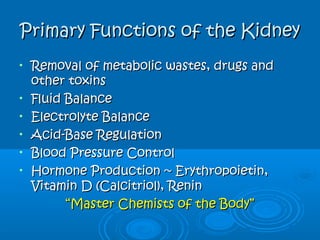
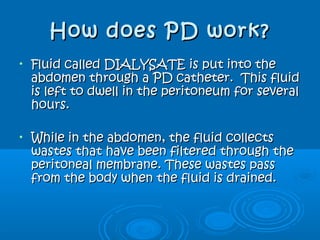
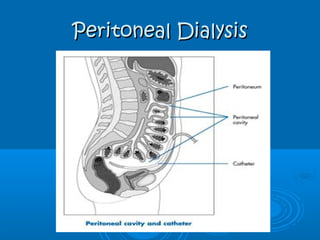
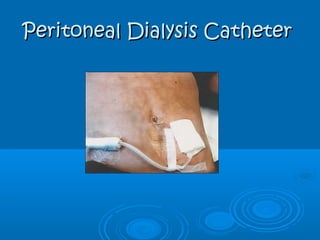
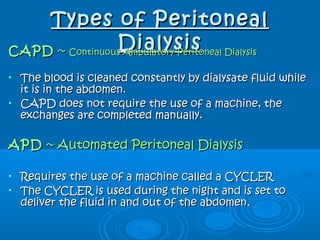
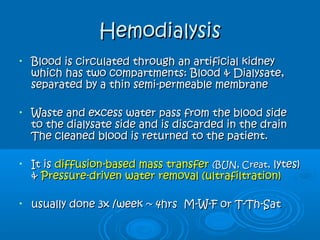
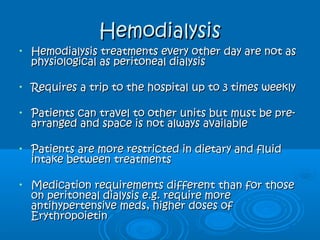
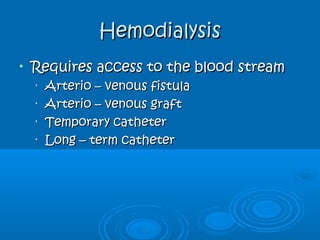
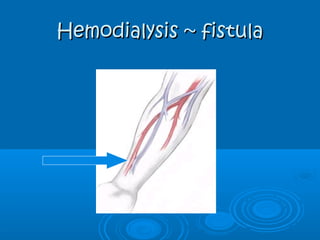
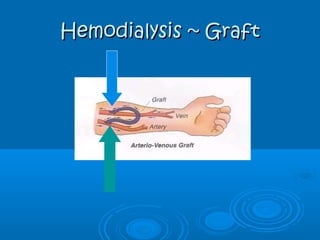
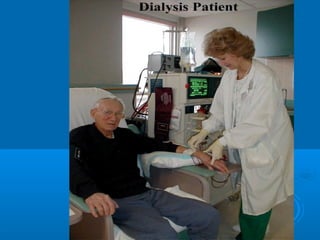
This document discusses renal replacement therapy (RRT) including the stages of kidney disease, types of dialysis, and access methods. It covers the primary functions of the kidney and consequences of kidney failure. The two main types of RRT are peritoneal dialysis and hemodialysis. Peritoneal dialysis uses the peritoneal membrane as a filter through a catheter, while hemodialysis uses an artificial kidney external to the body with vascular access.