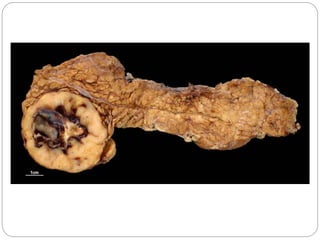
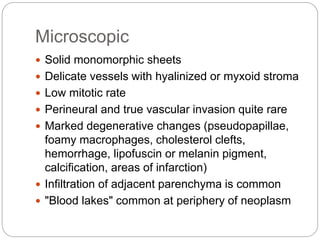
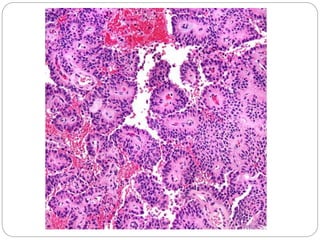
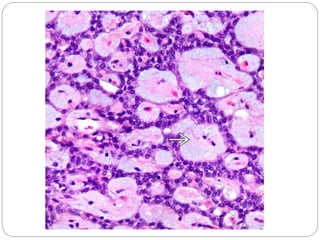
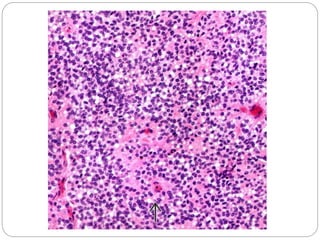
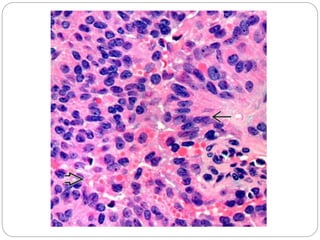
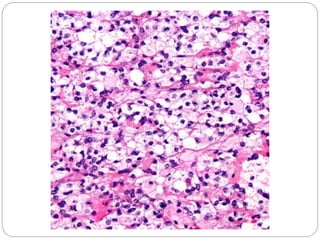
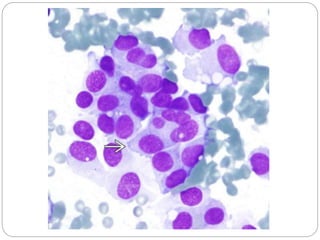
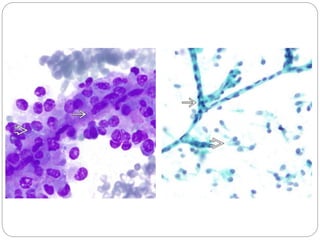
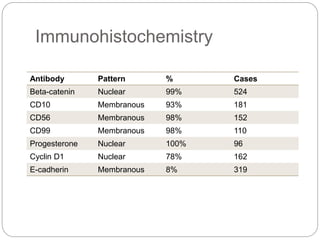
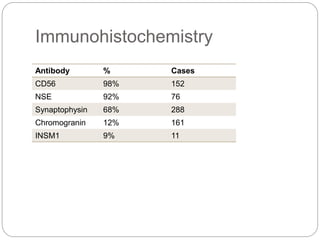
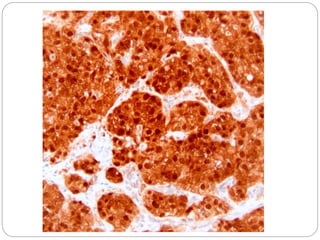
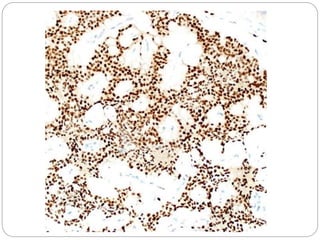
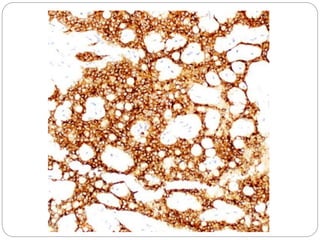
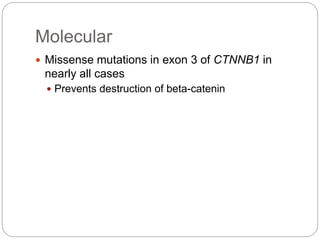
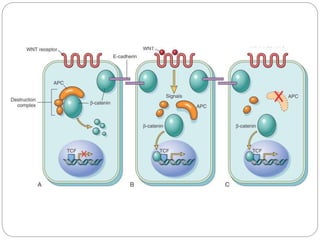
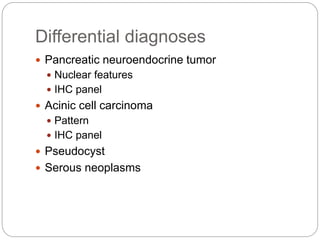
Solid pseudopapillary neoplasm of the pancreas is a low-grade malignant tumor most common in young women. It is characterized by mutations in the CTNNB1 gene in 90-100% of cases. Clinically, it presents as an indolent, well-circumscribed solid and cystic mass distributed throughout the pancreas. Microscopically, it displays monomorphic sheets and pseudopapillary structures with degenerative changes and perineural/vascular invasion is rare. Immunohistochemistry is positive for beta-catenin, CD10, CD56 and other markers. Prognosis is generally excellent even with rare metastases.