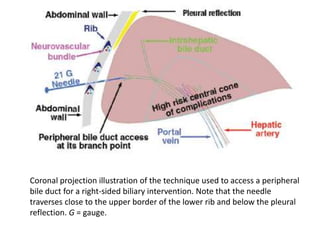
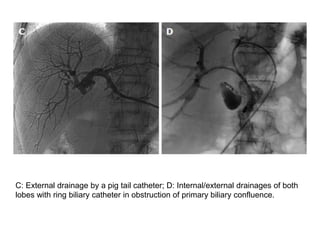
This document discusses percutaneous transhepatic biliary drainage (PTBD) for the treatment of malignant biliary obstruction. PTBD involves puncturing the obstructed bile duct under imaging guidance and placing a drainage catheter to decompress the biliary system. It is indicated for palliation or as a preoperative procedure. Complications can include pain, bile leaks, hemorrhage, cholangitis, and stent blockage over time. The procedure involves imaging to plan access, puncturing the bile duct with a needle, placing a wire and catheter across the stricture, and sometimes placing a stent to maintain drainage.