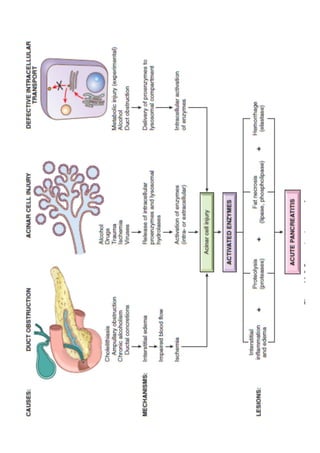
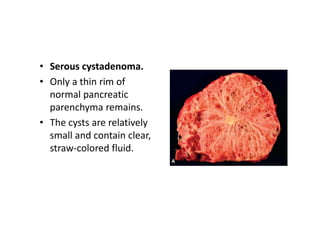
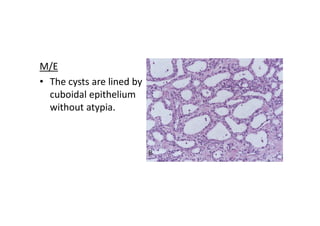
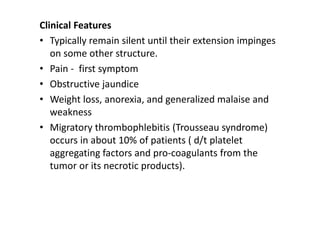
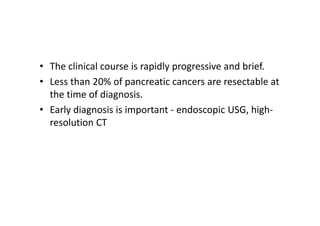
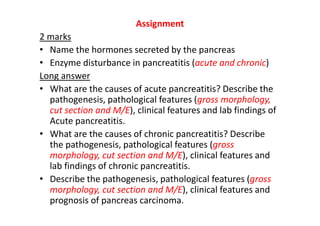
The pancreas is a critical organ with both endocrine and exocrine functions, primarily involved in digestion and blood sugar regulation. It can be affected by various congenital anomalies and conditions such as pancreatitis and neoplasms, leading to a range of symptoms and complications. Specific diseases include acute and chronic pancreatitis, which can cause significant abdominal pain and may lead to serious systemic issues, and pancreatic cancer, which has a high mortality rate and often remains asymptomatic until advanced.