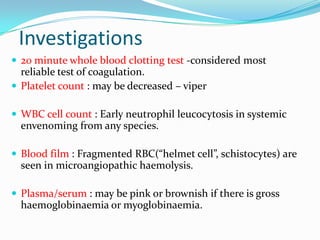
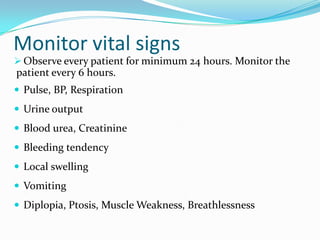
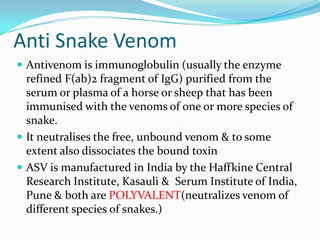
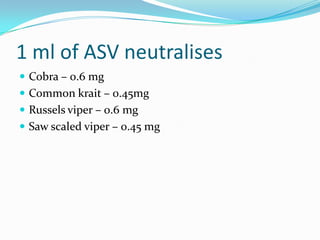
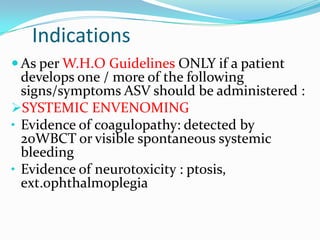
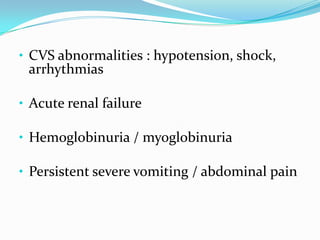
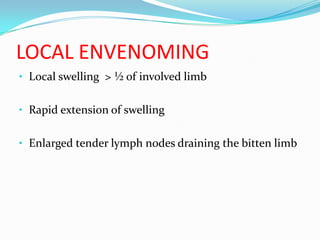
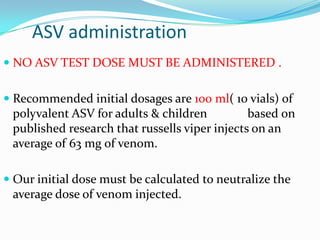
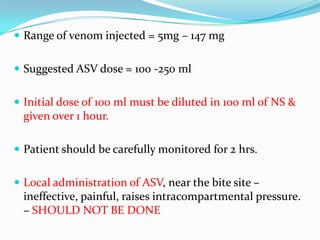
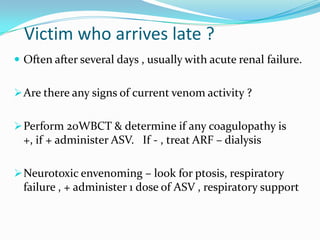
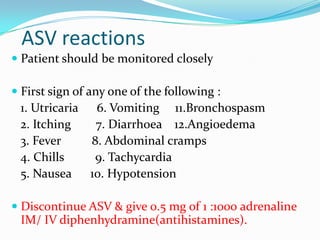
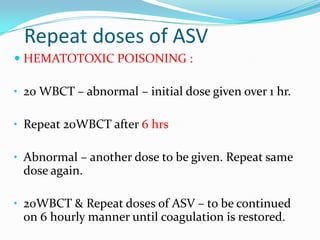
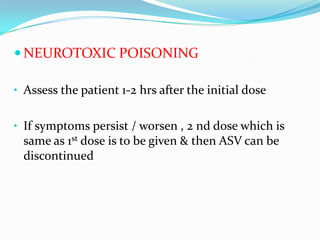
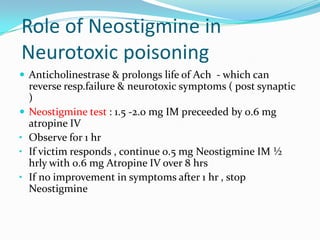
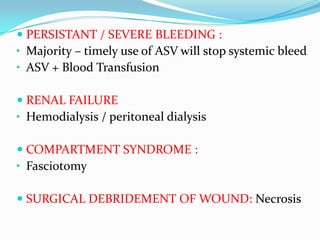
The document outlines guidelines for the treatment of snake bites, including rapidly assessing the airway, breathing, and circulation of the patient; administering tetanus toxoid, antibiotics, and anti-venom as needed based on symptoms; and closely monitoring vital signs and administering supportive care for any complications like respiratory failure, hypotension, or renal failure. Laboratory tests are also recommended to identify coagulopathies or tissue damage from the venom.