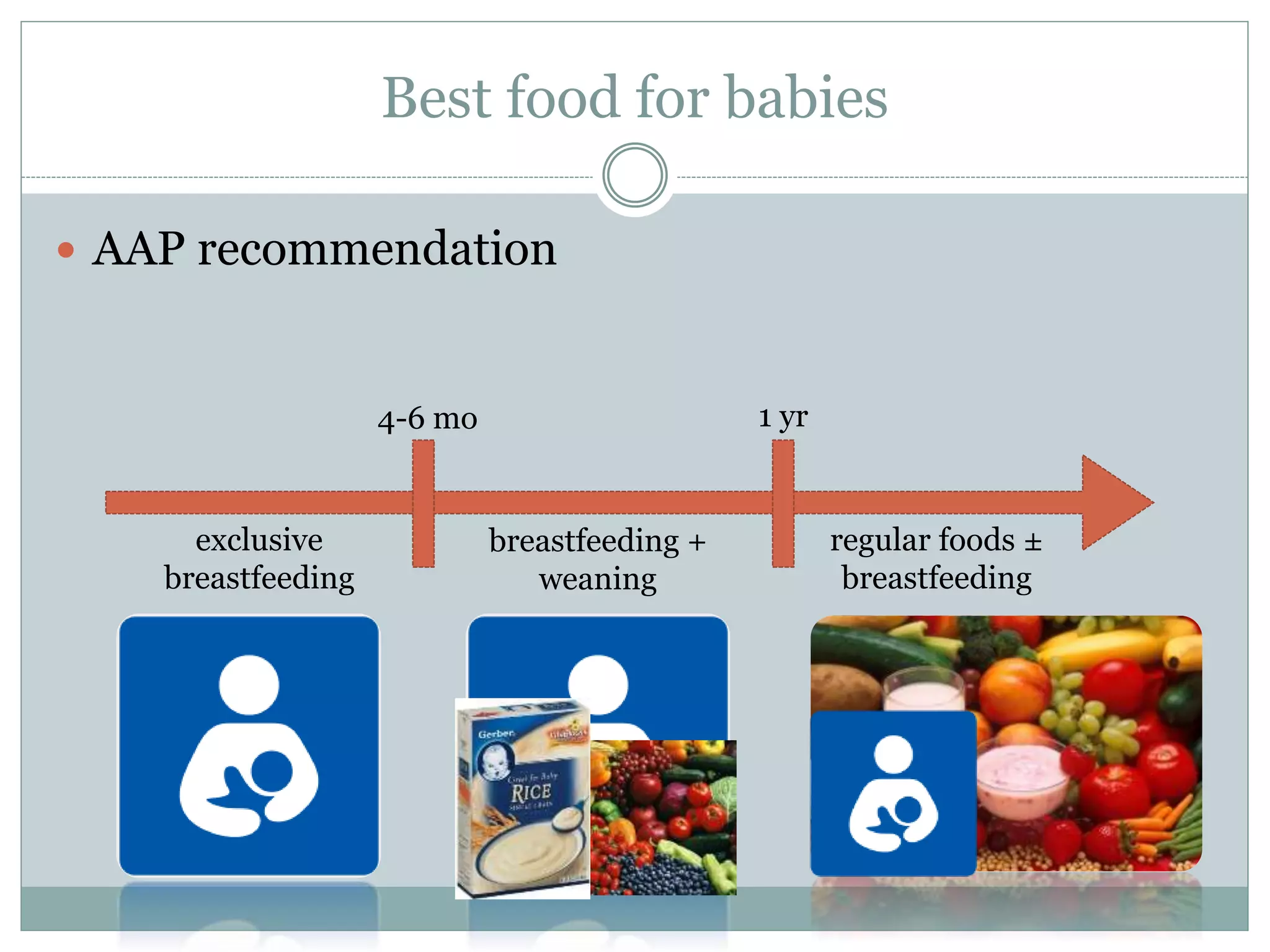
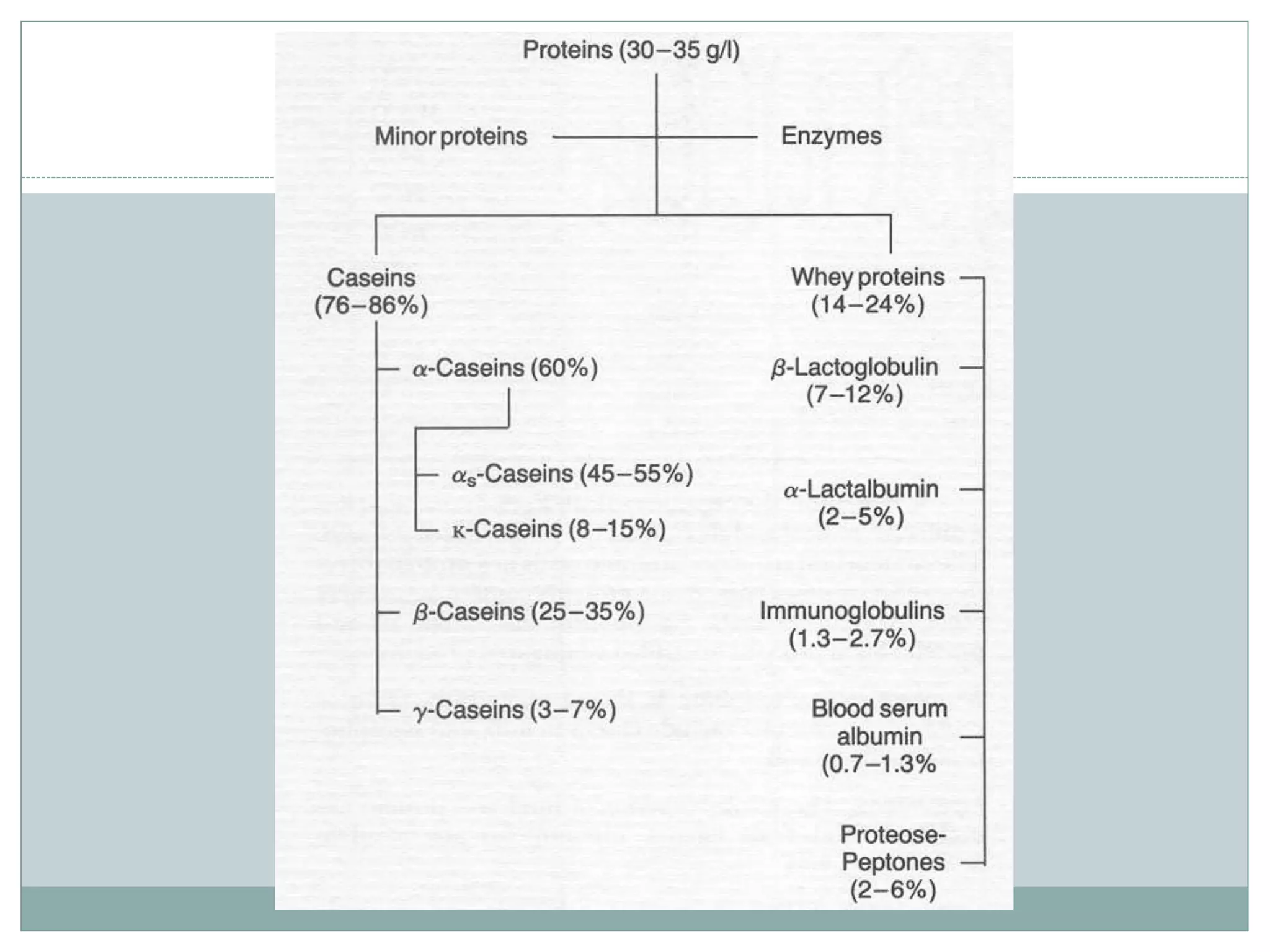
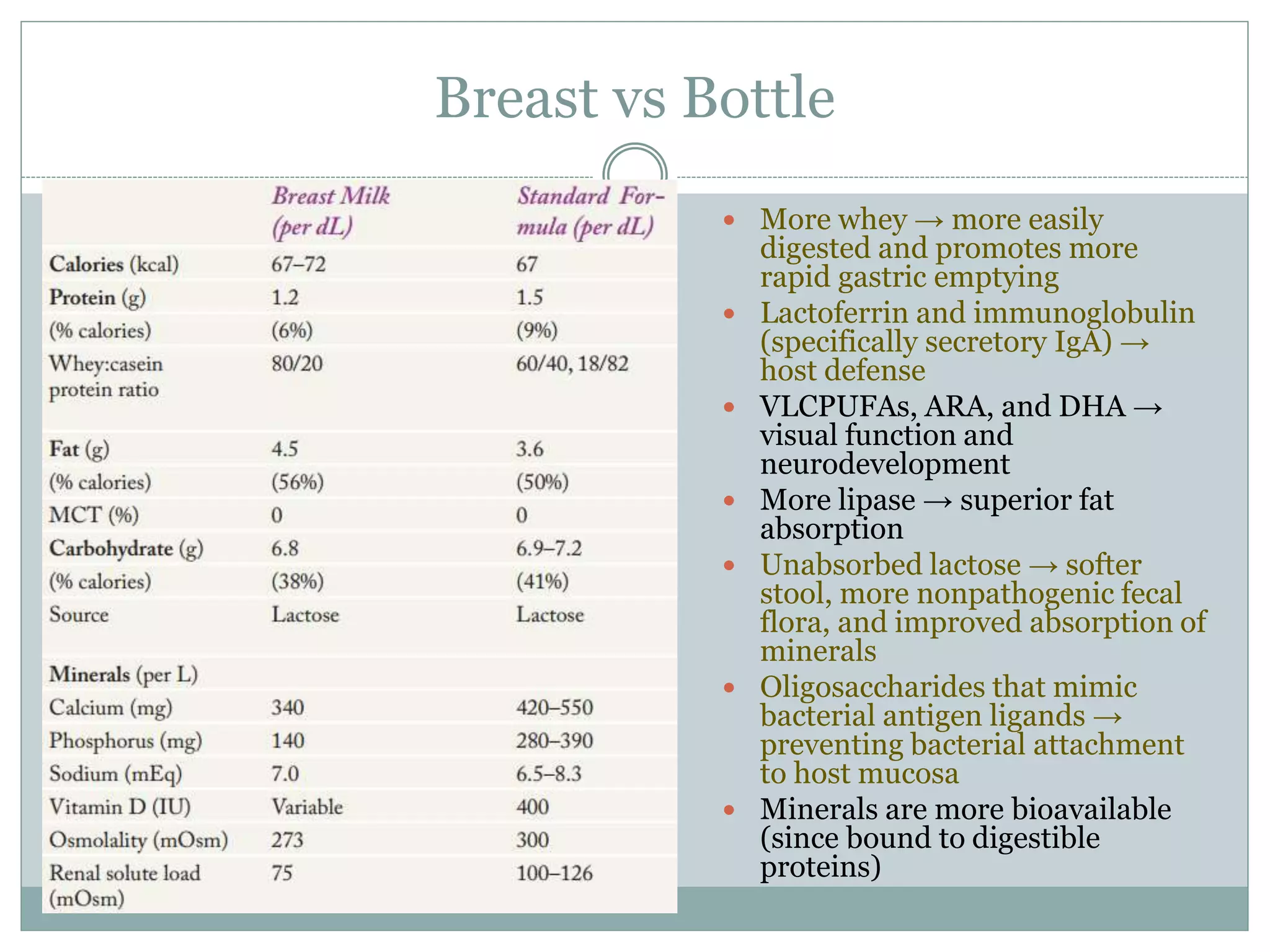
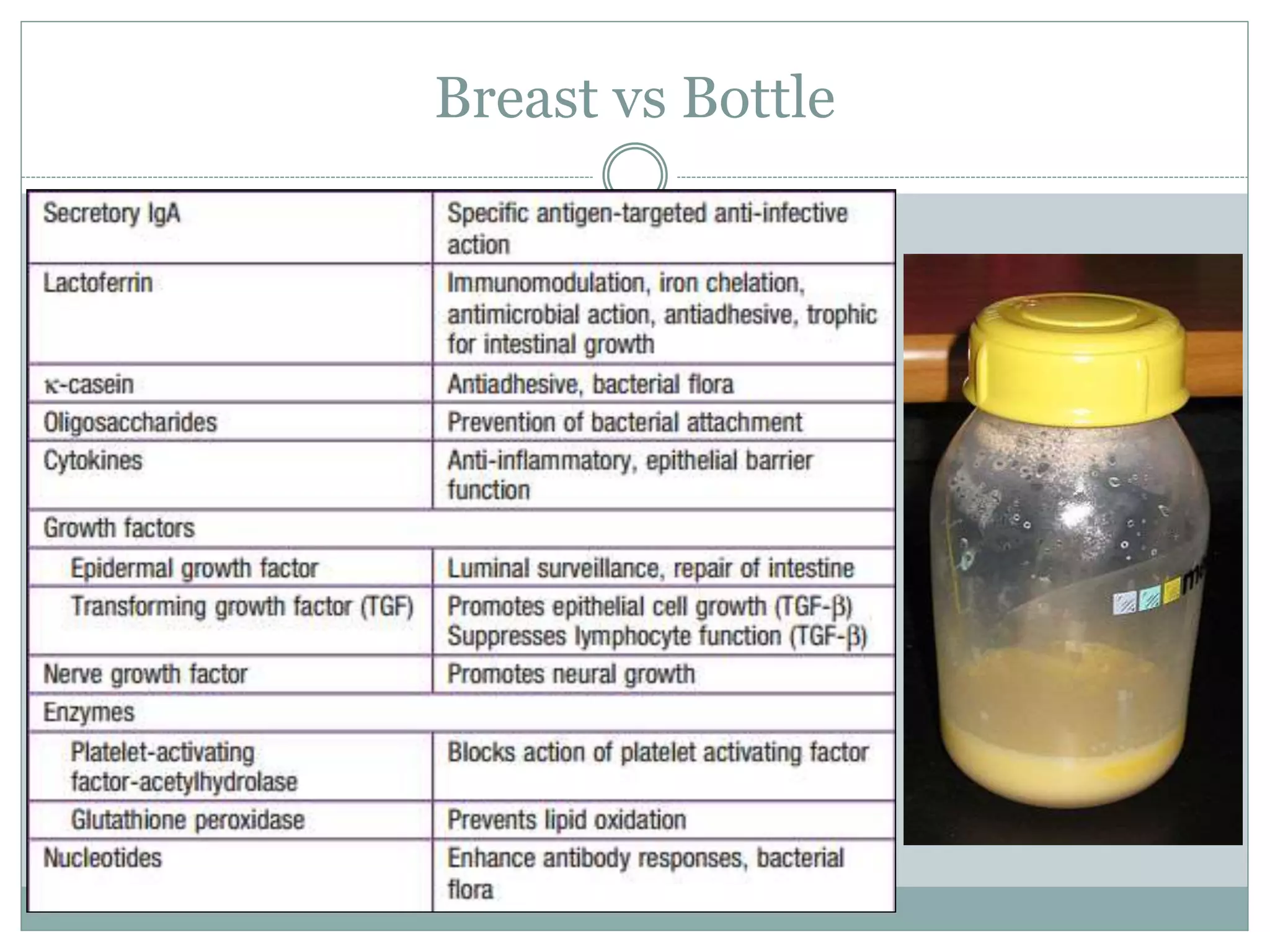
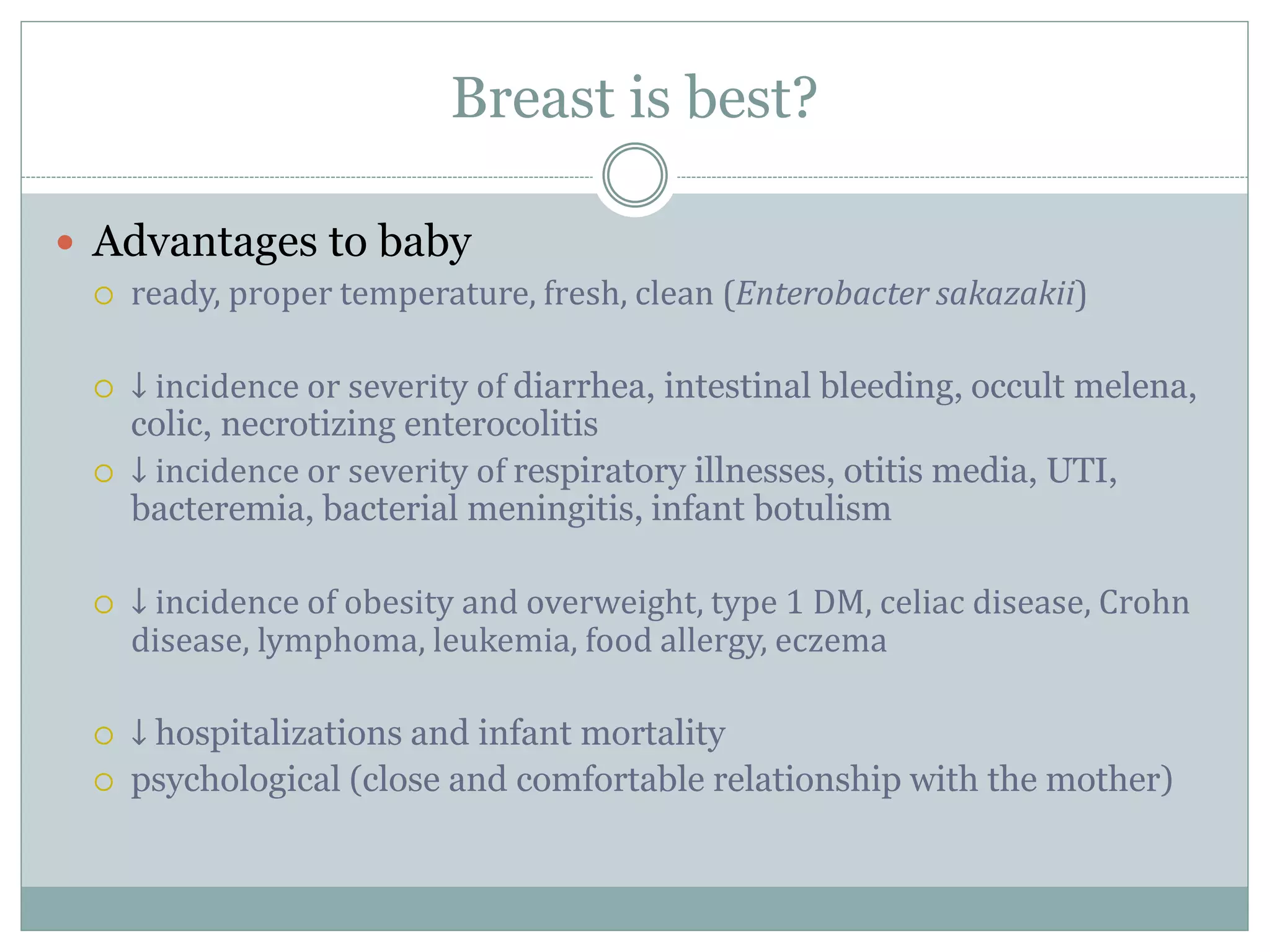
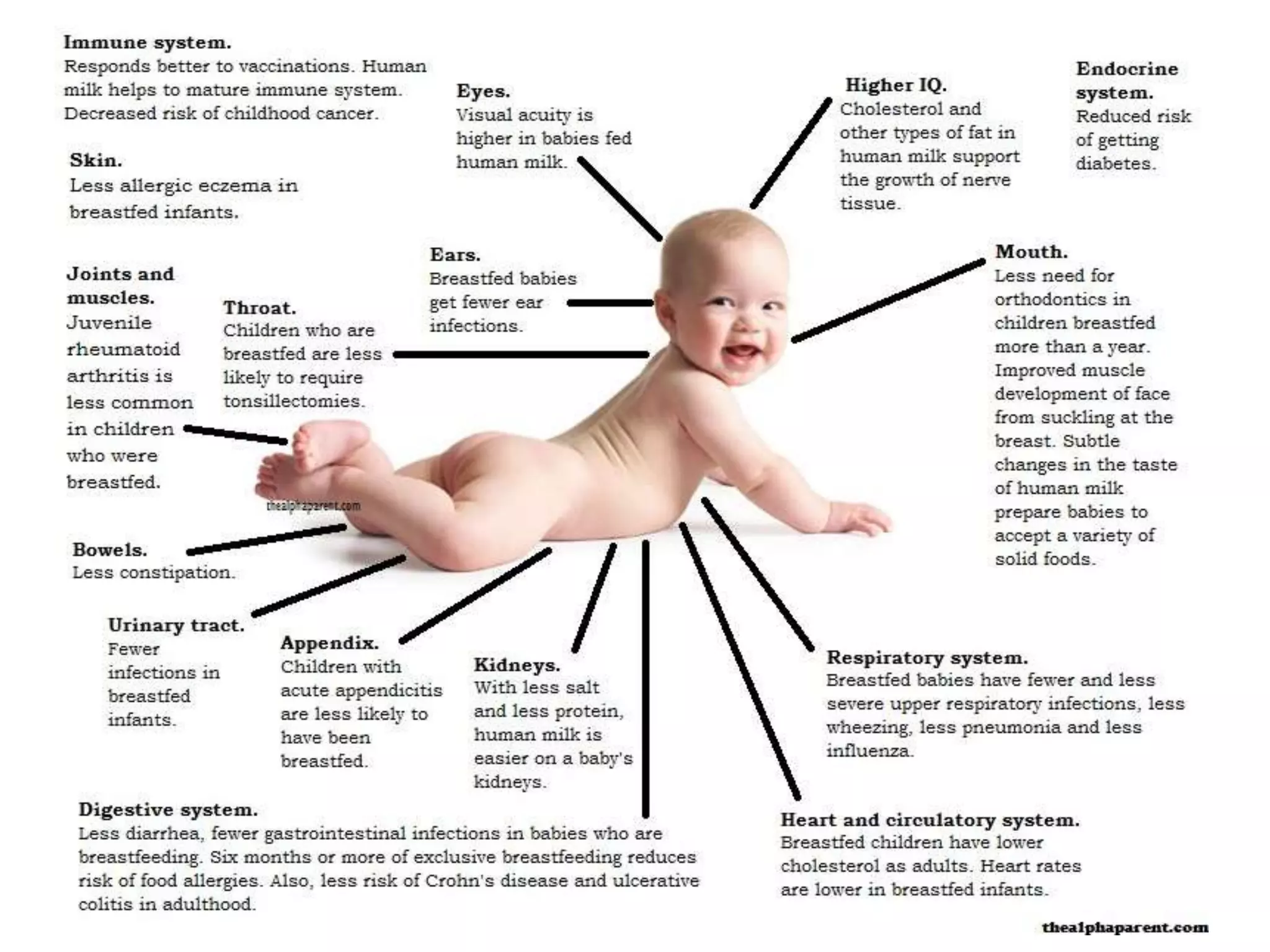
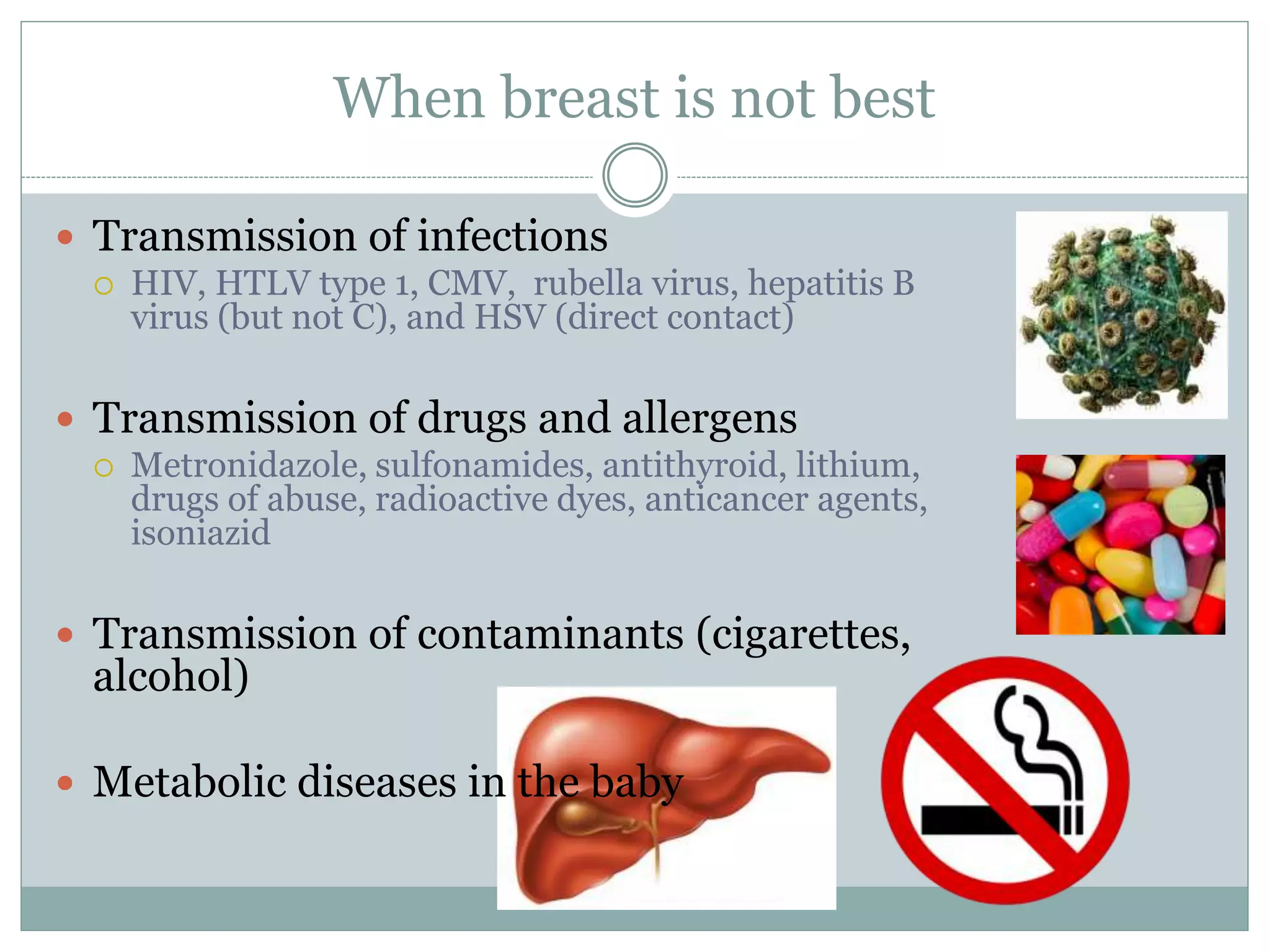
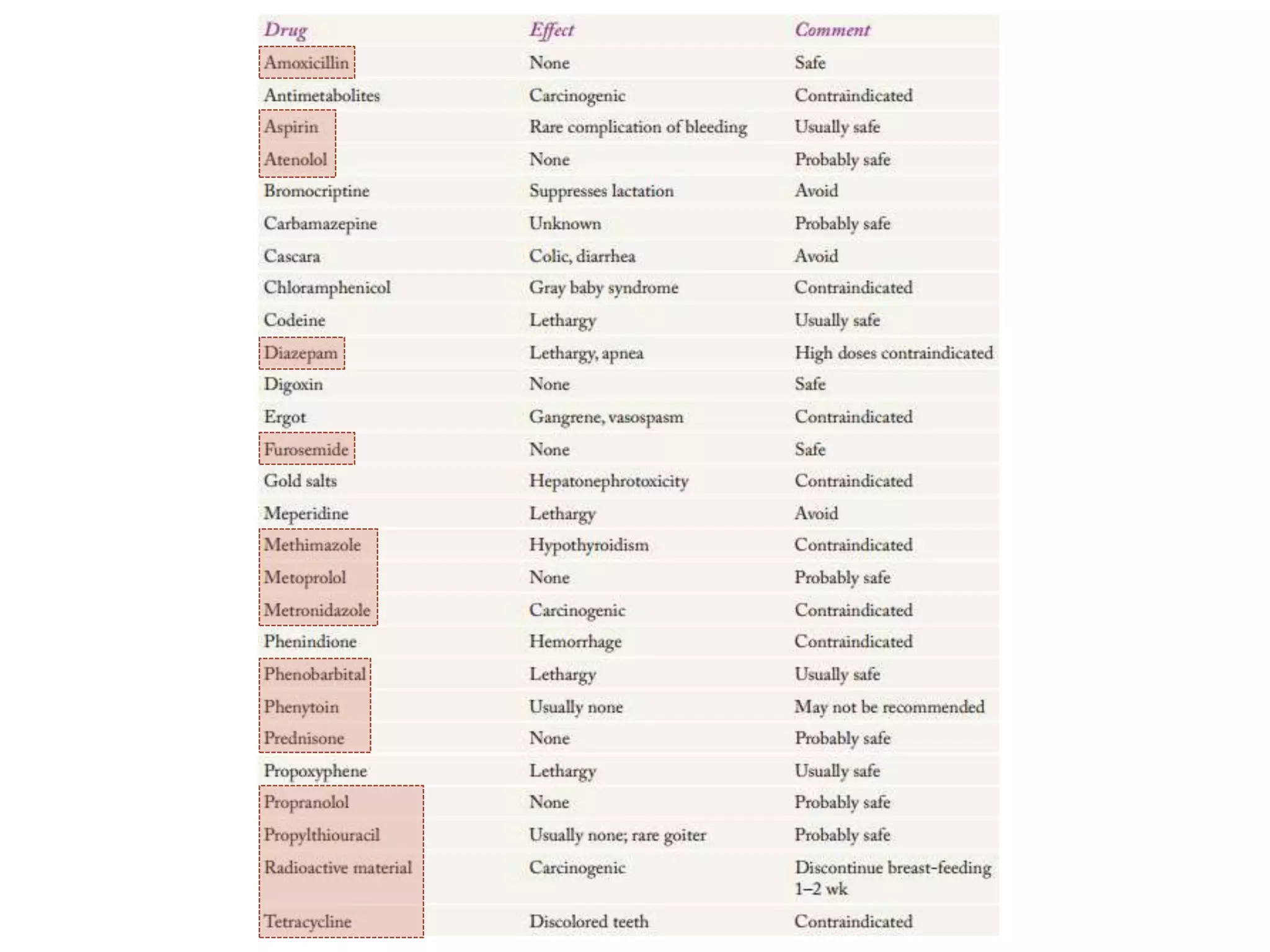
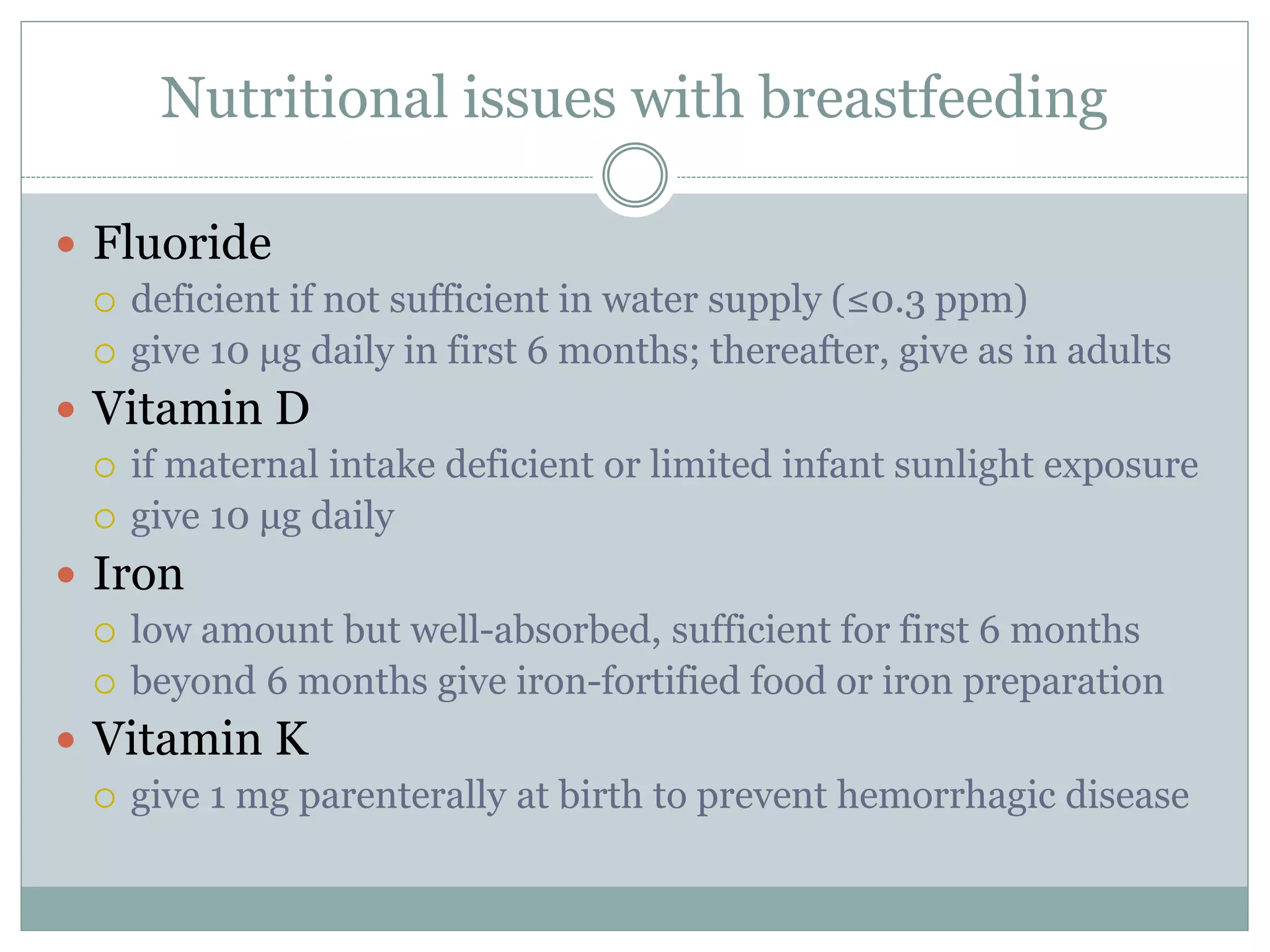
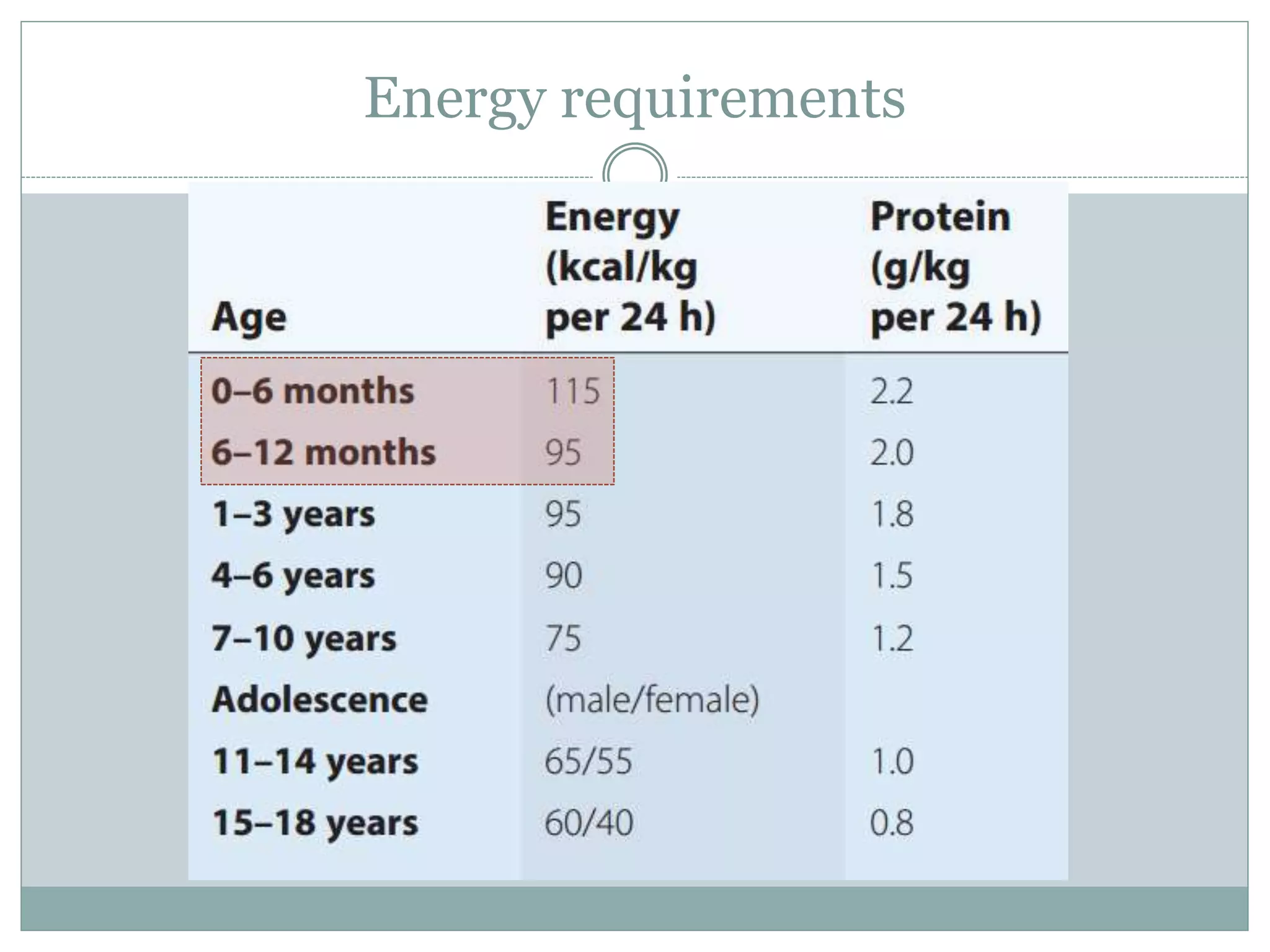
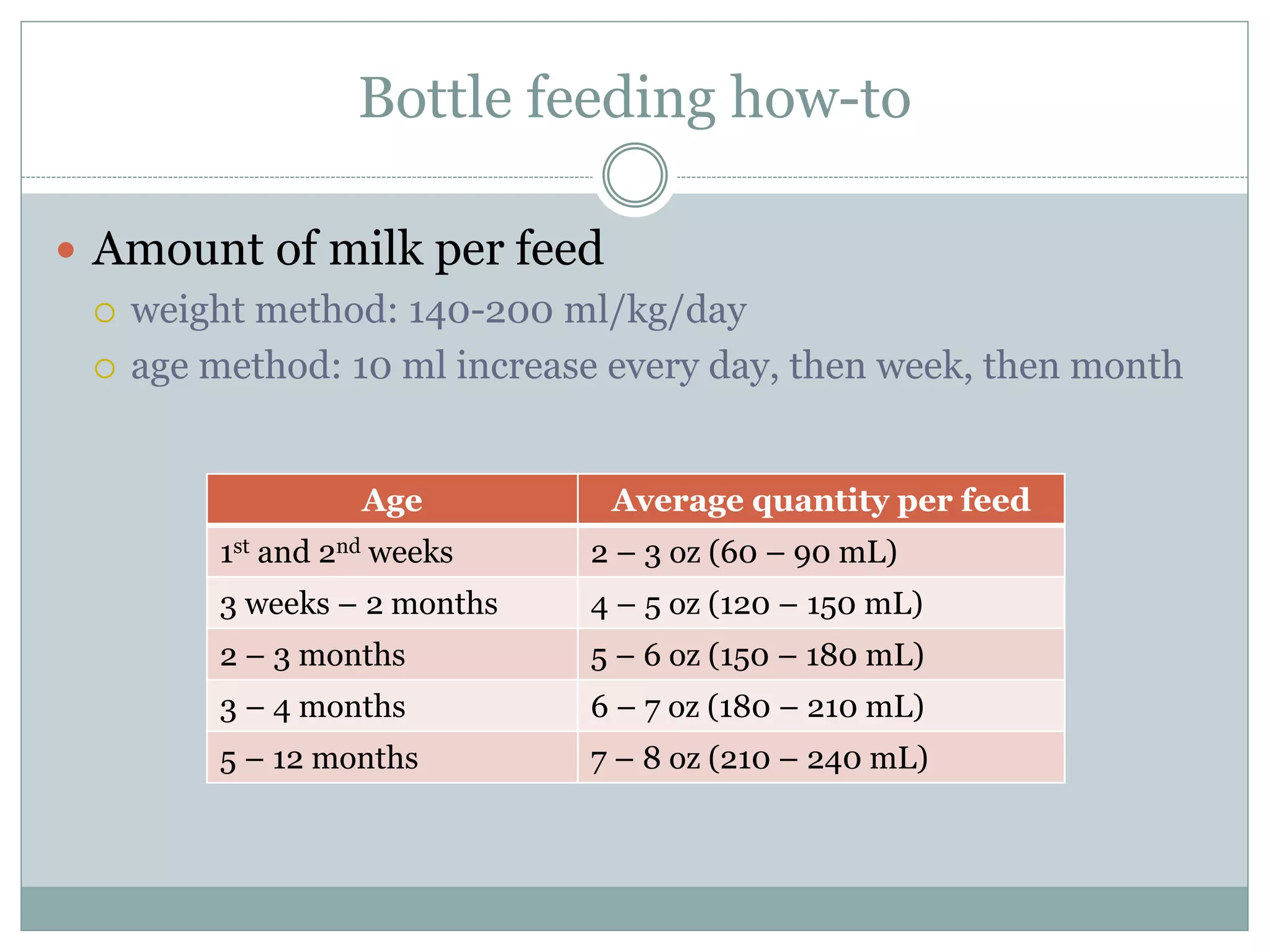
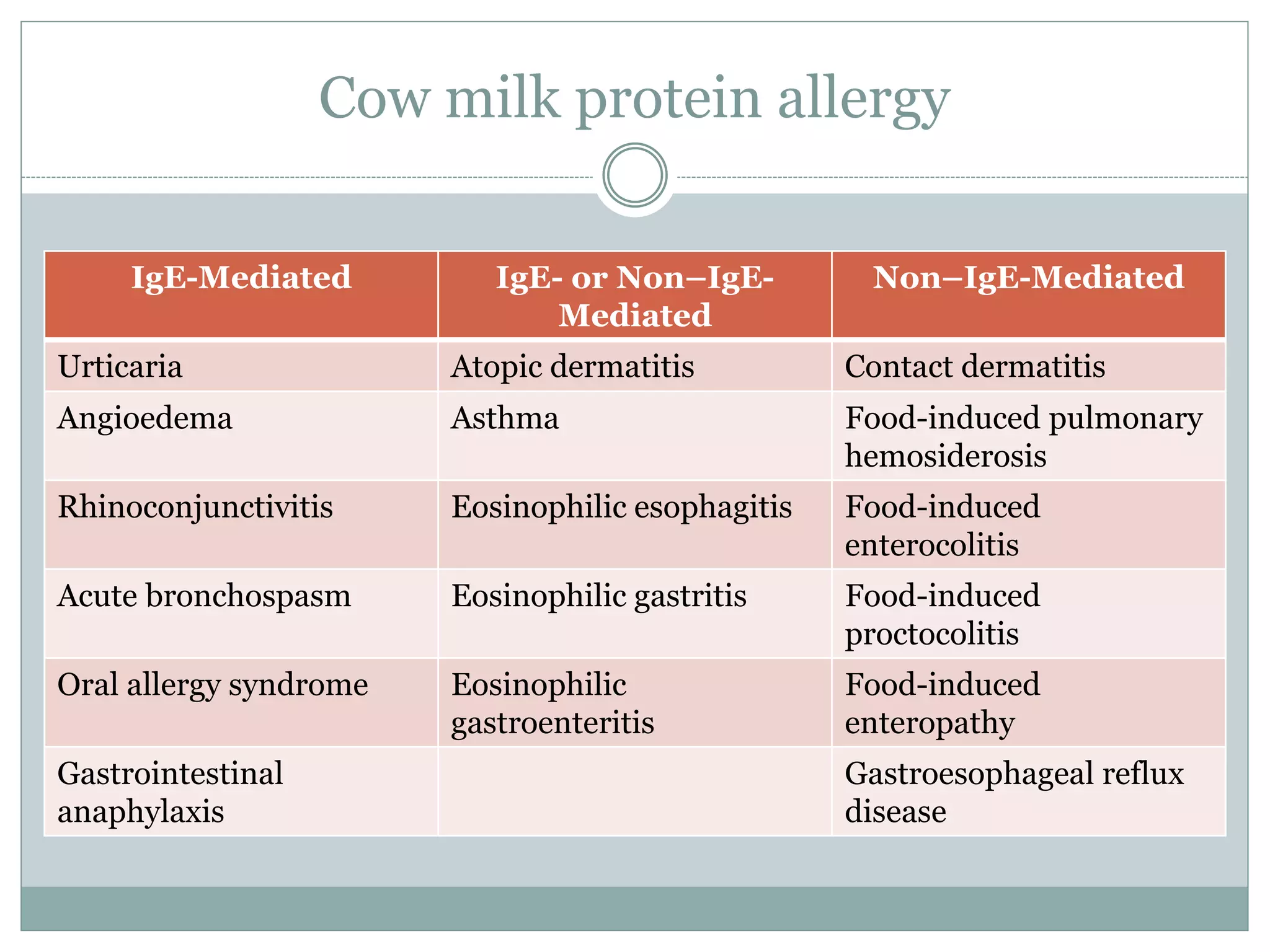
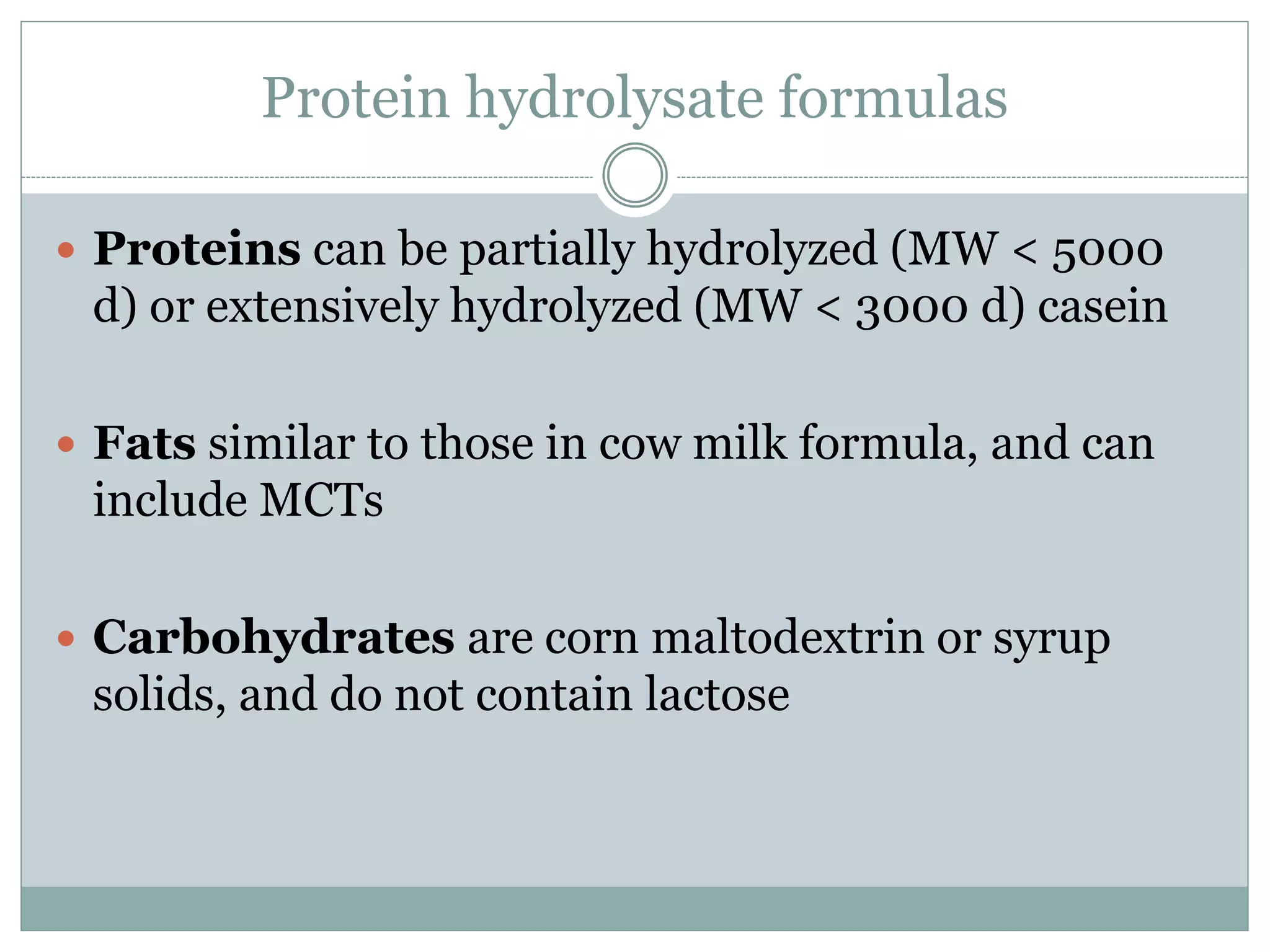
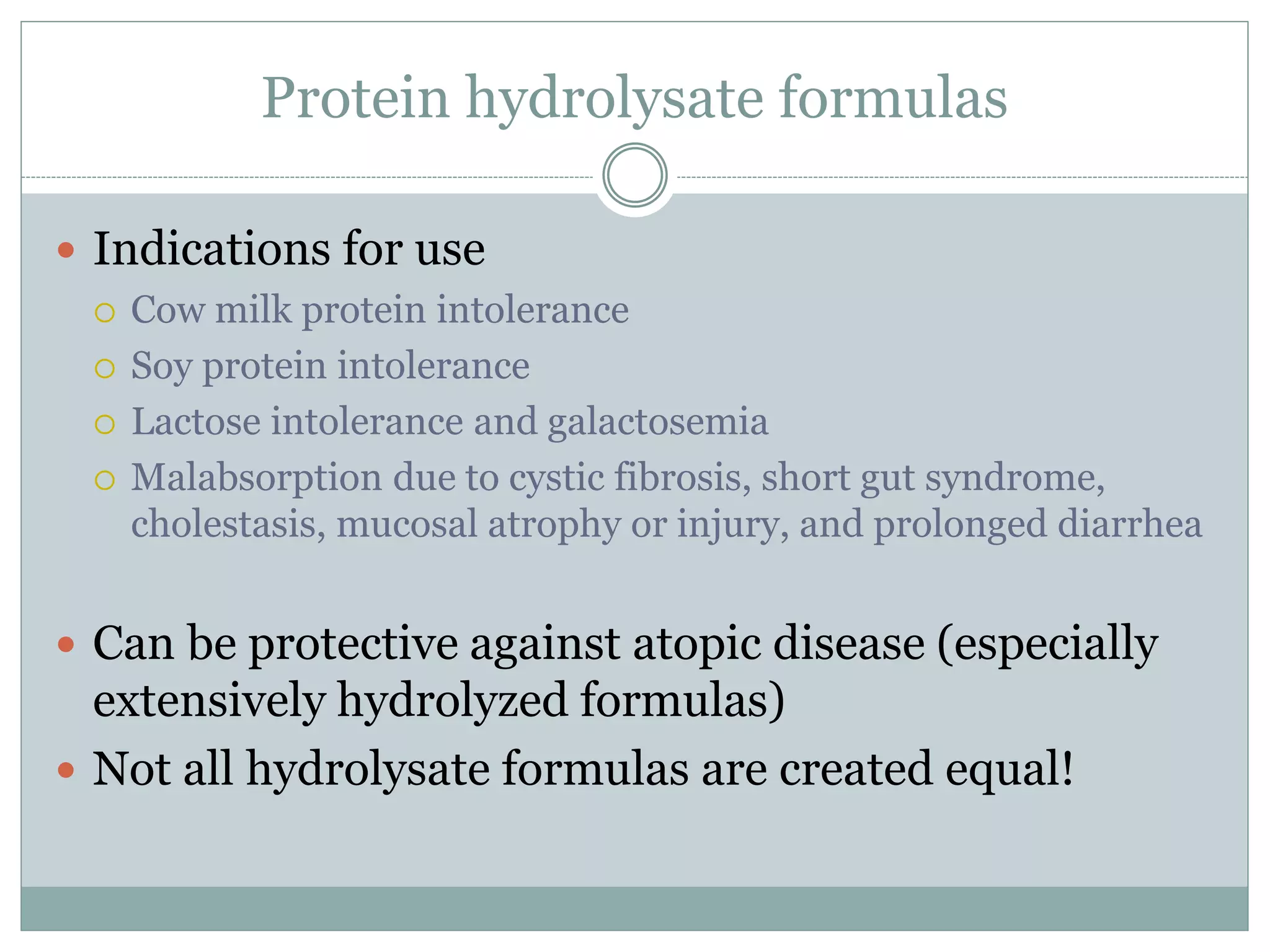
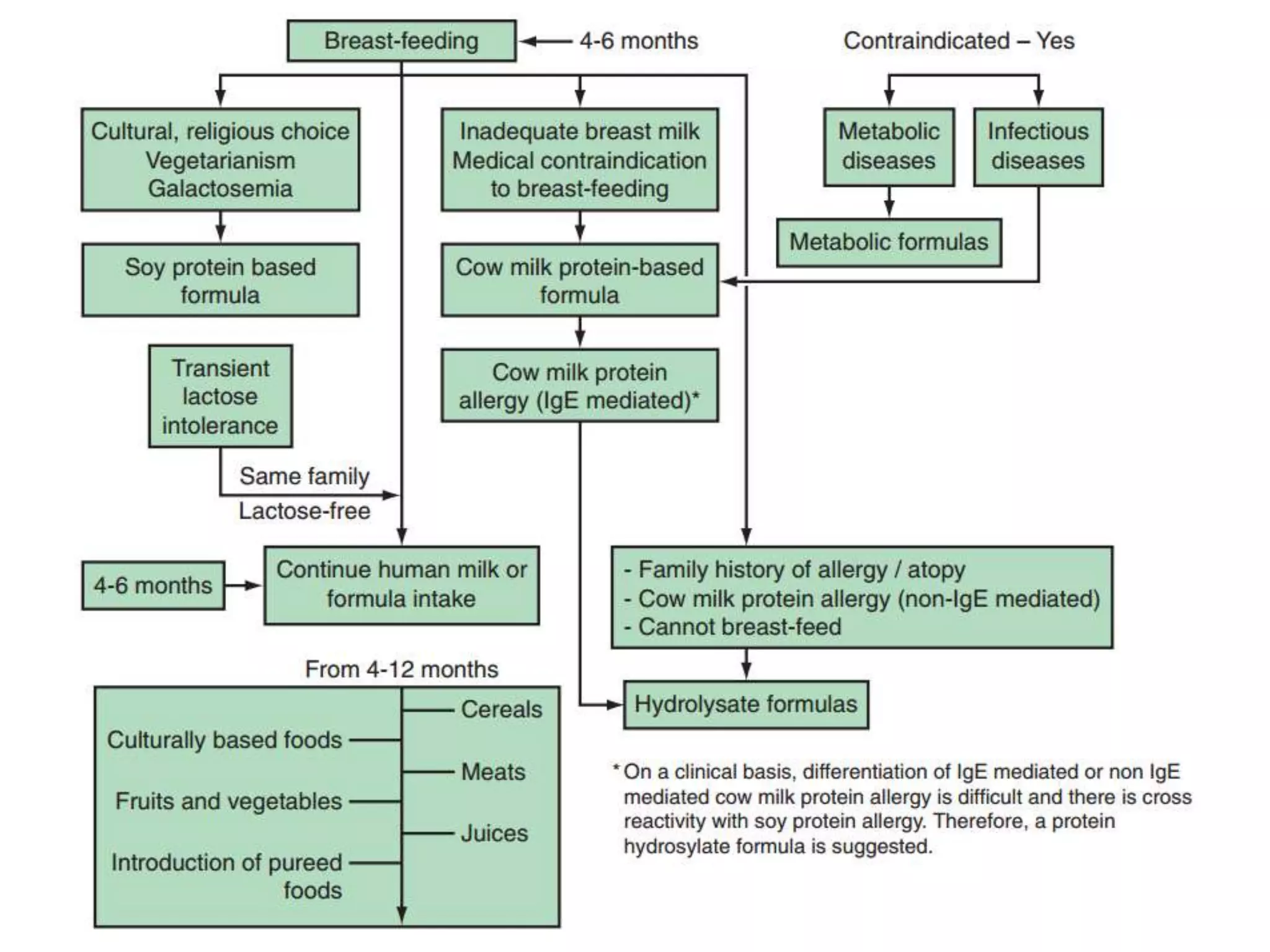
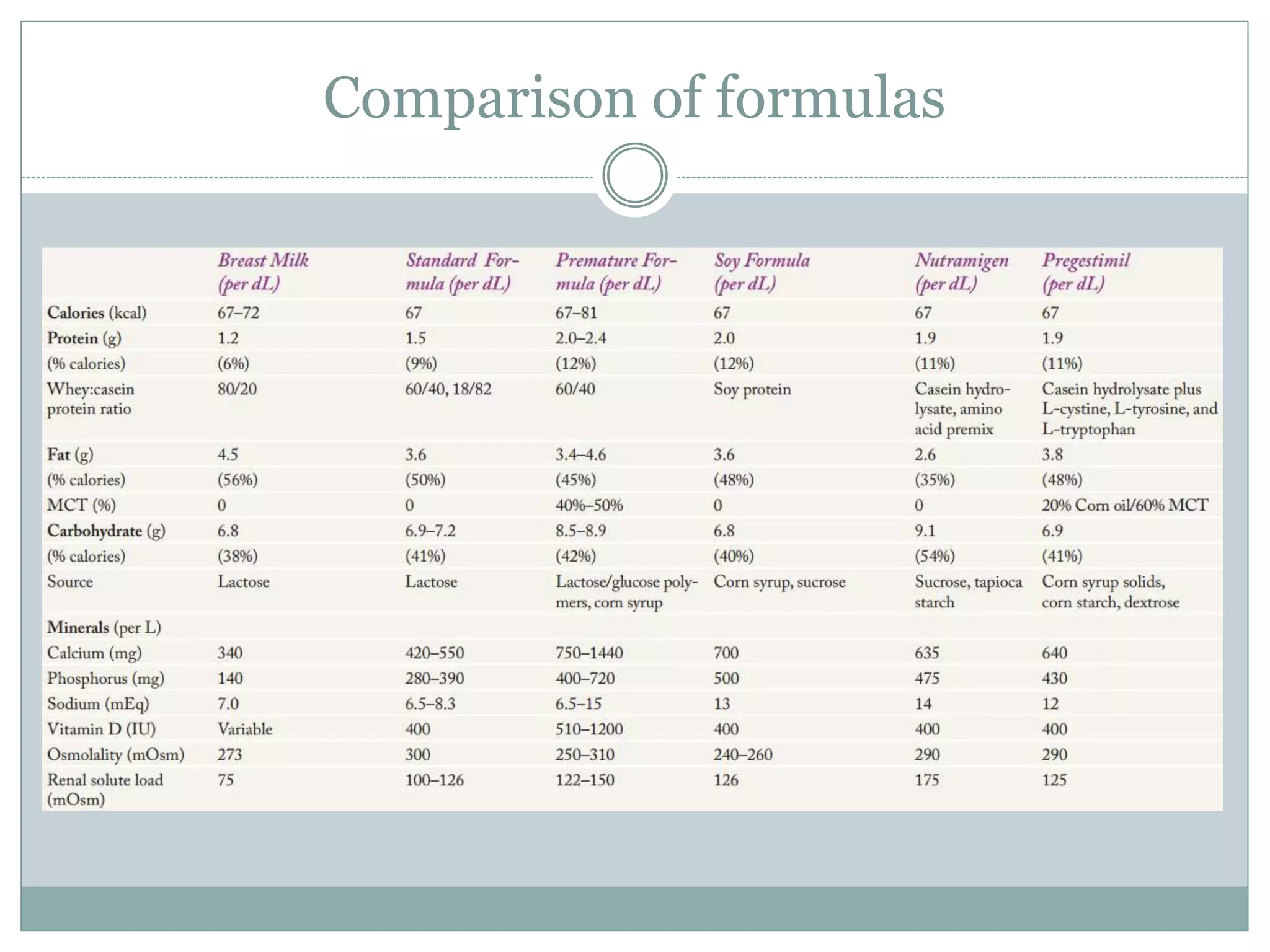
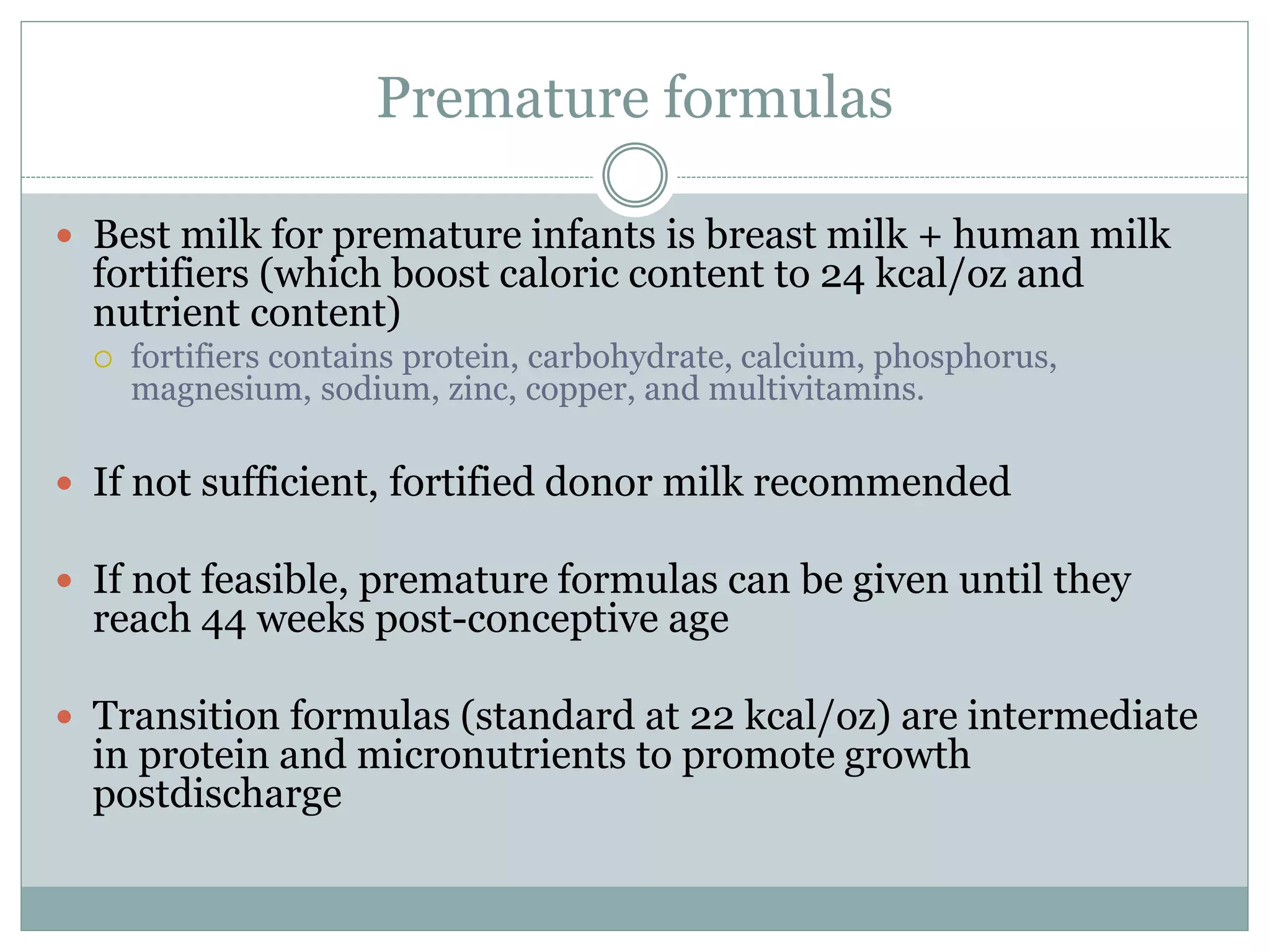
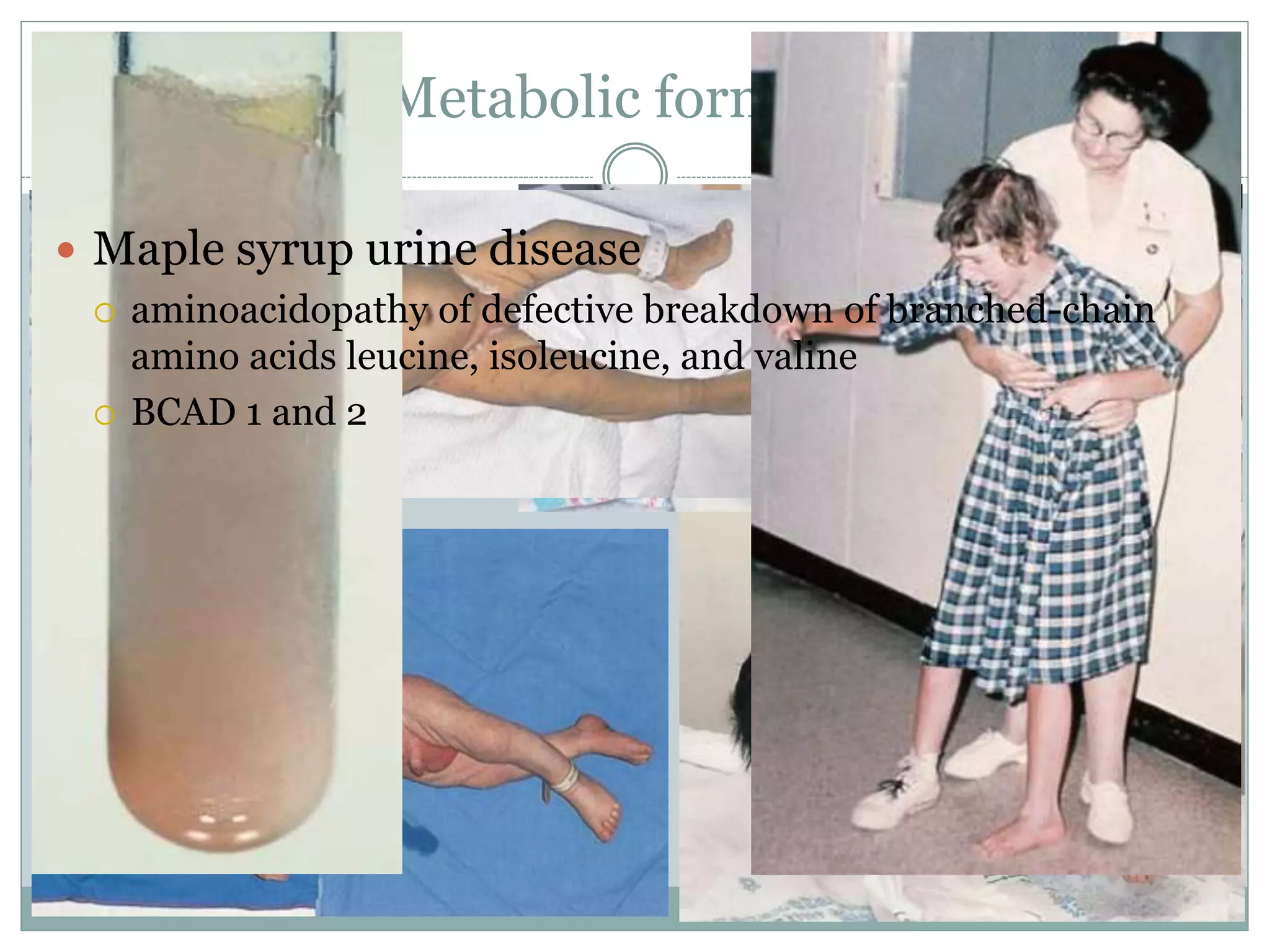
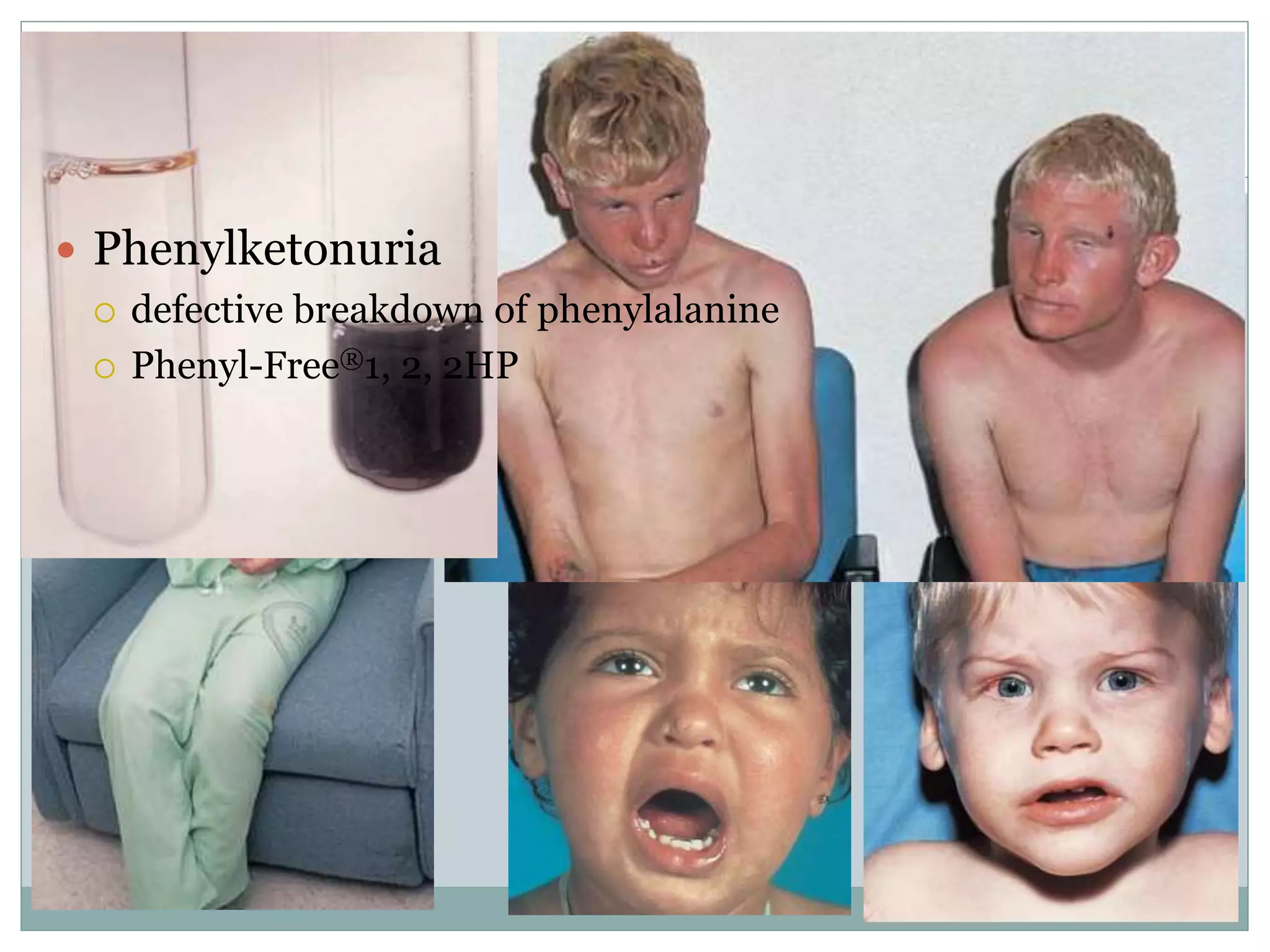
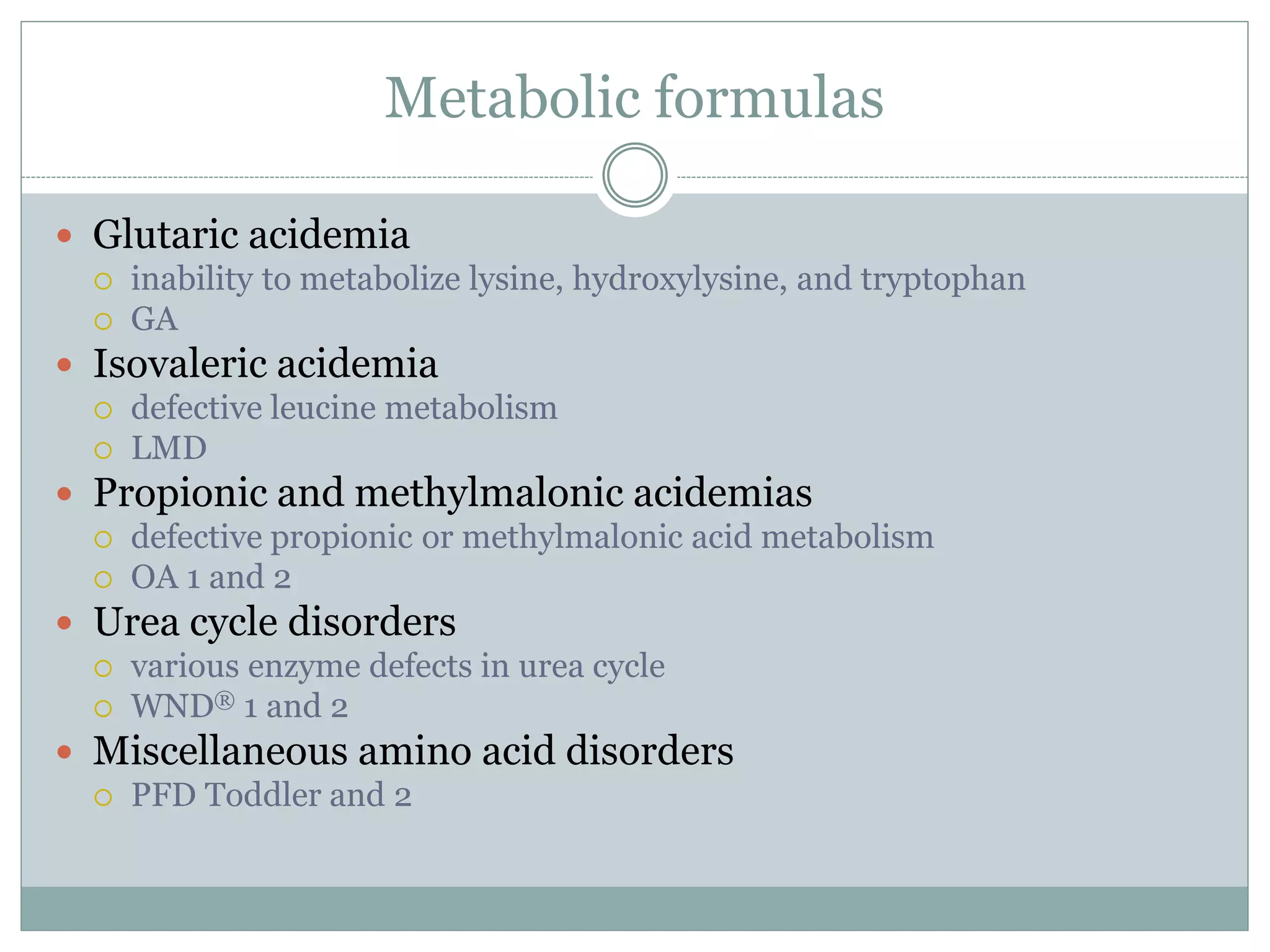
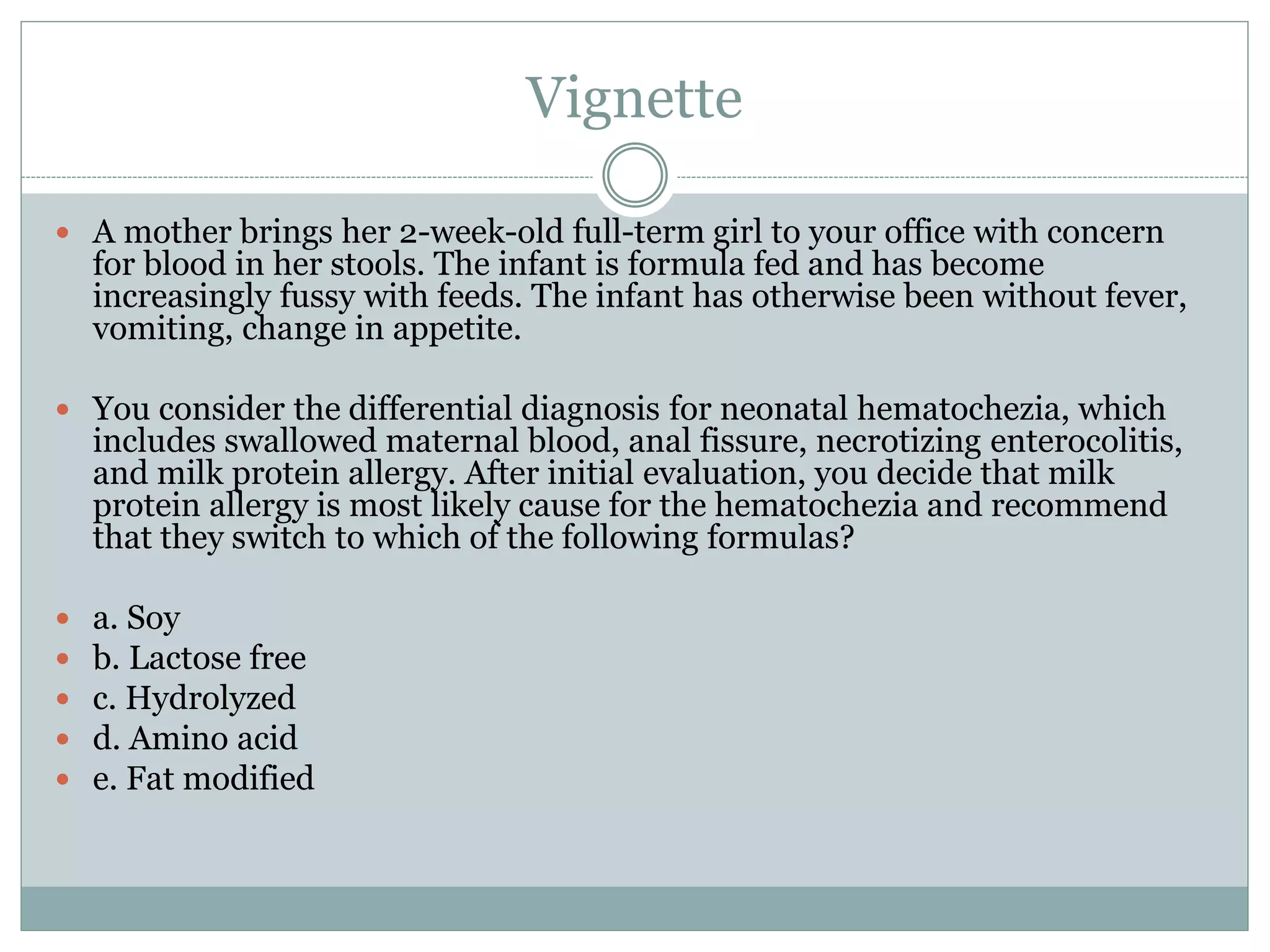
The document discusses the various types of milk formulas available for infants, their nutritional content, and the benefits of breastfeeding versus formula feeding. It outlines the indications for the use of different types of formula, including cow's milk protein-based, soy, protein hydrolysate, and amino acid formulas, along with their respective indications and nutritional considerations. Additionally, it highlights breastfeeding advantages, challenges, and the implications of feeding choices on infant health and development.