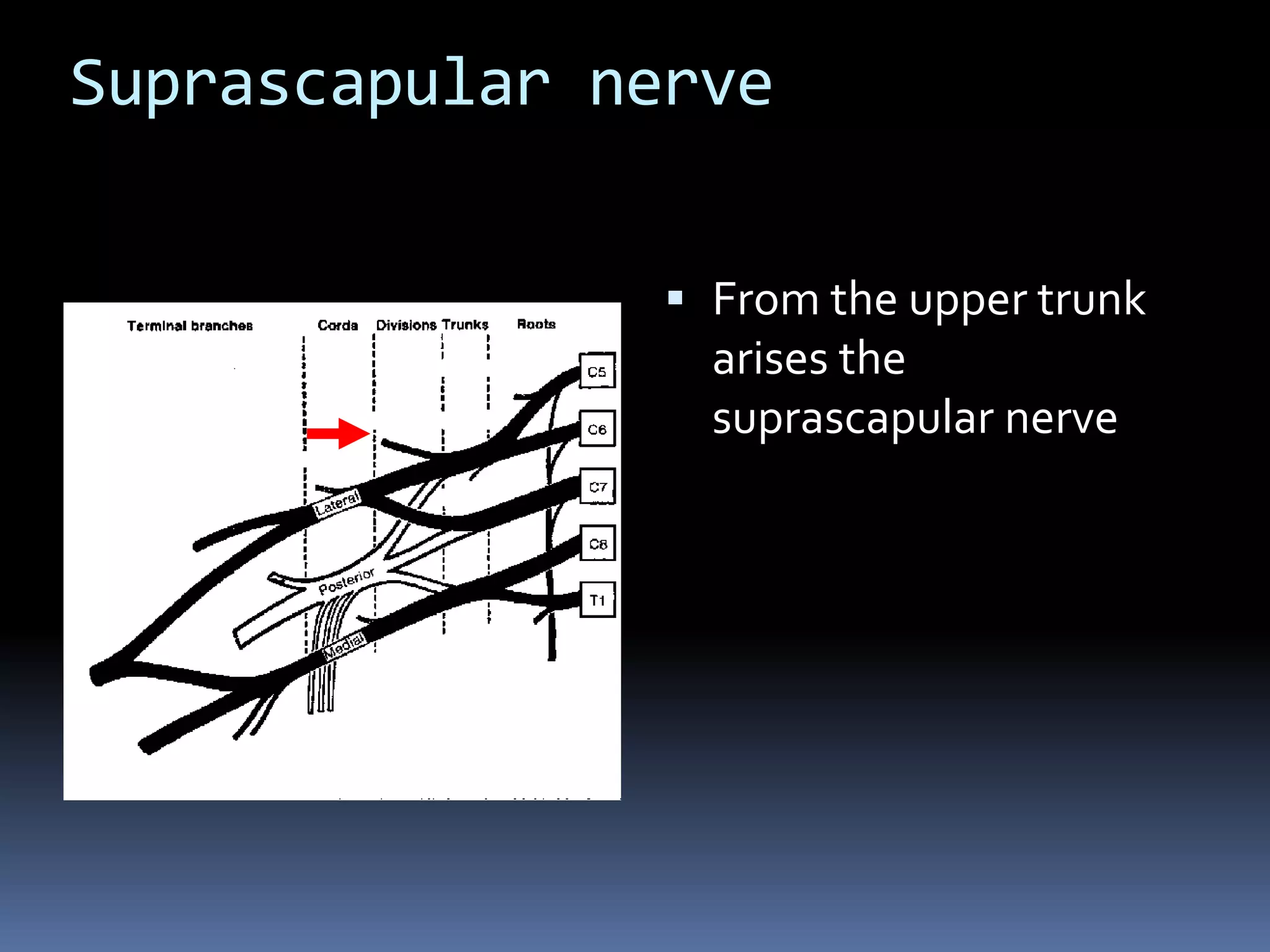
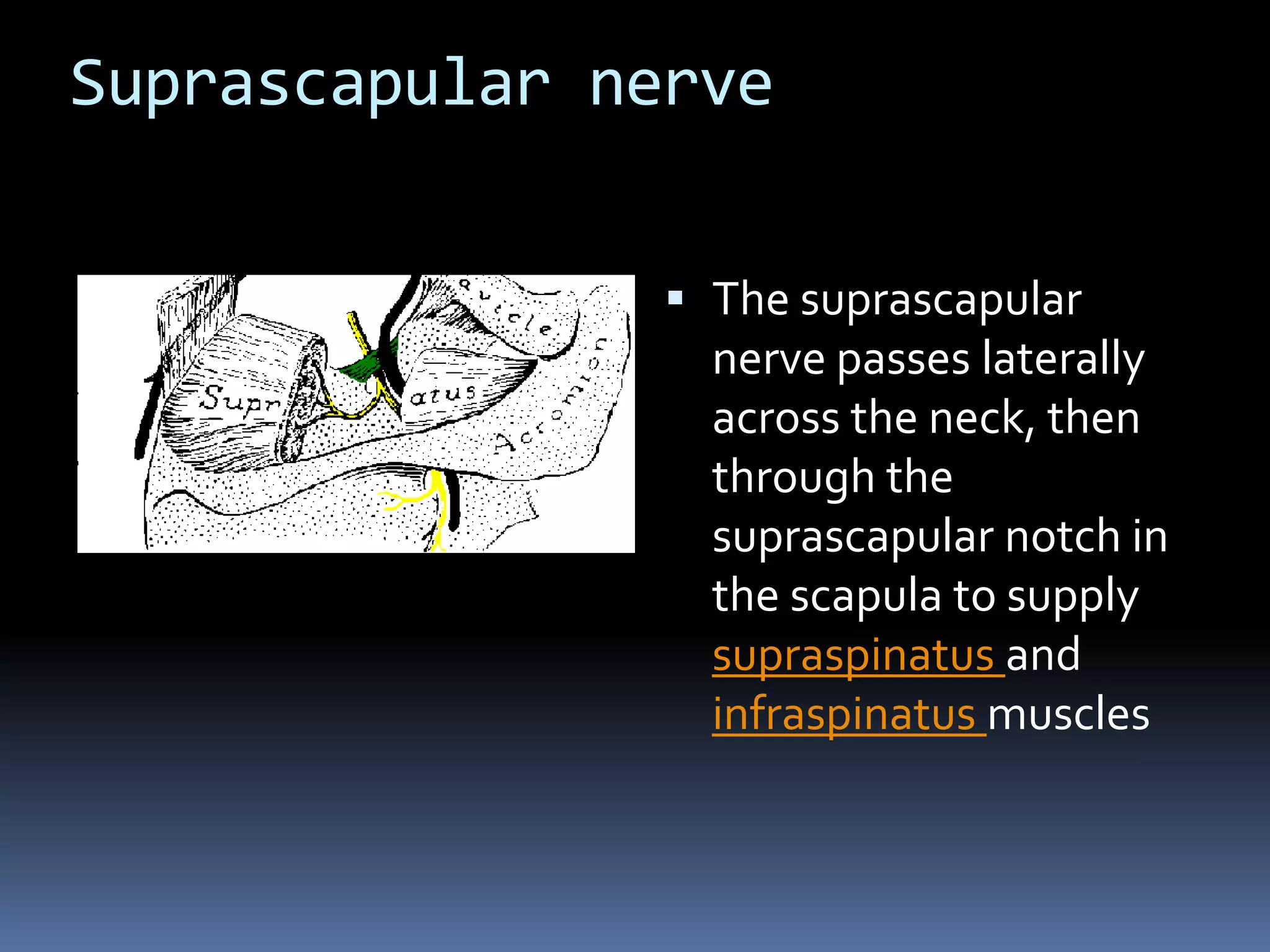
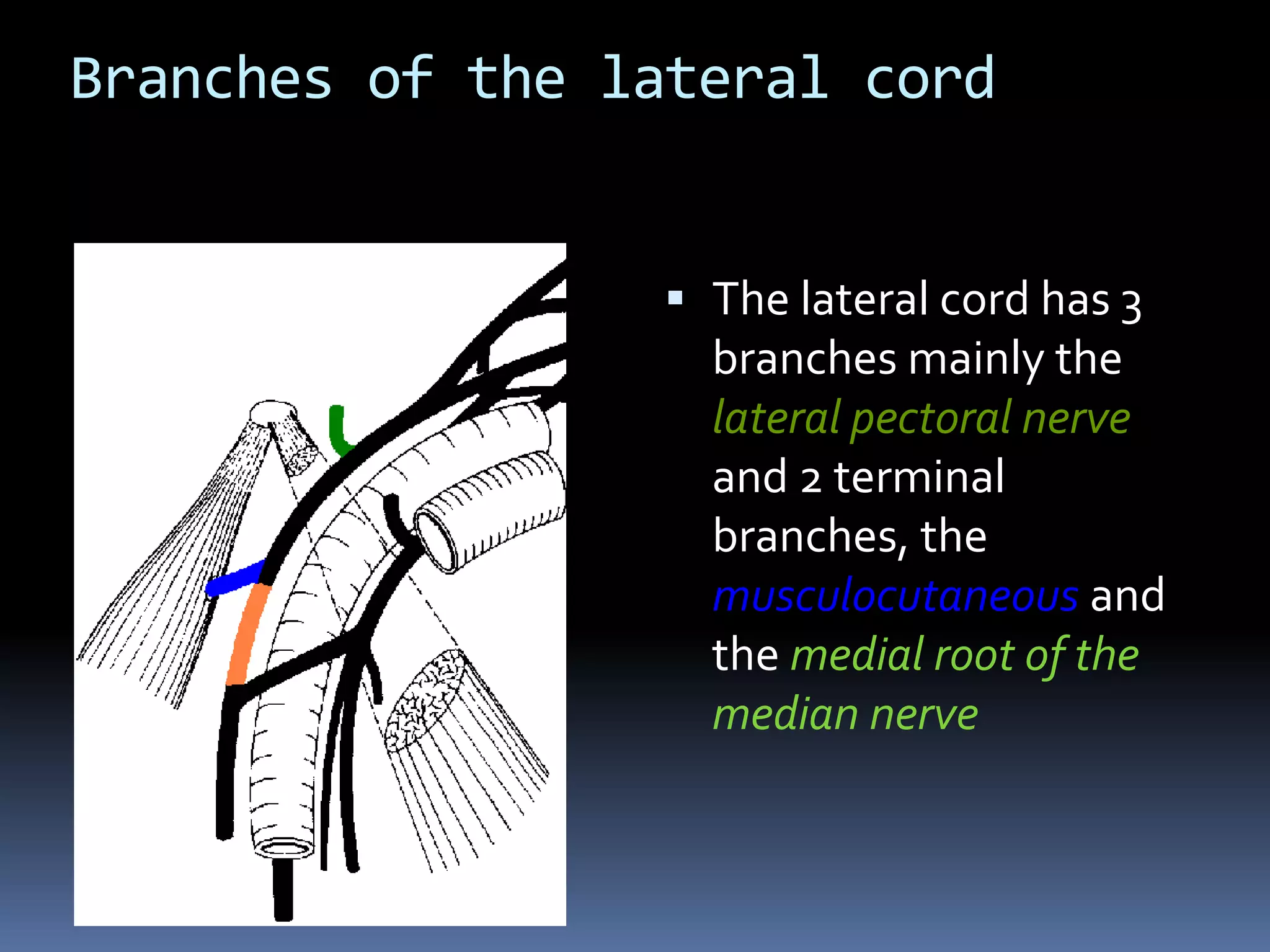
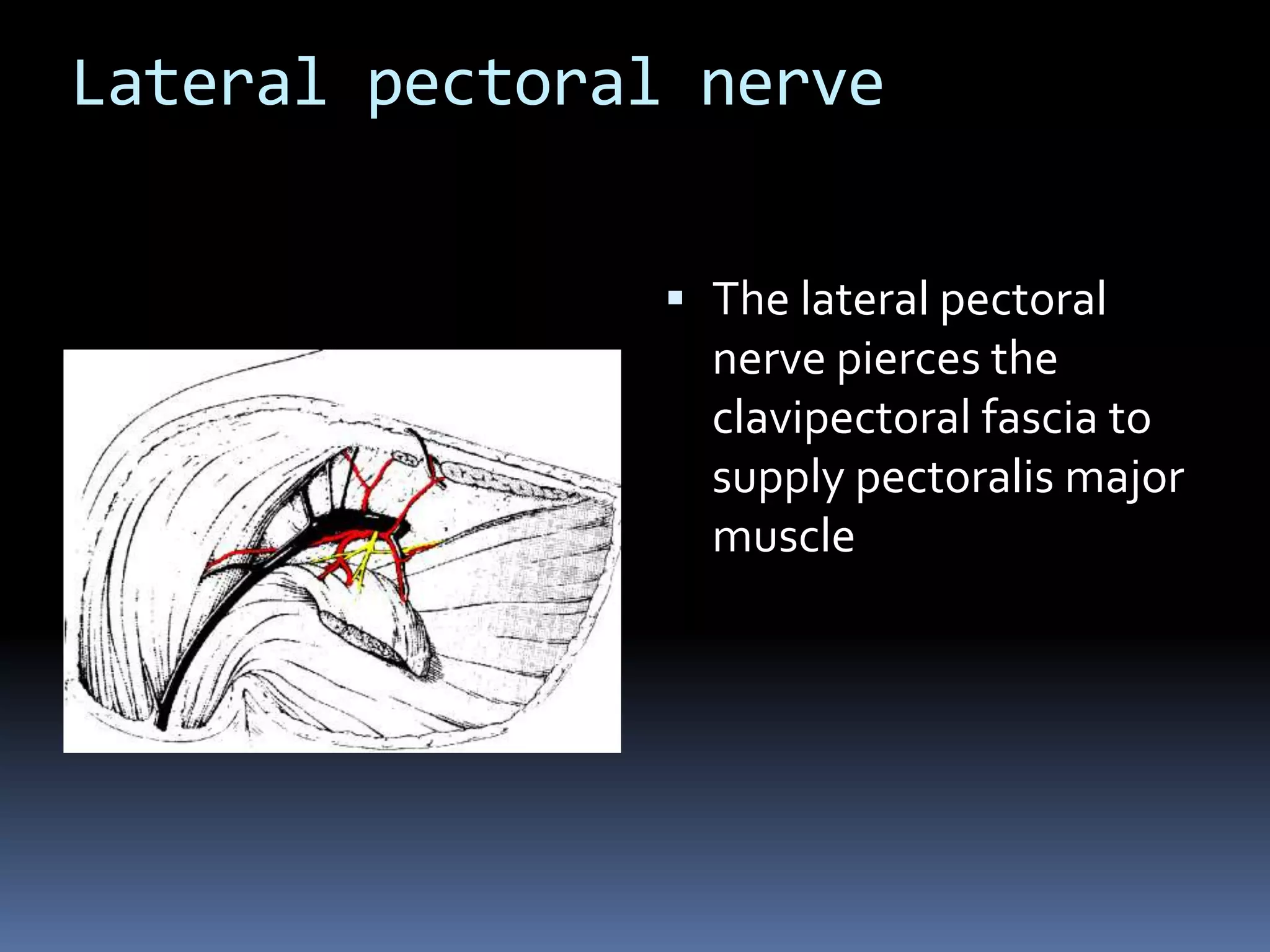
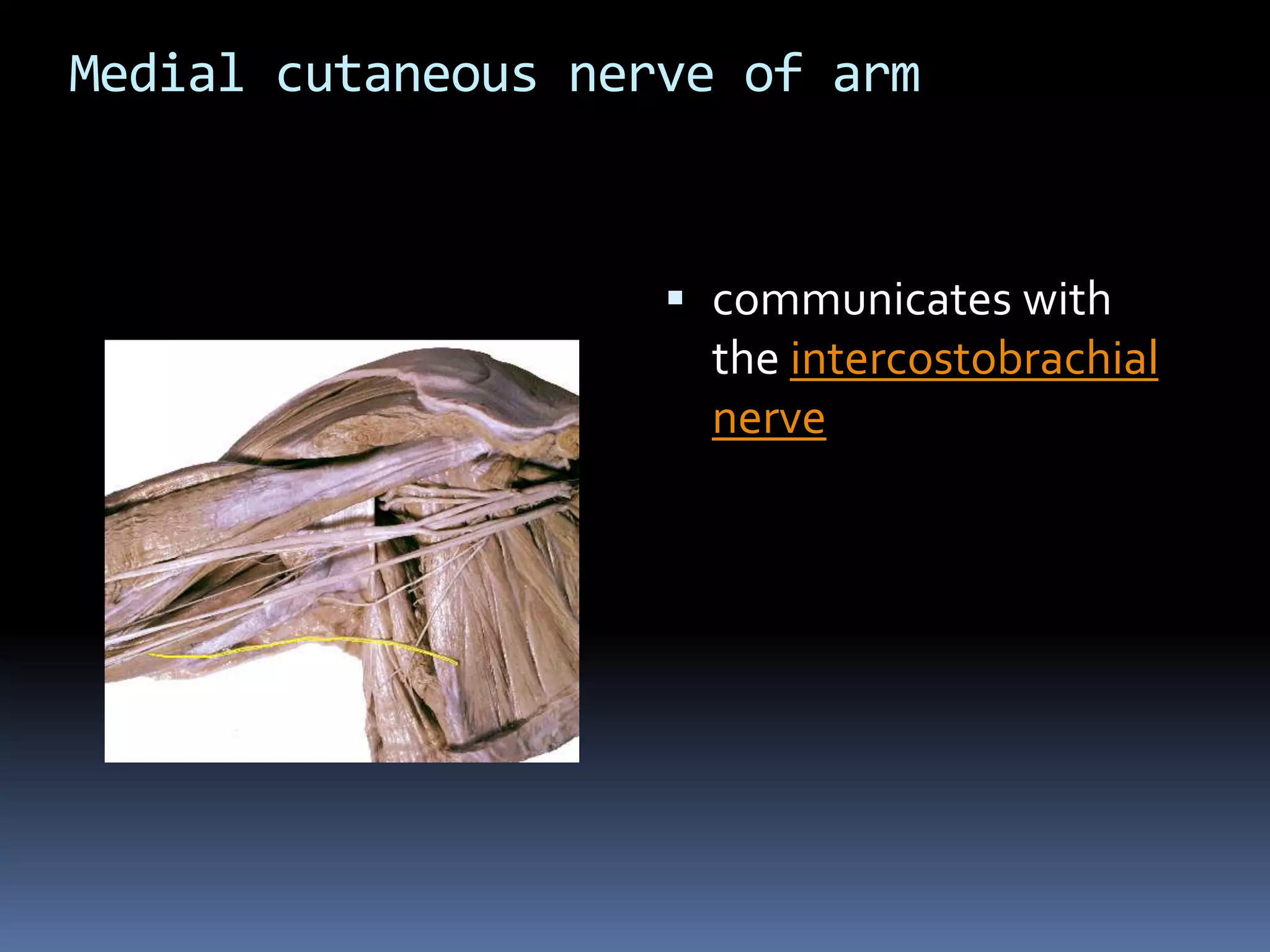
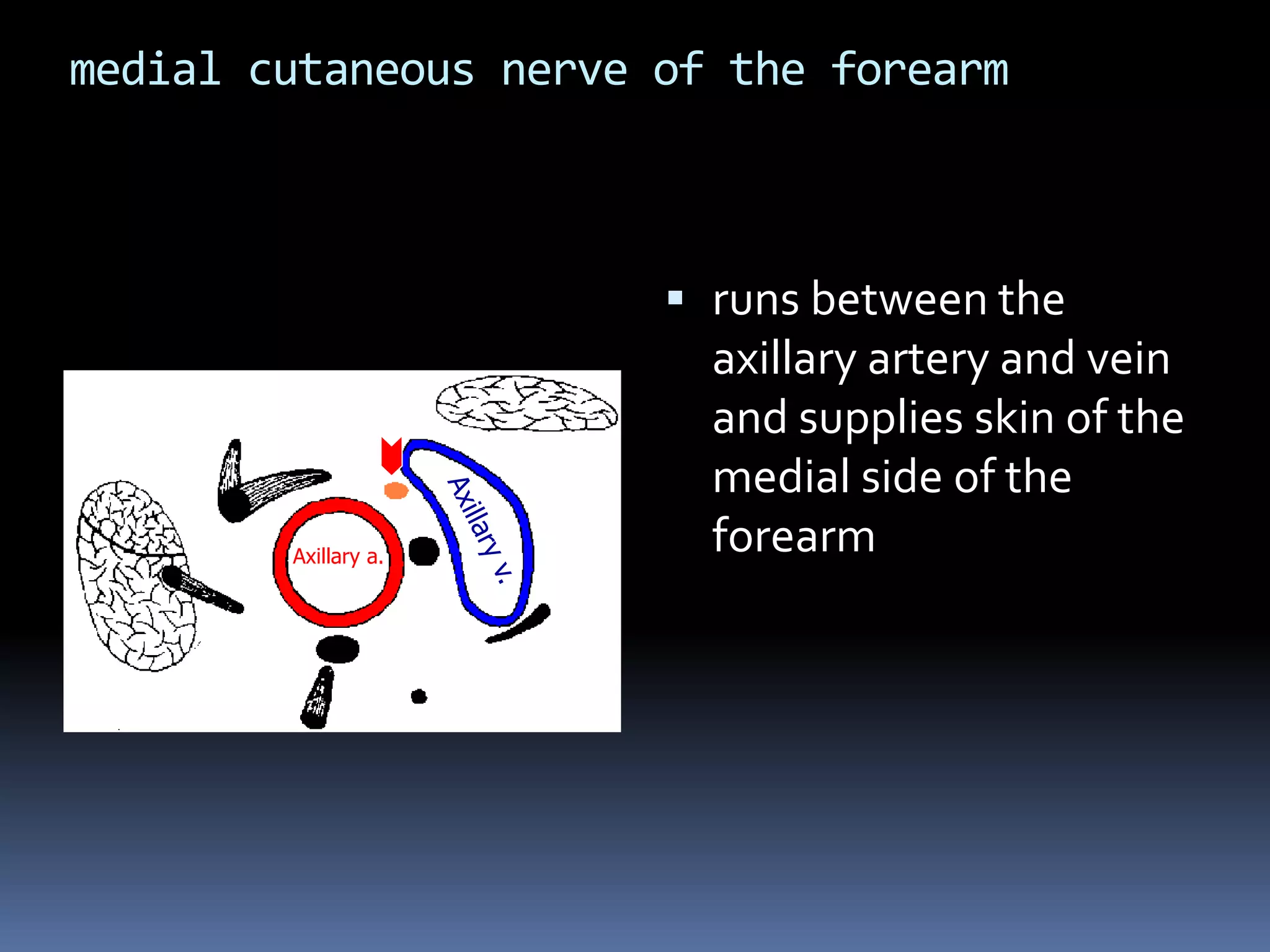
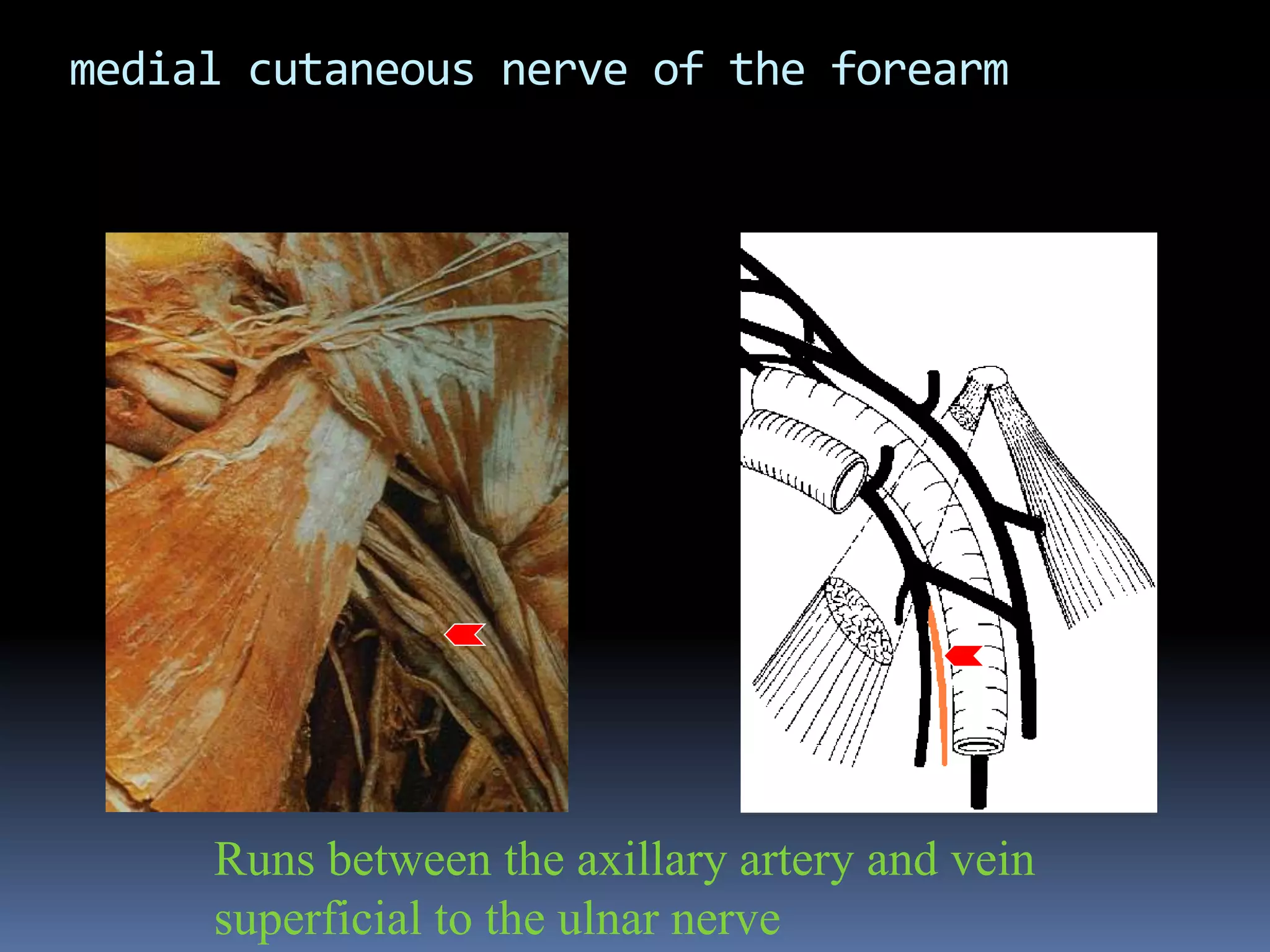
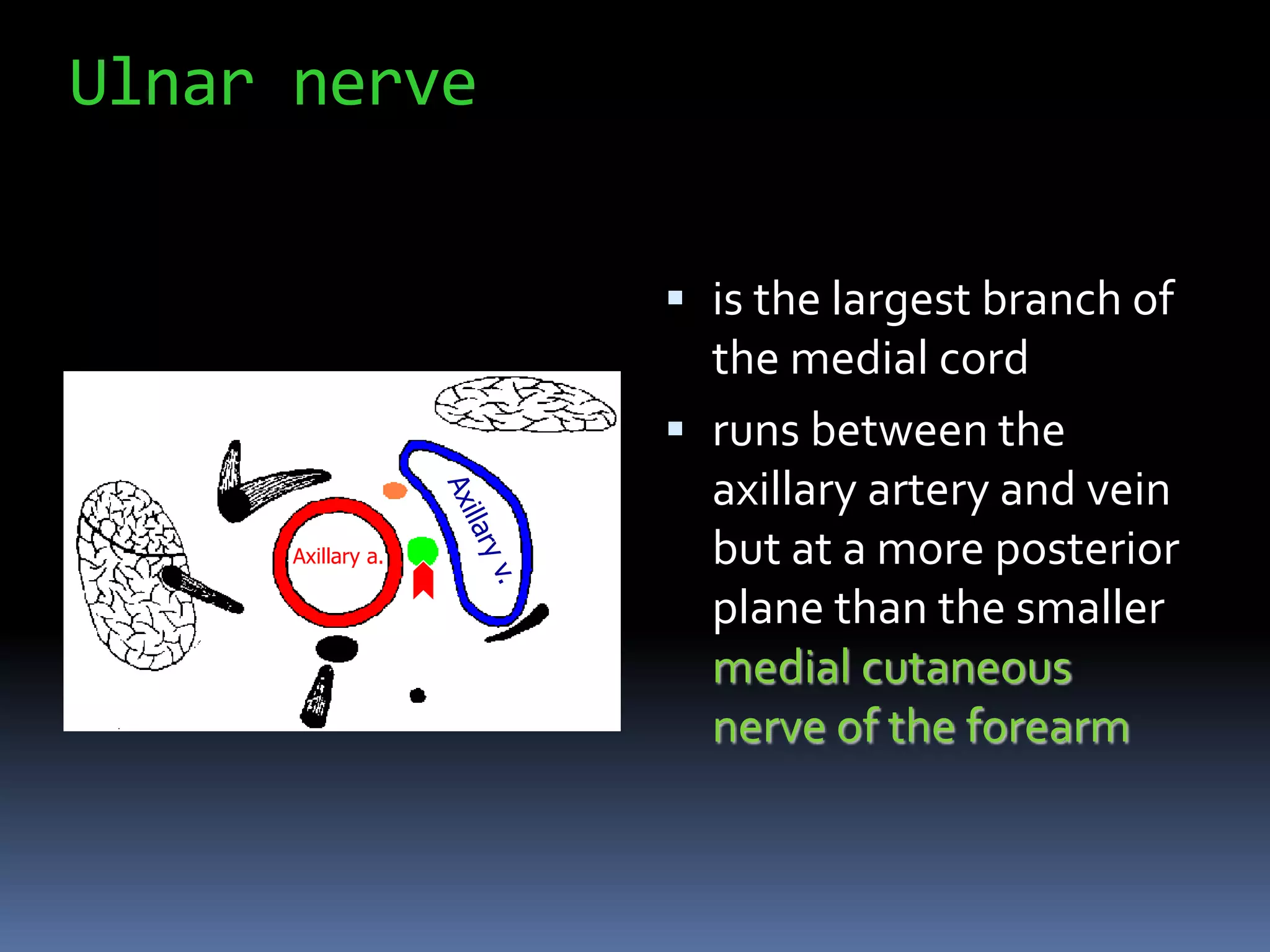
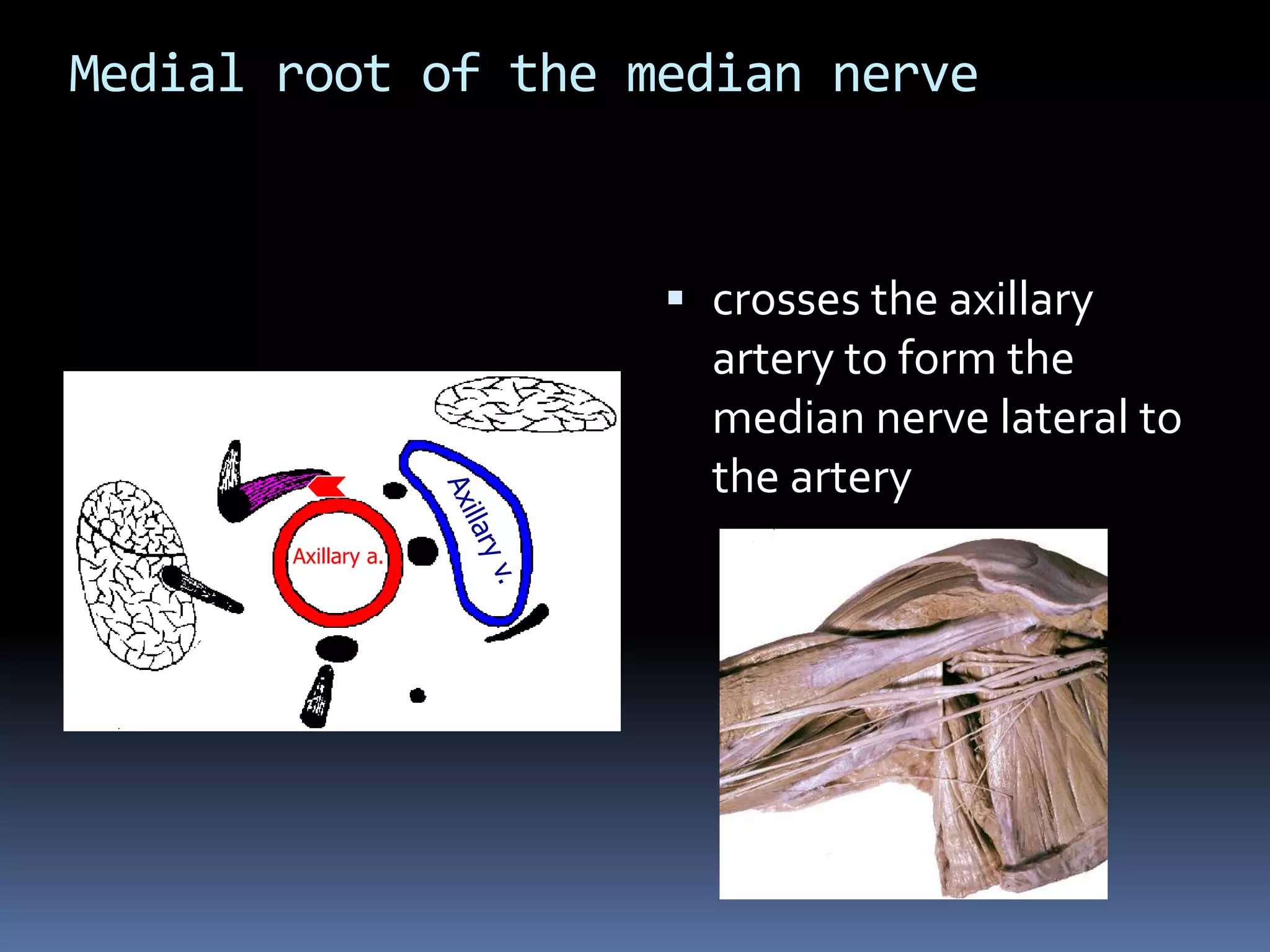
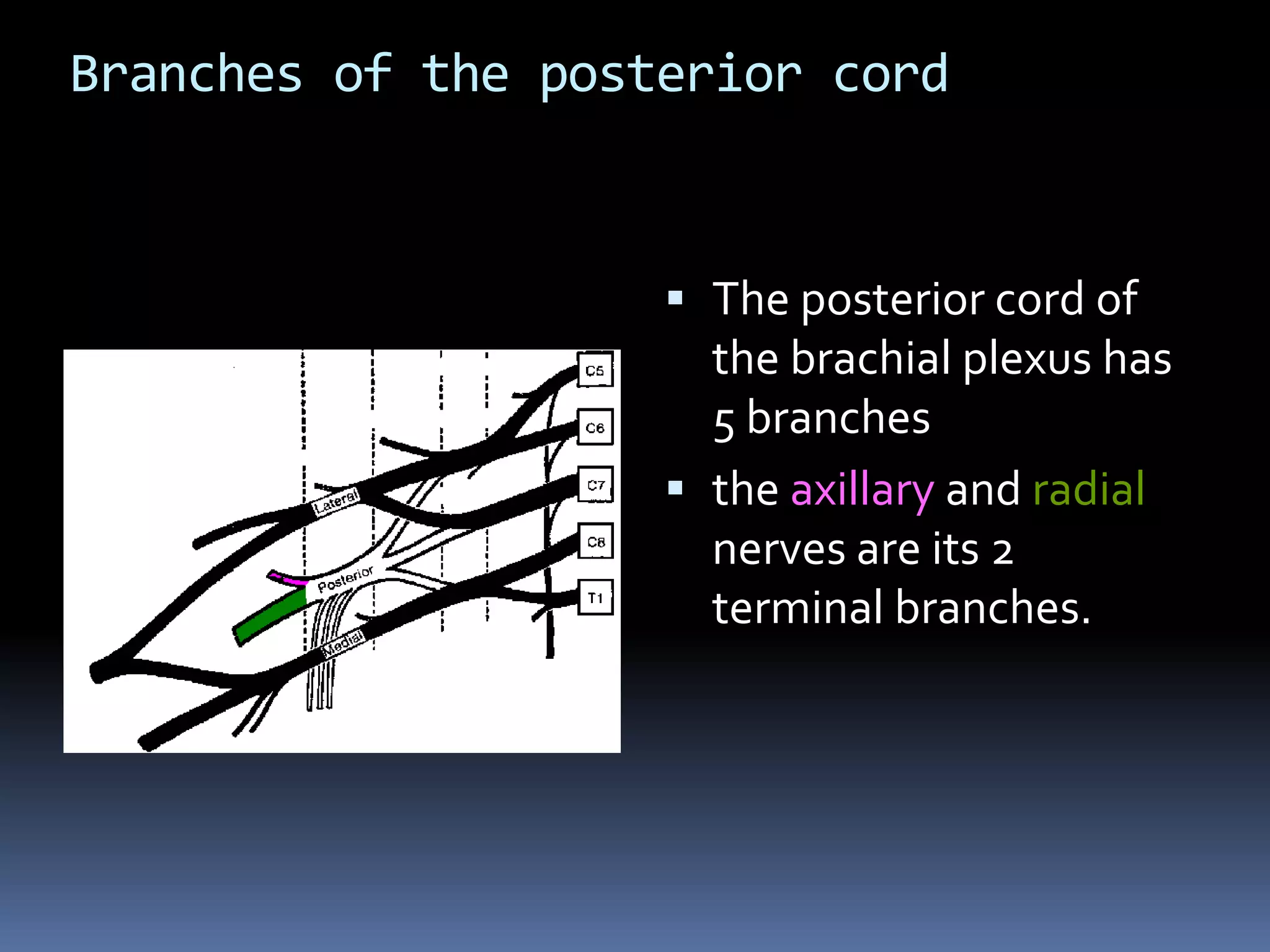
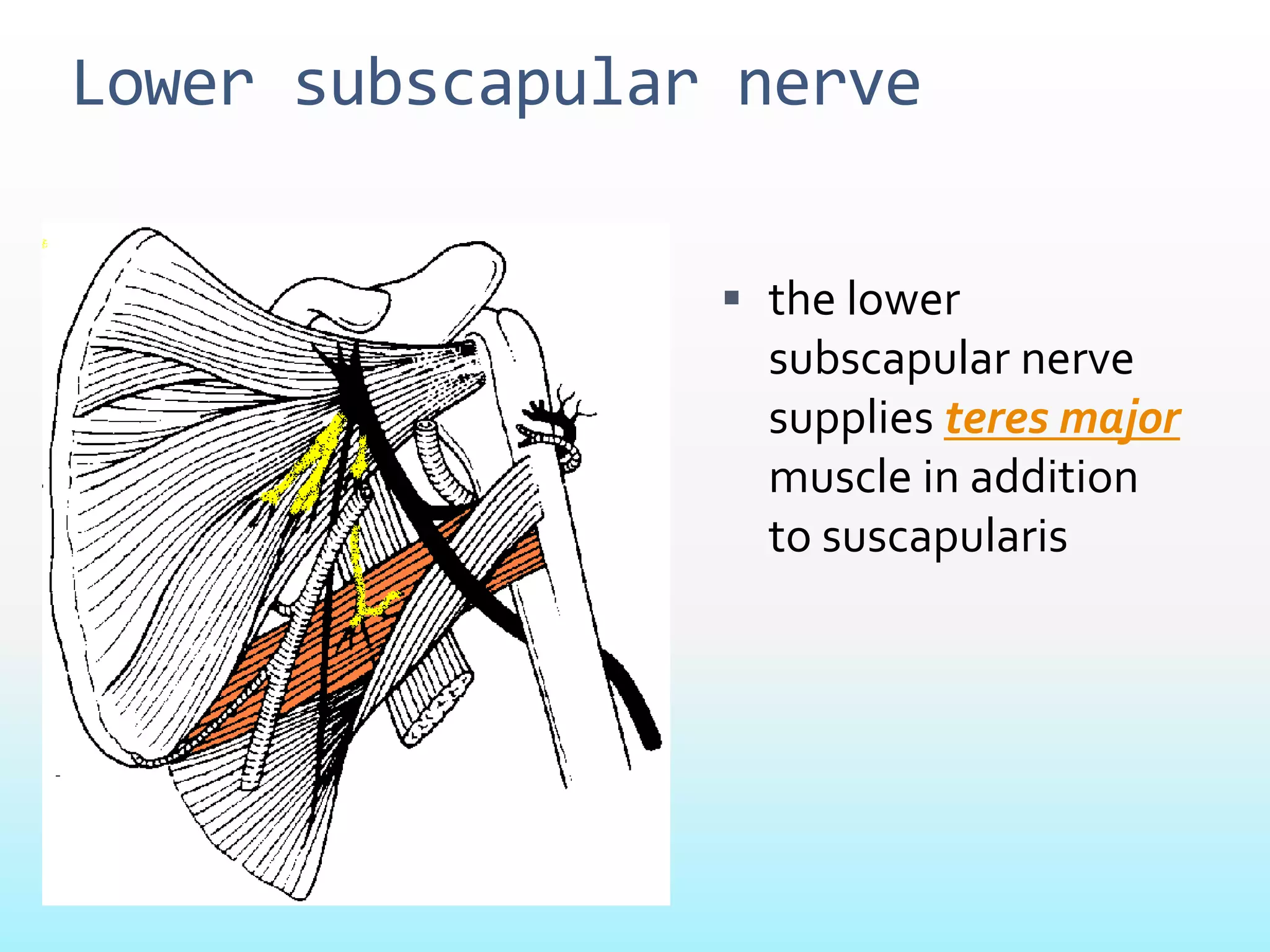
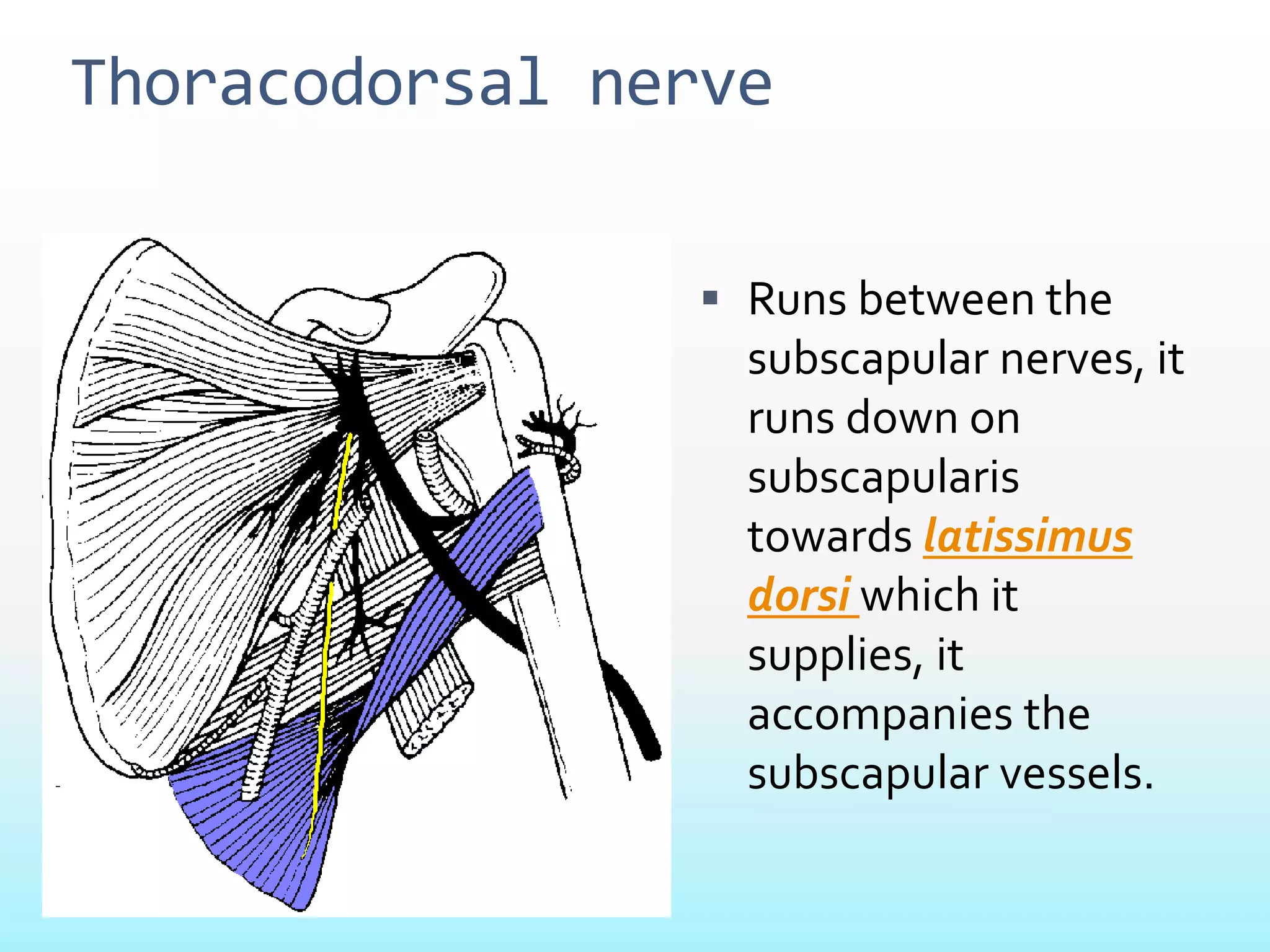
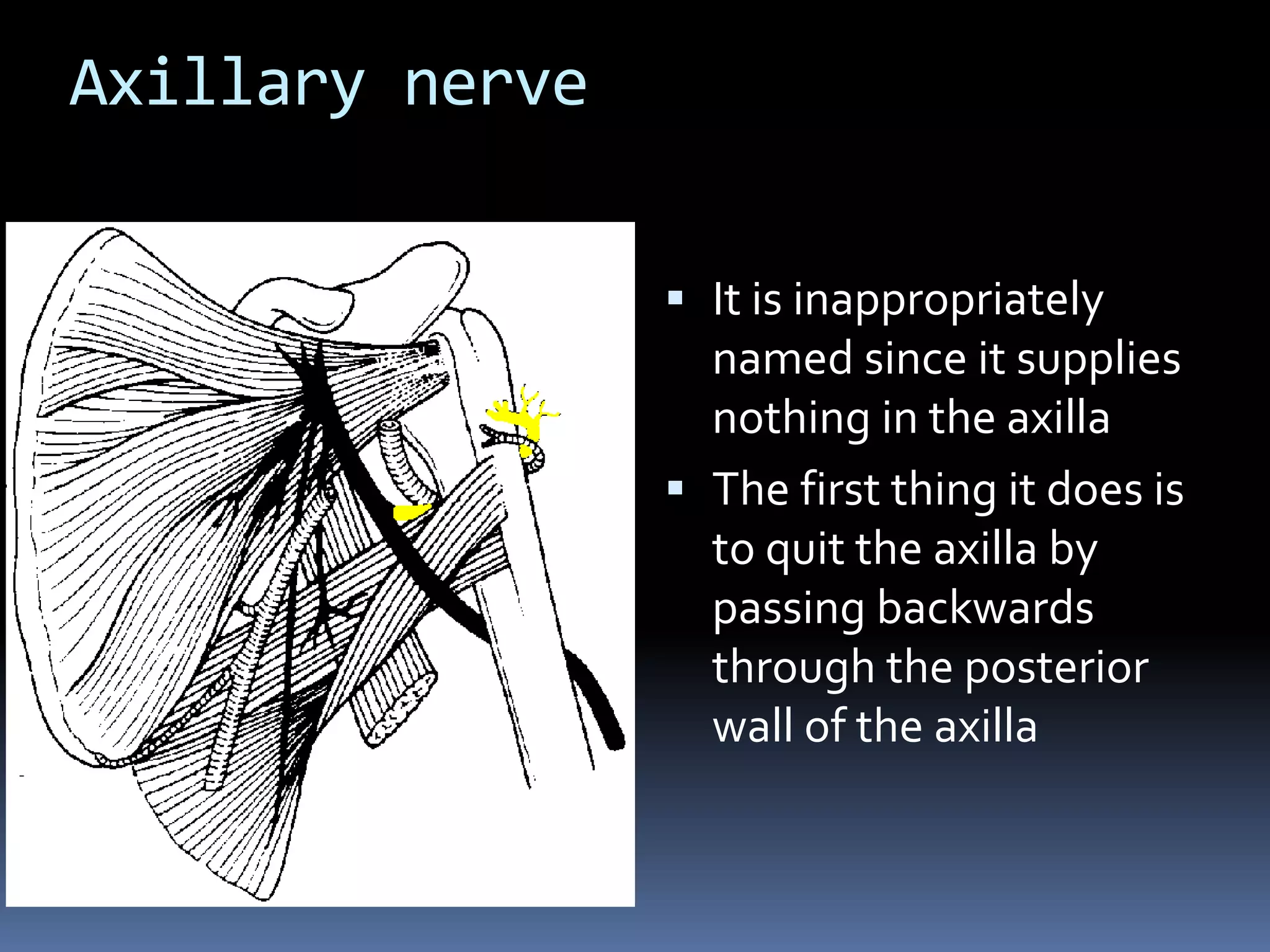
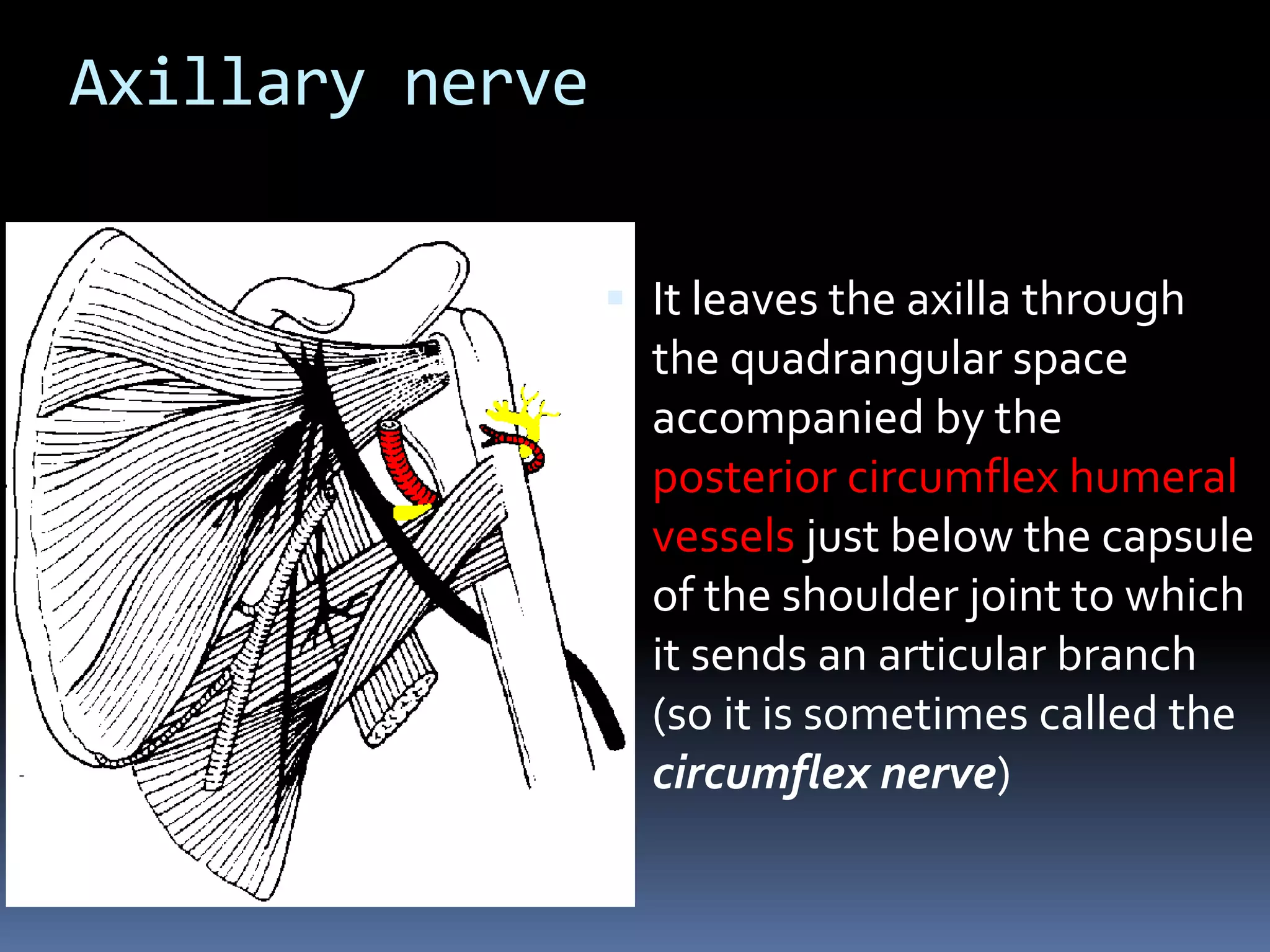
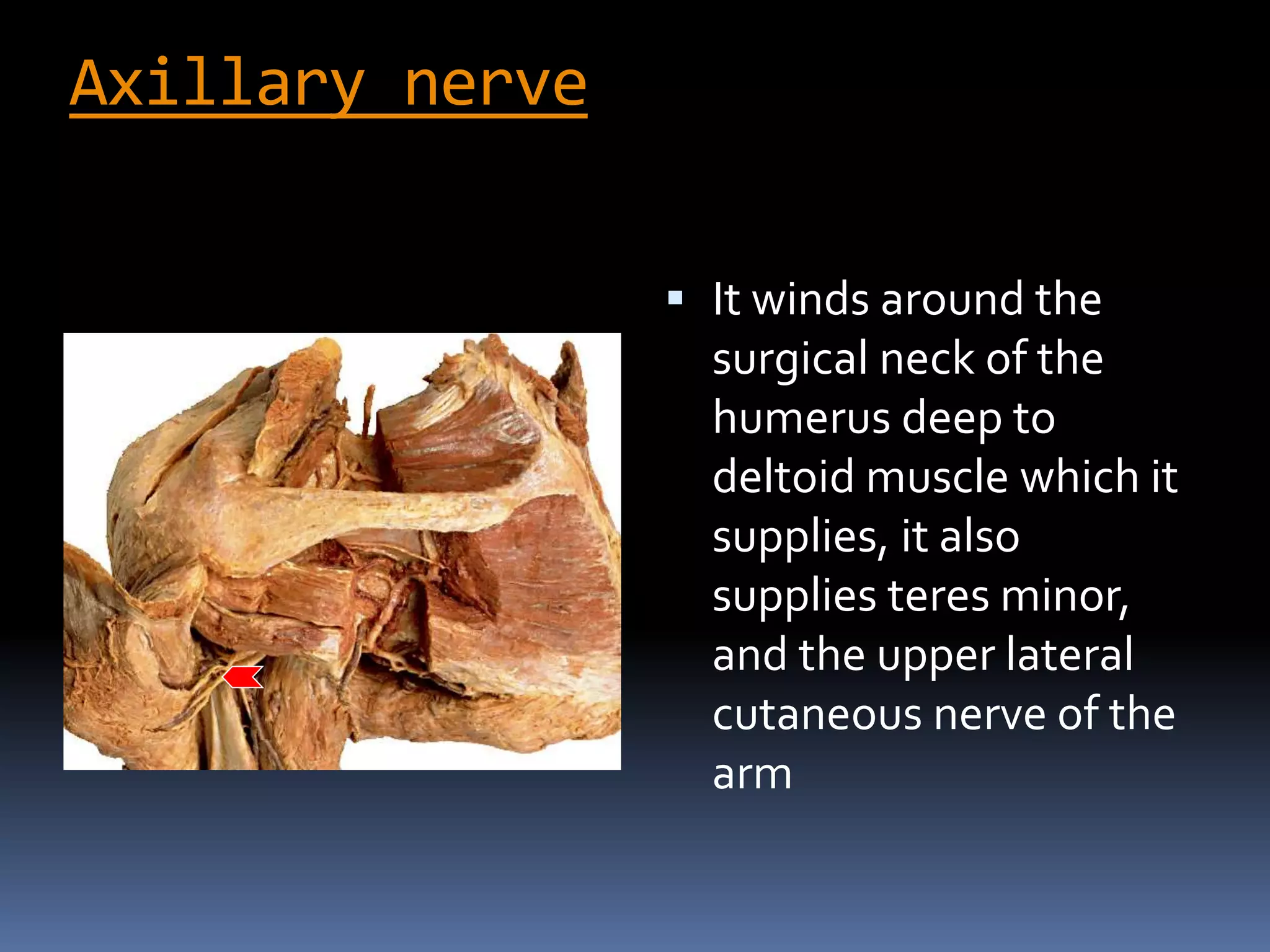
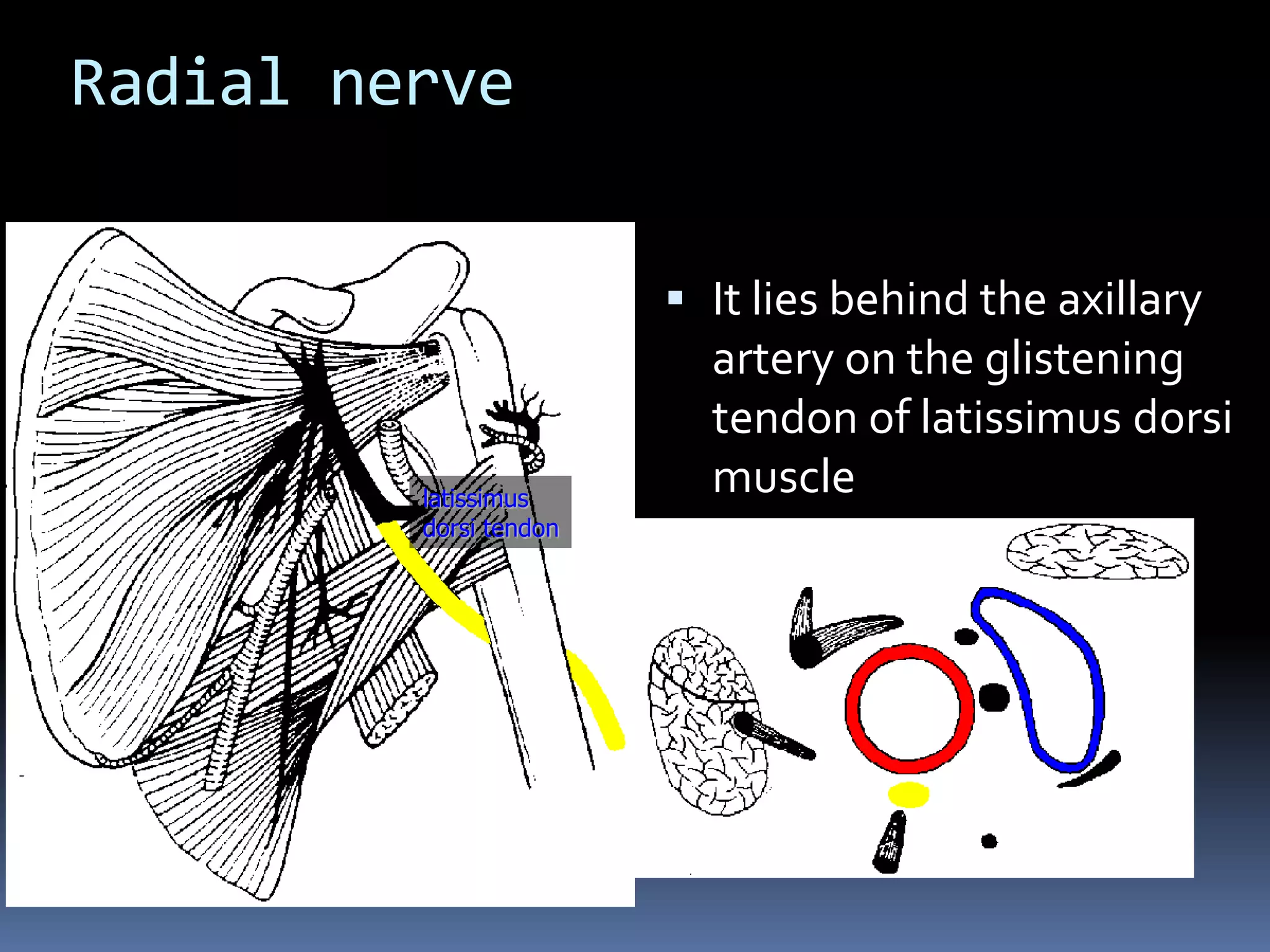
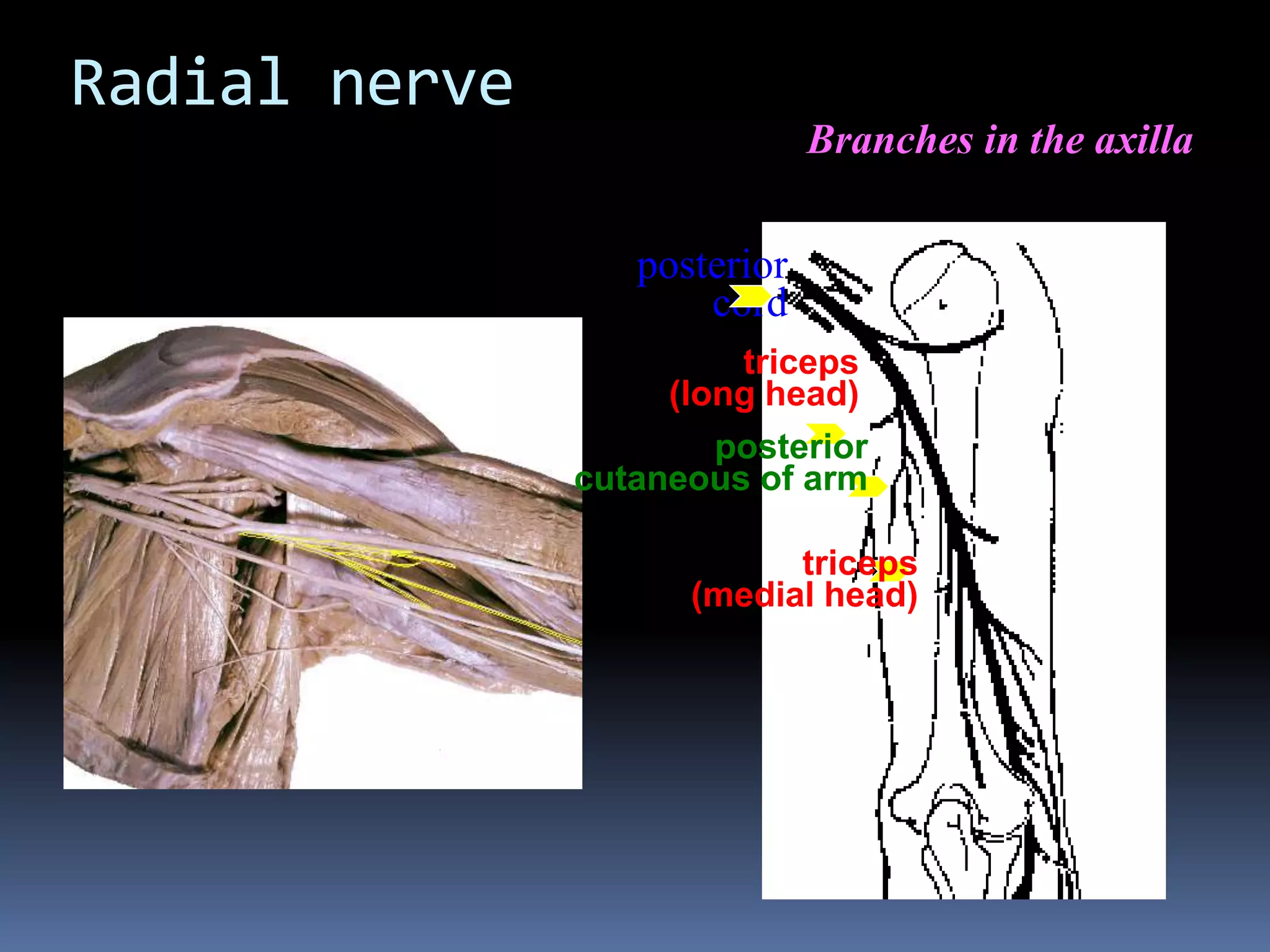
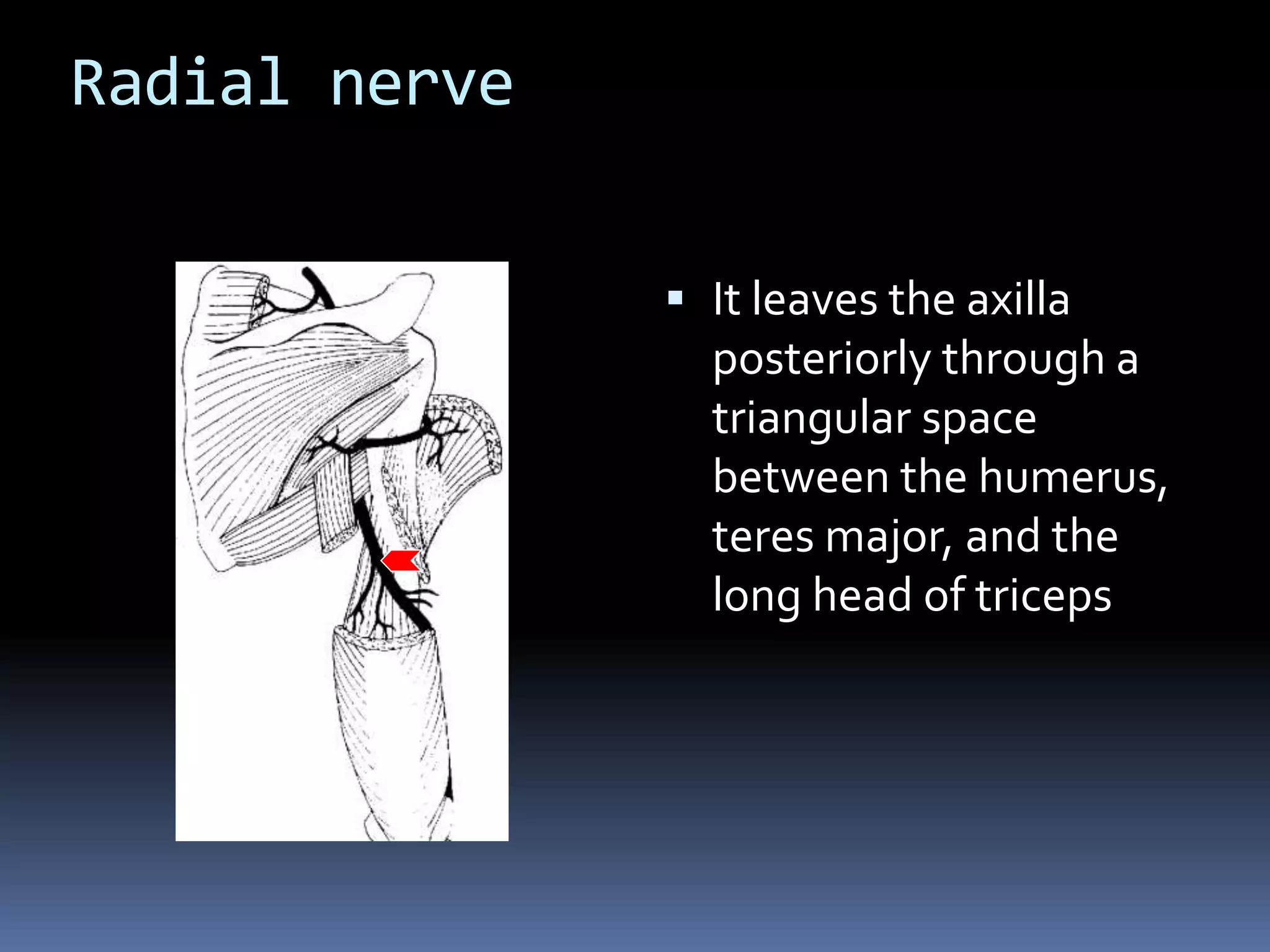
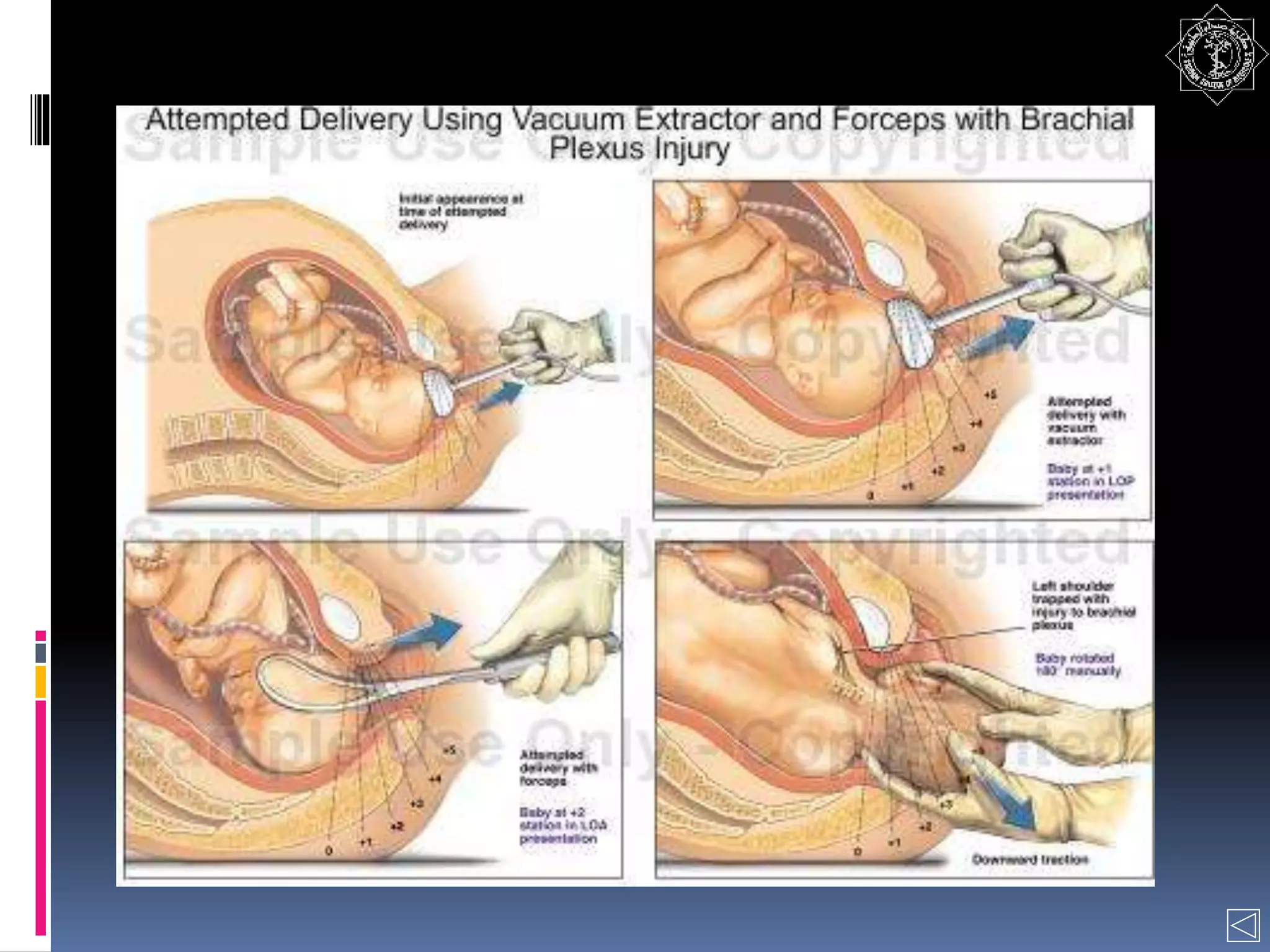
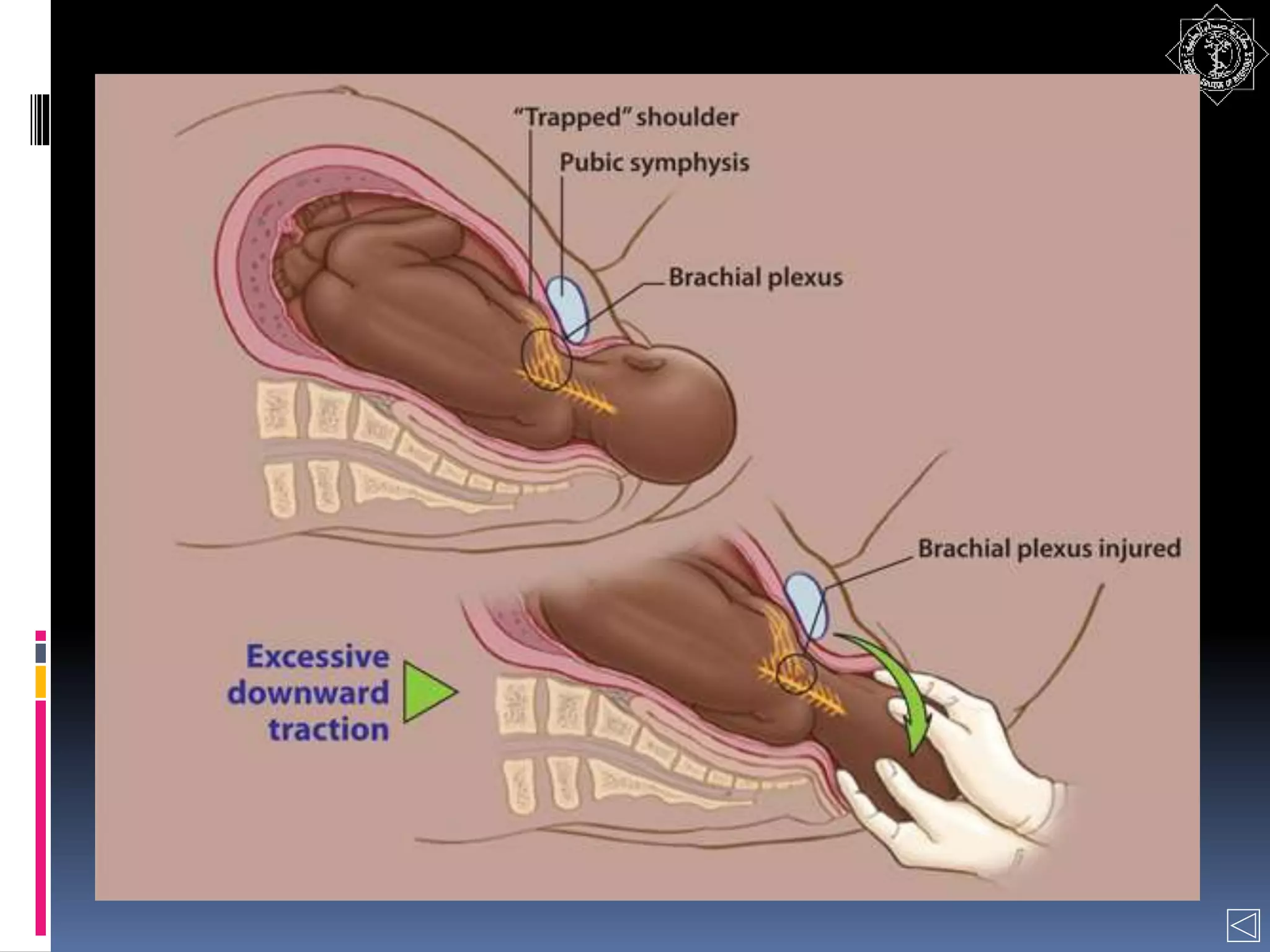
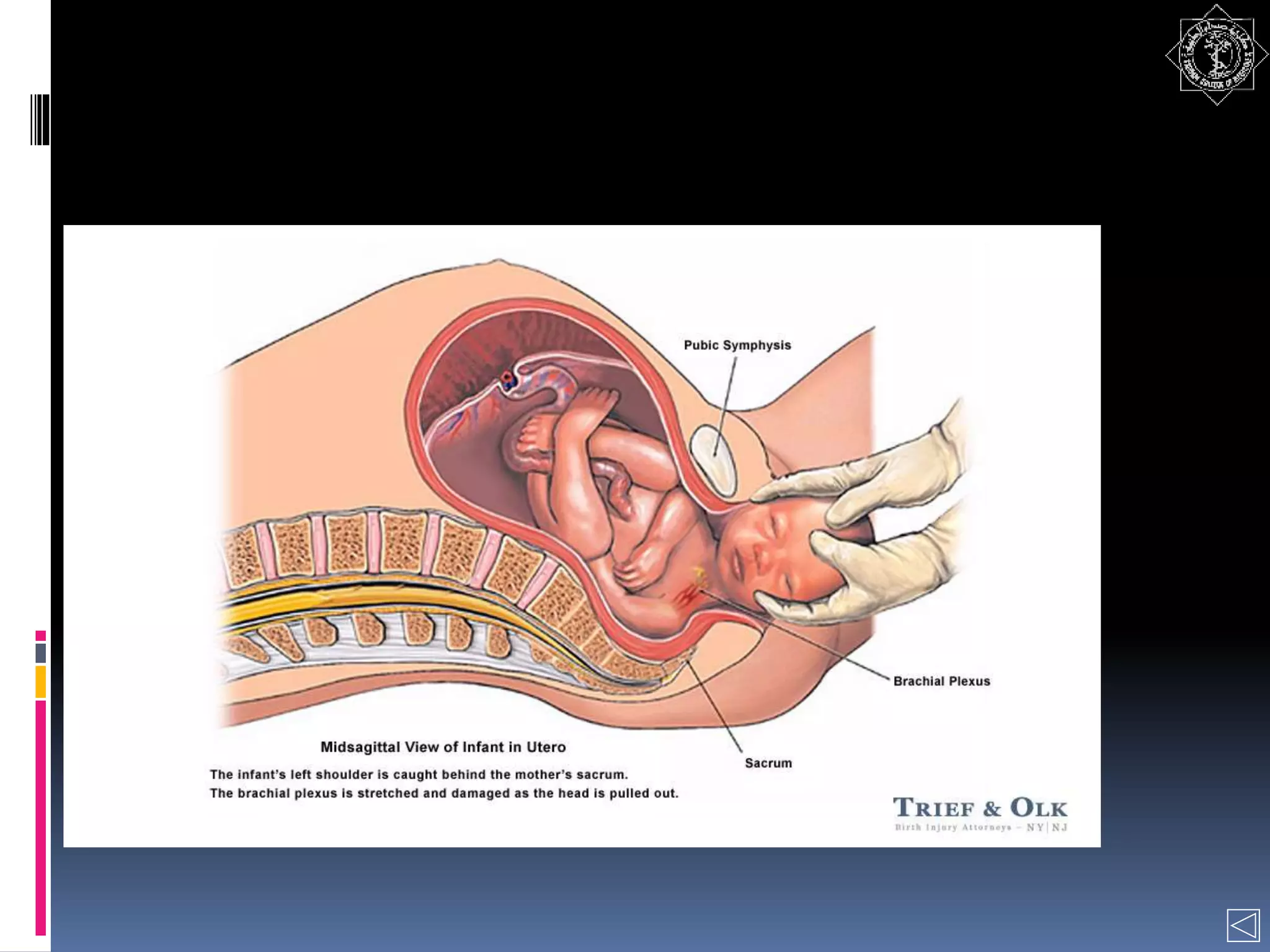
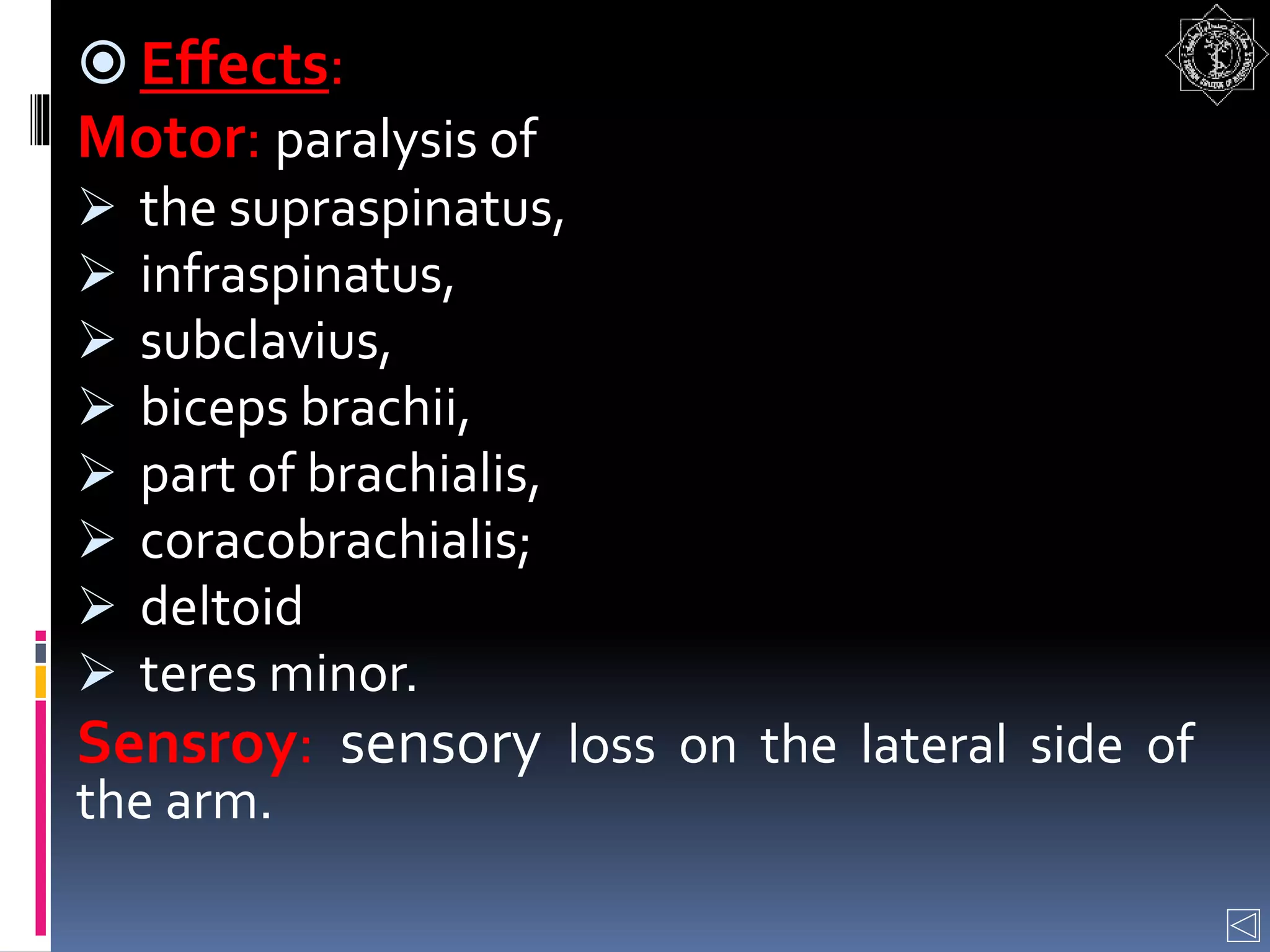
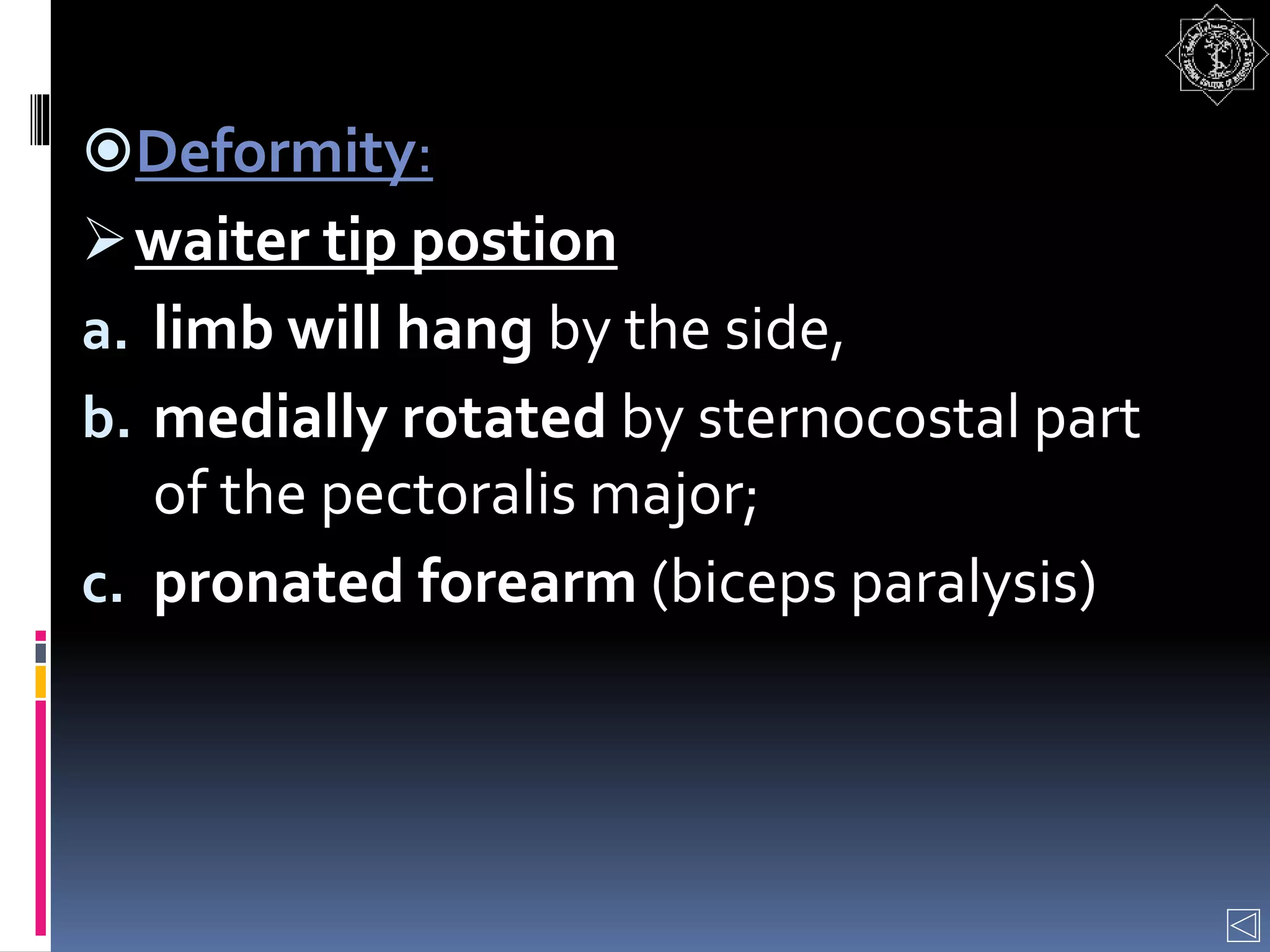
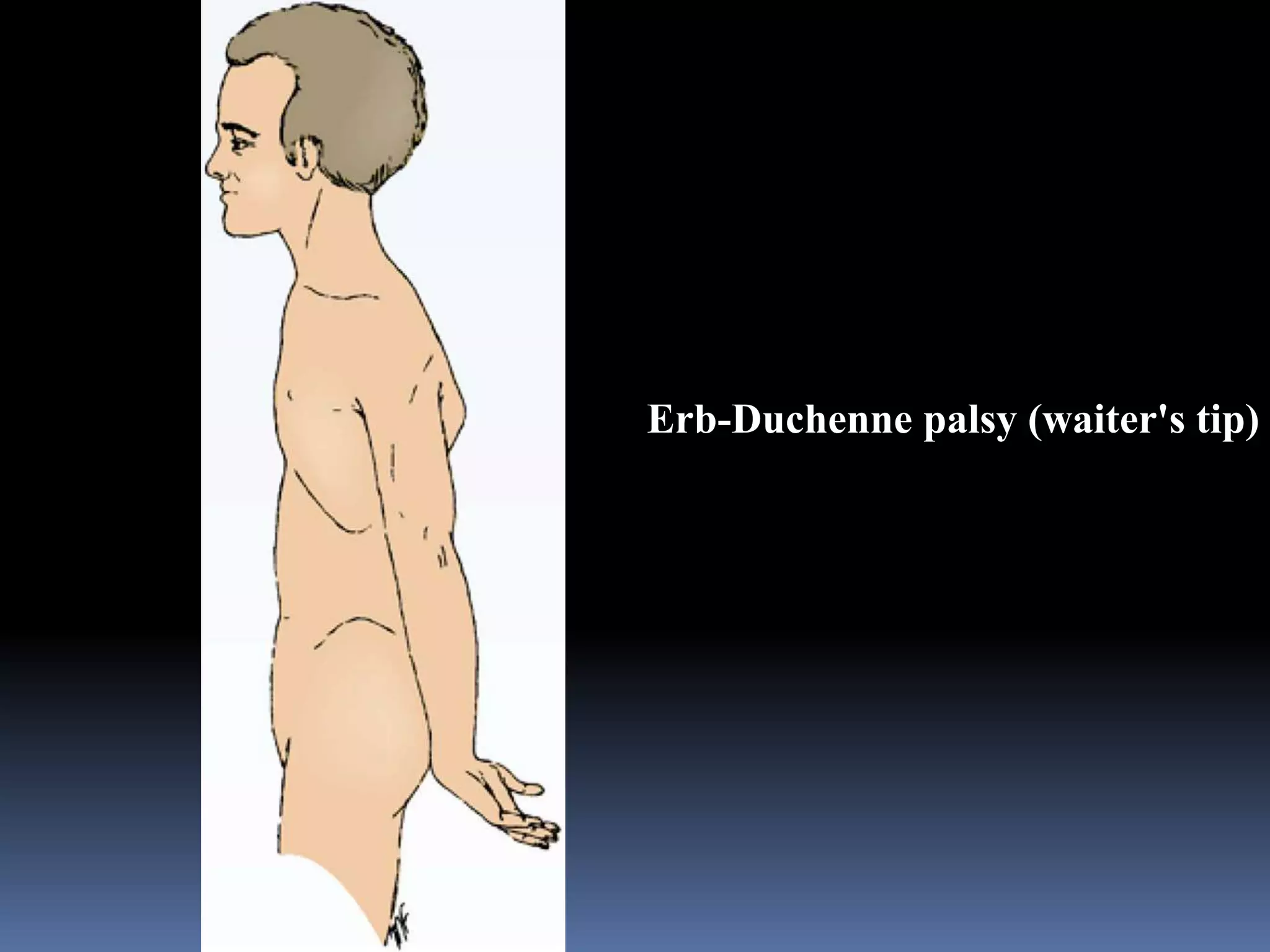
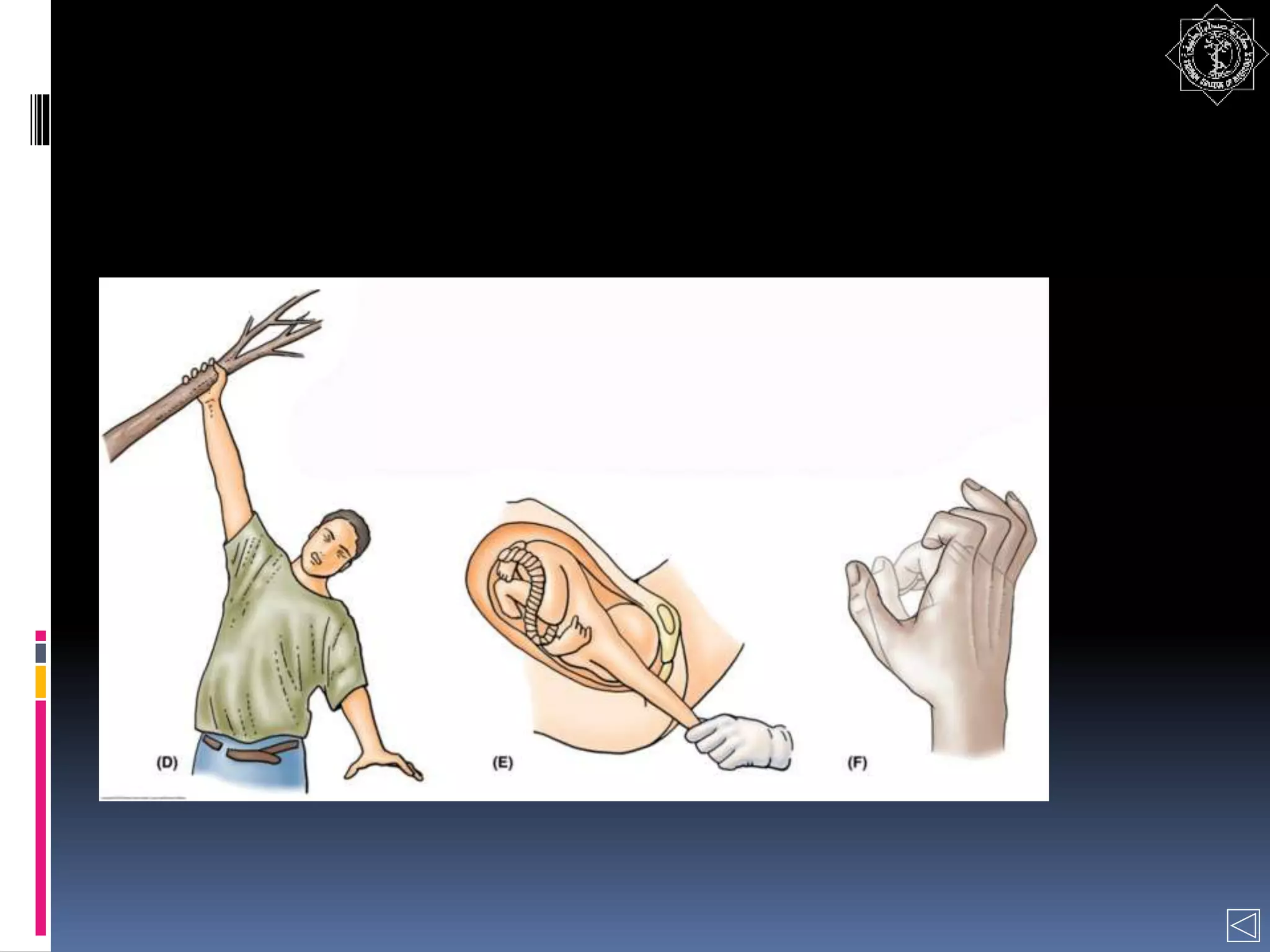
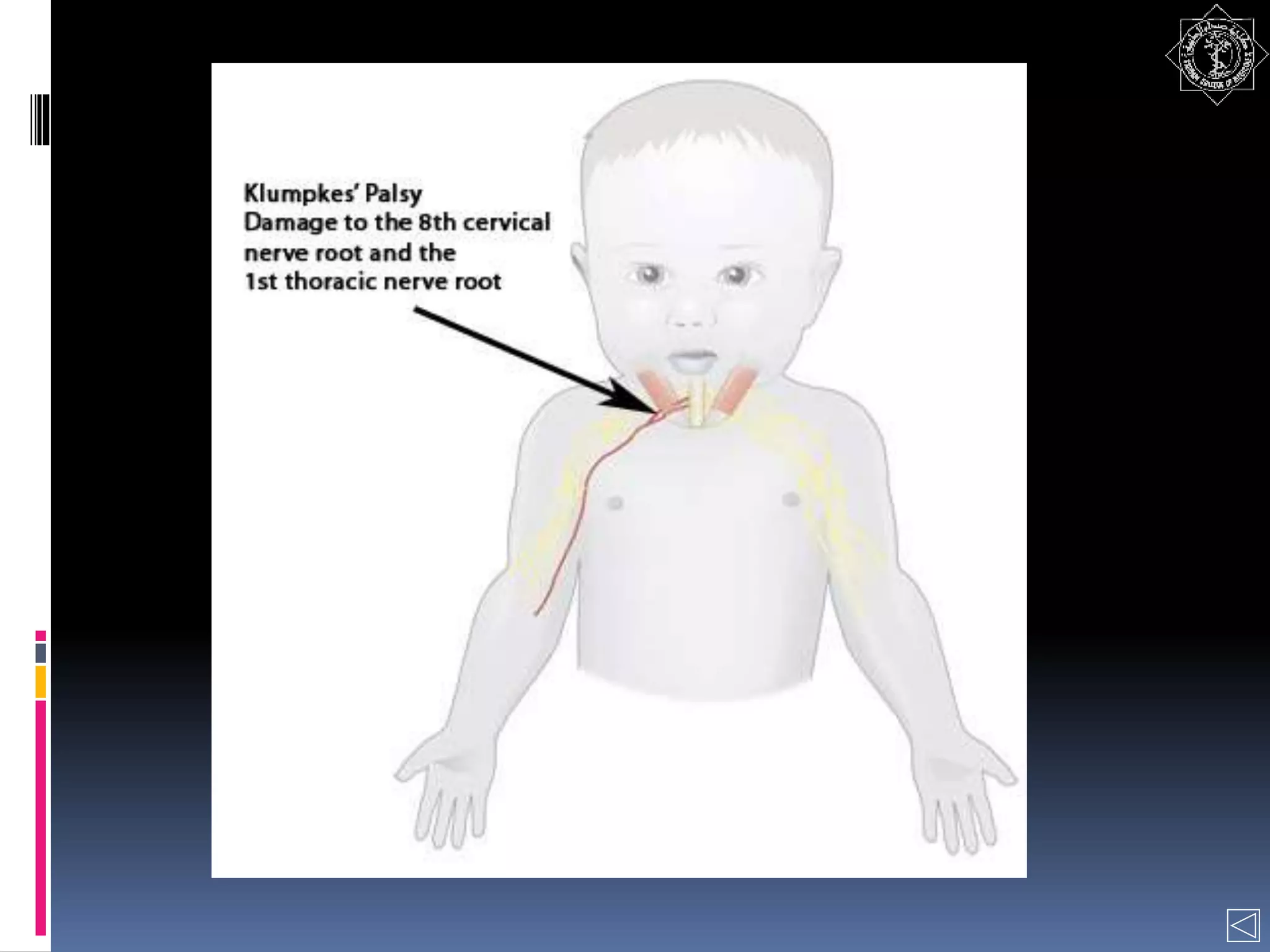
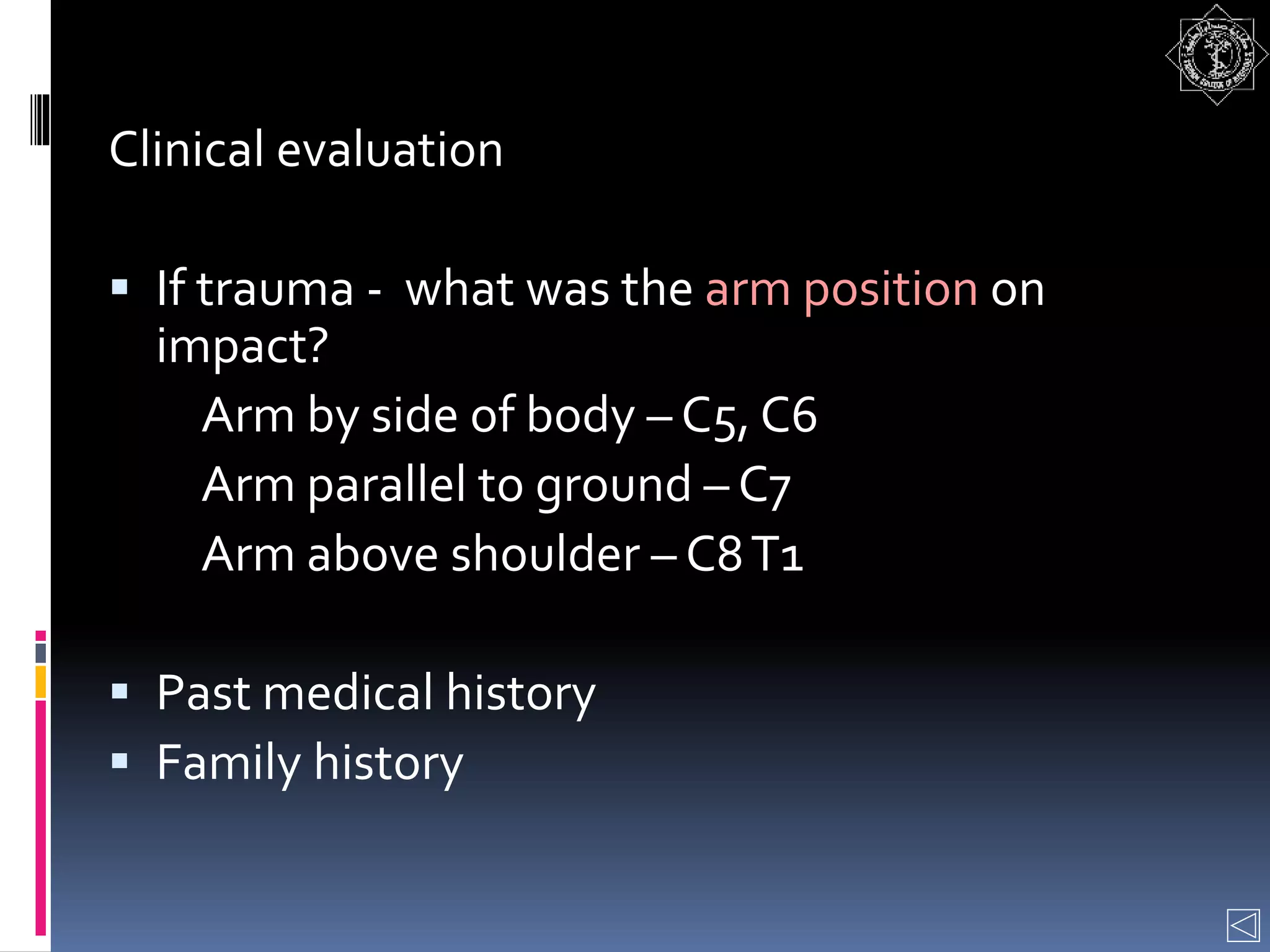
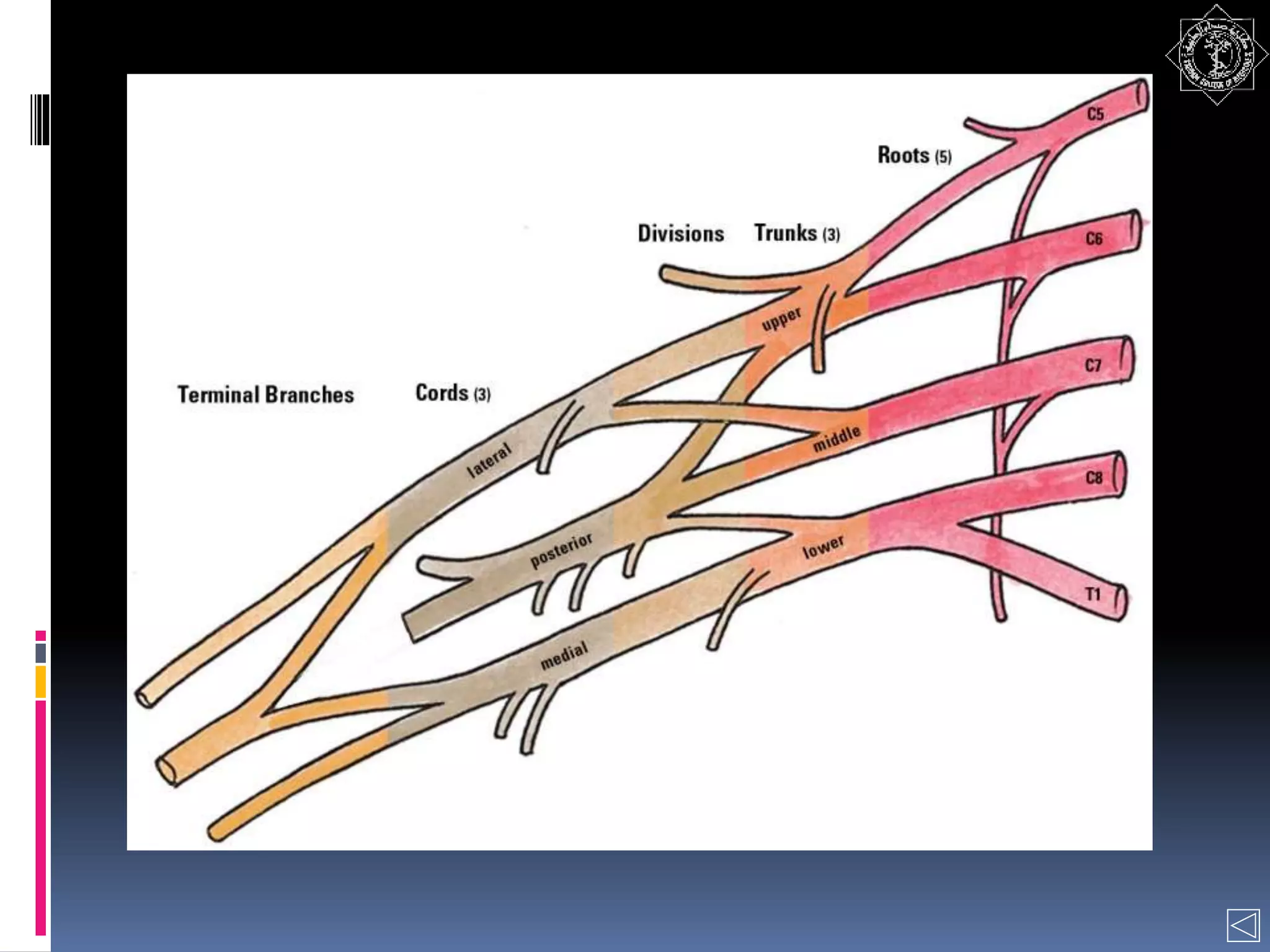
The brachial plexus is a network of nerves that originates from the cervical spinal nerves C5-T1 and supplies the upper limb. It has 5 roots which combine to form 3 trunks, then each trunk divides into anterior and posterior divisions which combine to form cords around the axillary artery. The cords give off many branches that innervate the muscles and skin of the upper limb. Injuries can occur from trauma or during childbirth and cause characteristic patterns of weakness depending on the level of injury along the plexus.