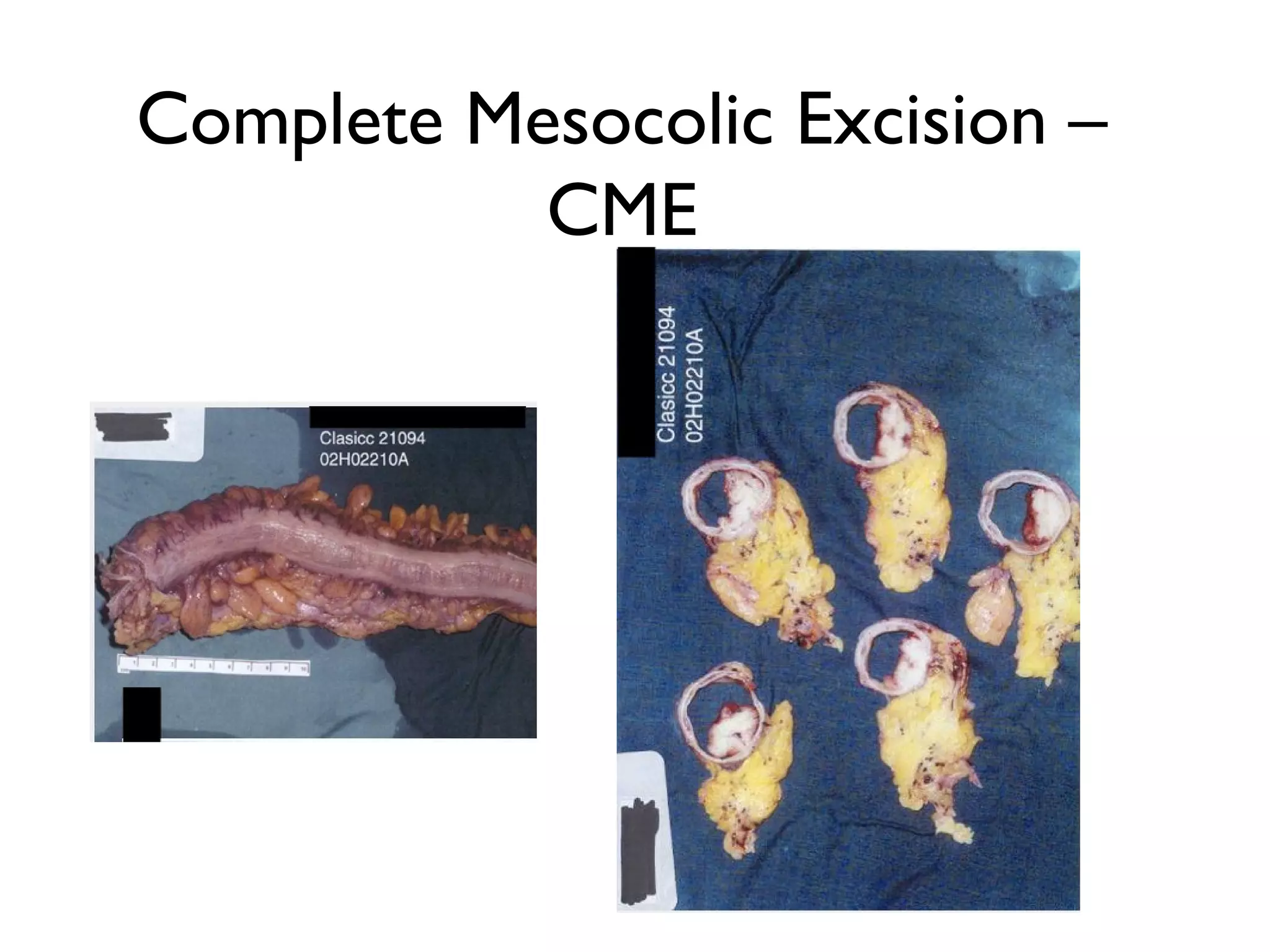
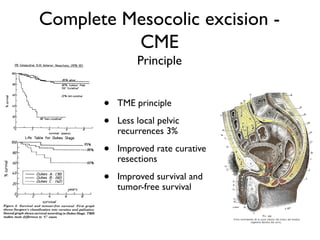
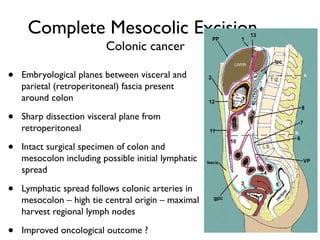
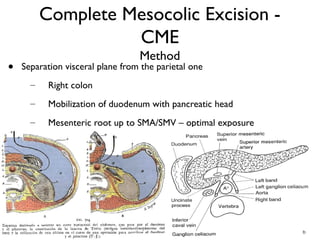
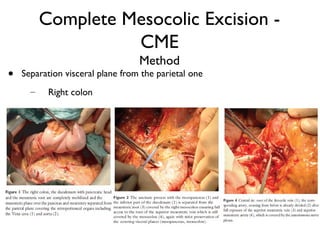
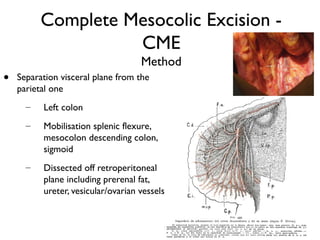
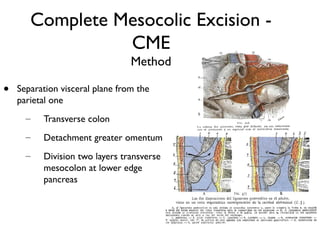
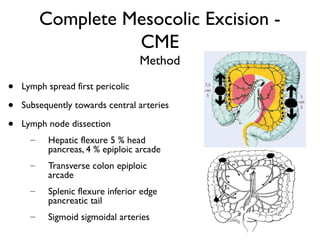
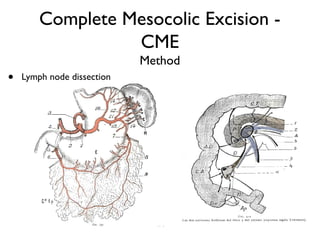
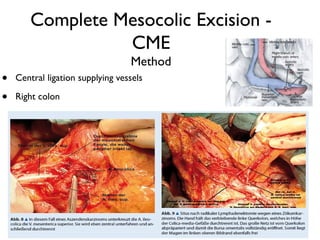
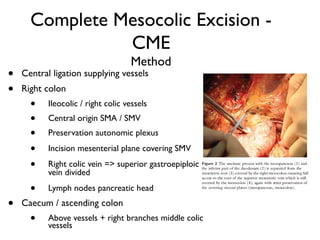
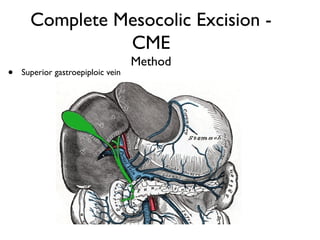
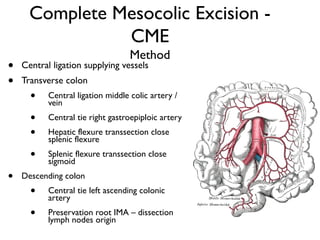
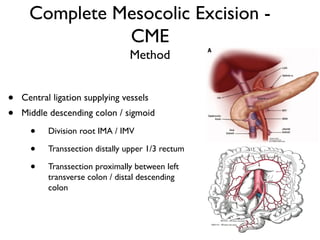
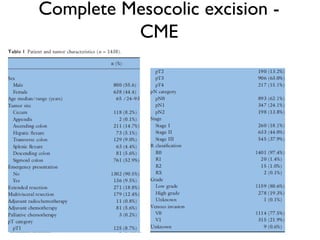
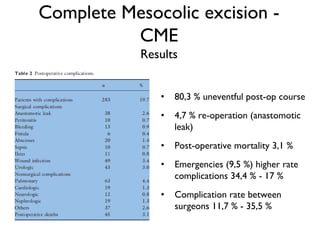
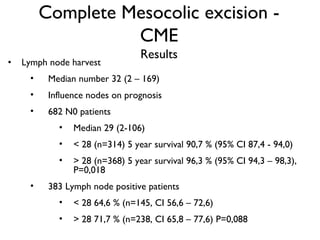
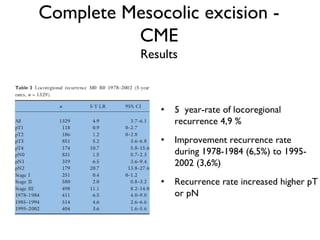
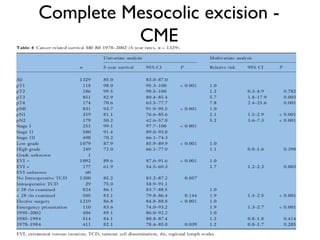
Complete Mesocolic Excision (CME) is a surgical technique for colon cancer based on Total Mesorectal Excision principles for rectal cancer. CME involves sharp dissection along embryonic planes between the visceral and parietal fascia to remove the colon and intact mesocolon lymphovascular package. Central ligation of supplying vessels also aims to maximize lymph node harvest. A study of over 1,300 colon cancer patients who underwent CME found improved 5-year cancer survival rates and reduced local recurrence compared to previous techniques, correlated with higher lymph node counts. CME principles include producing an intact specimen and maximizing lymph node dissection for improved oncologic outcomes.