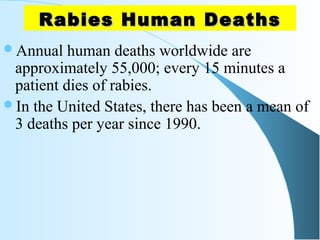
Rabies is a fatal viral disease transmitted through the bites of rabid animals, most commonly dogs. It causes inflammation of the brain and is nearly 100% fatal once symptoms develop. Over 95% of human deaths from rabies occur in Asia and Africa, with an estimated 55,000 deaths worldwide each year. Rabies can be prevented through vaccination of animals and humans. For humans, pre-exposure vaccination or prompt post-exposure prophylaxis, including wound cleansing, vaccination, and possibly rabies immunoglobulin administration, can prevent the disease if administered promptly after exposure.