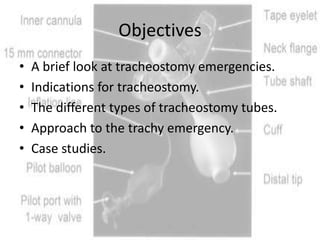
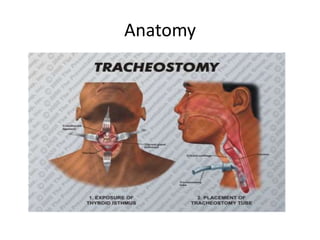
The document discusses tracheostomy emergencies, including indications for tracheostomies, different types of tracheostomy tubes, and approaches to emergencies such as tube obstruction or displacement. Case studies are presented on blocked and dislodged tracheostomy tubes. Key steps in managing emergencies include providing oxygen, suctioning, changing to a cuffed tube if needed, and ensuring correct tube placement. Understanding tracheostomy emergencies is important for emergency nurses as more patients are discharged home with long-term tracheostomies.