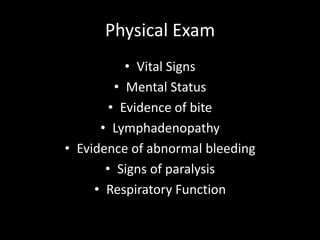
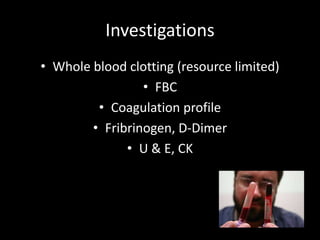
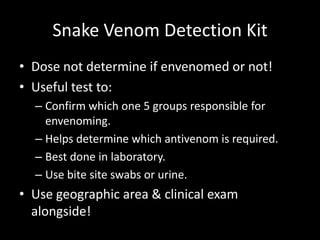
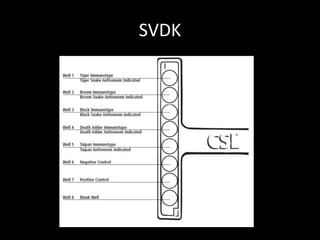
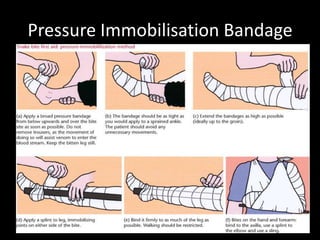
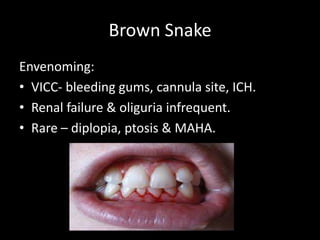
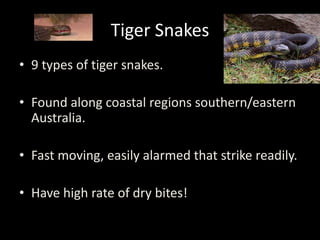
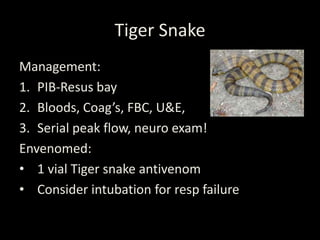
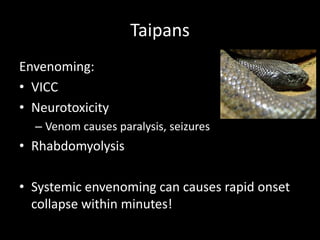
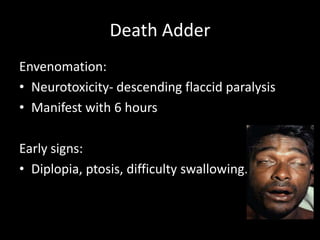
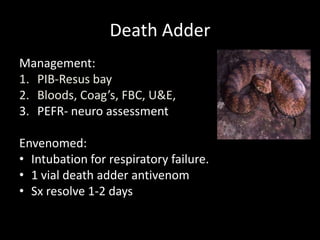
This document provides guidance for emergency department nurses on snake bite management in Australia. It discusses the most common poisonous snakes found in Australia and their characteristic clinical envenoming syndromes. It emphasizes the importance of a thorough risk assessment, physical exam, and investigations to determine if envenoming has occurred. The document also reviews pressure immobilization bandaging techniques, indications for antivenom administration, and supportive care for the different clinical envenoming syndromes caused by Australia's major snake groups: brown snakes, tiger snakes, mulga/black snakes, taipans, and death adders.