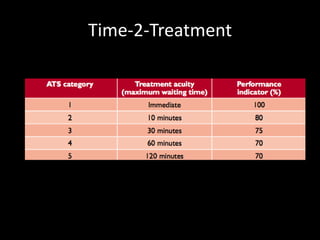
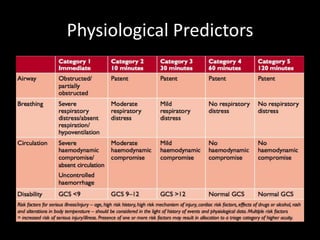
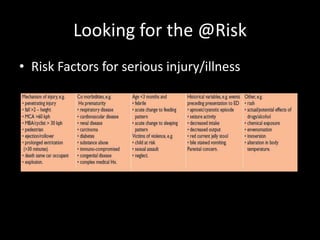
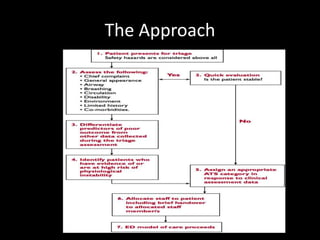
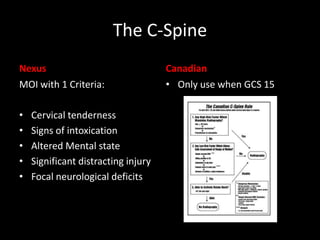
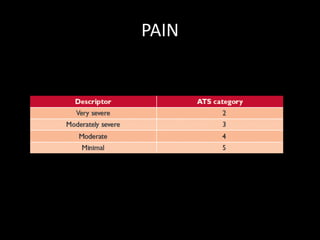
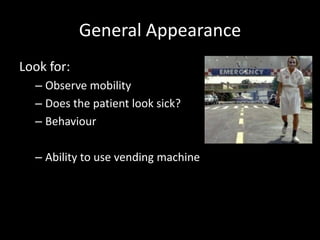
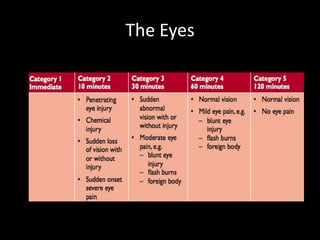
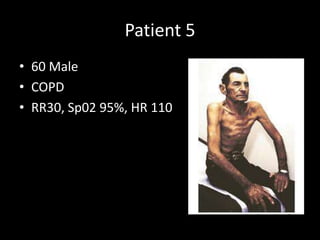
The document outlines the fundamentals of triage, including its definition, the Australian and Australasian Triage Scales, and the assessment of patients based on physiological predictors and risk factors for poor outcomes. It emphasizes the importance of timely response to clinical findings and provides guidelines for evaluating airway, breathing, circulation, and disability during triage. Additionally, it highlights critical observations and alerts for high-risk patients, as well as strategies for managing crowded waiting rooms.