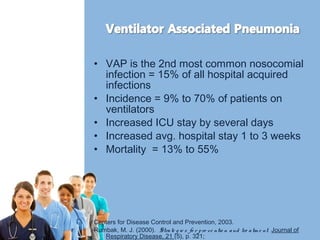
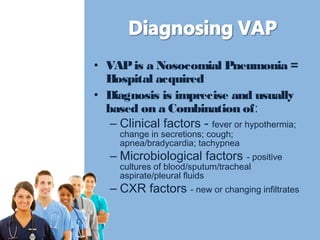
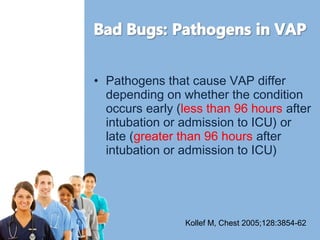
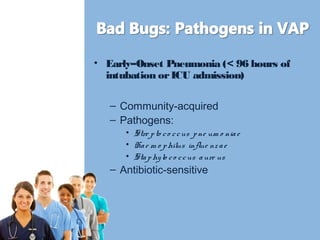
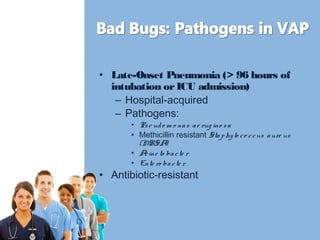
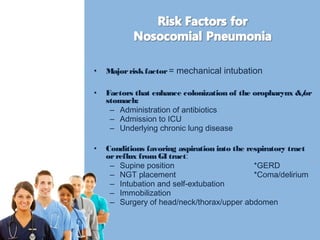
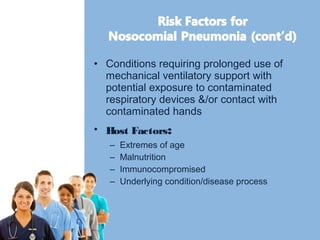
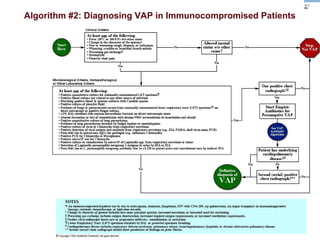
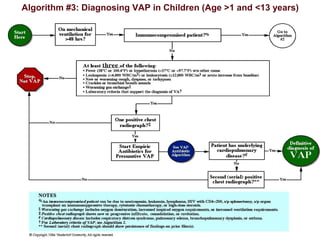
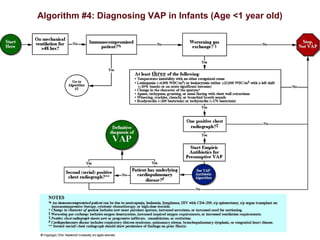
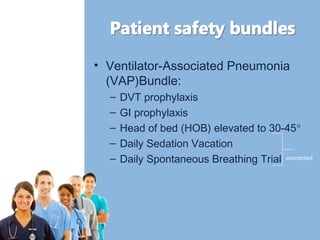
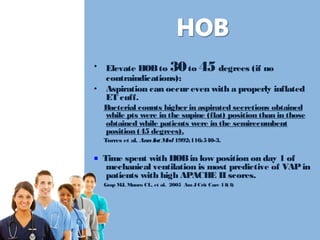
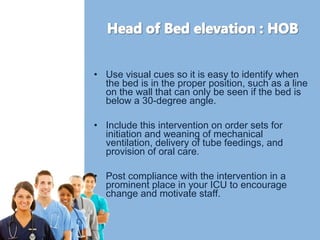
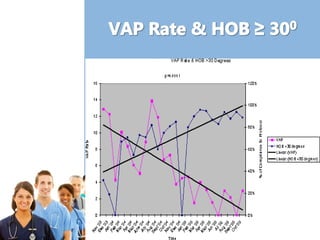
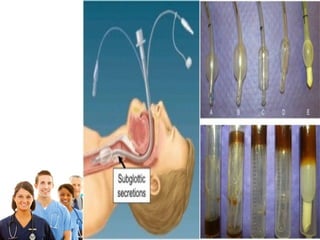
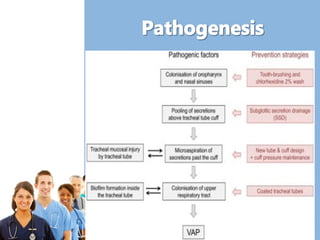
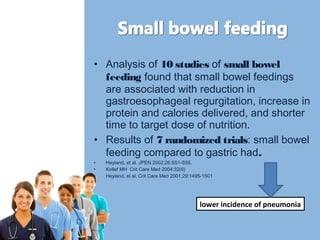
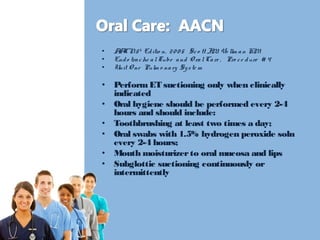
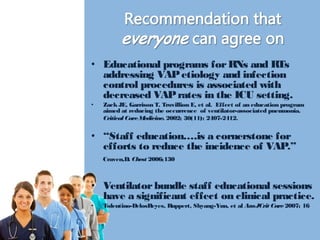
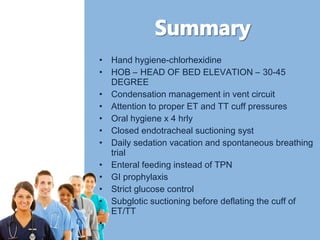
Ventilator-associated pneumonia (VAP) is a common nosocomial infection that increases ICU stay and mortality. The document discusses risk factors for VAP and strategies to prevent and diagnose it, including implementing a VAP bundle with elements like elevating the head of bed, daily sedation vacations, and oral care. It emphasizes the importance of staff education to properly implement prevention protocols and decrease VAP rates.