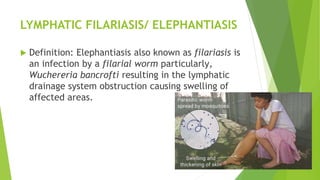
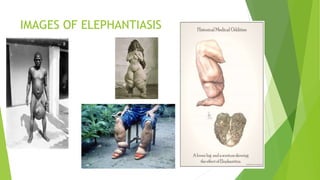
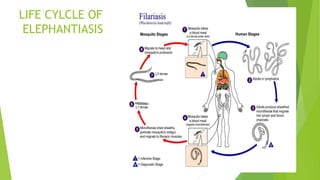
This presentation discusses elephantiasis, also known as lymphatic filariasis. It is caused by filarial worms being transmitted via mosquito bites, infecting the lymphatic system and causing blockages. This leads to swelling of the limbs and genitals. It occurs commonly in areas with poor sanitation. The life cycle involves microfilariae infecting mosquitoes which then transmit the parasite during blood meals. Diagnosis involves identifying the parasite via blood samples, tissues, or clinical symptoms like swelling. Treatment involves preventative drugs and antibiotics, while management focuses on wound care, exercises, and addressing psychological impacts of disfigurement. Complications can include disability, necrosis, and secondary infections if not properly cared for.