This document discusses advances in ECMO and REBOA treatment.
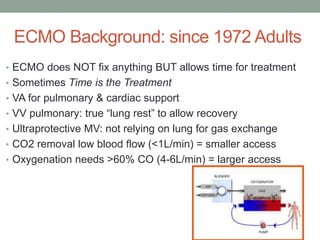
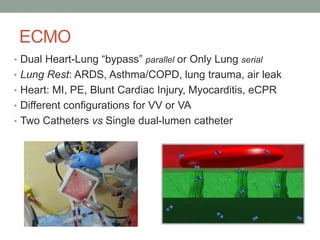
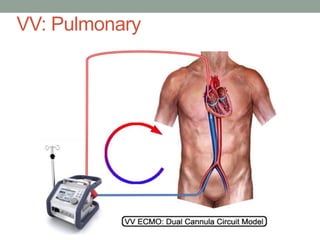
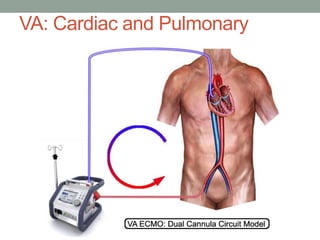
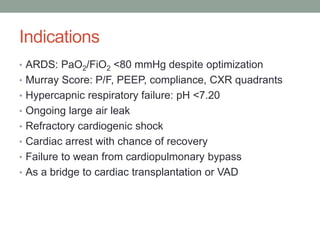
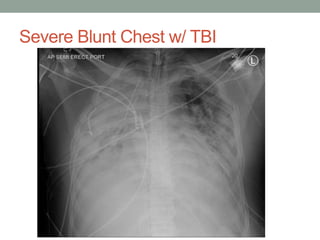
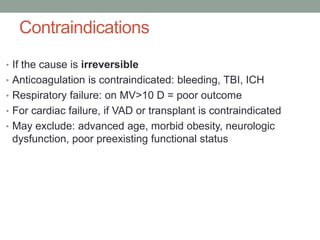
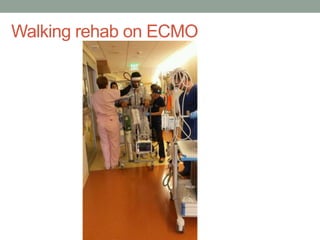
ECMO provides lung and heart support to allow time for treatment when time is the treatment. It is used for conditions like ARDS, lung trauma, heart attacks, and as a bridge to transplant. Outcomes have improved at ECMO centers.
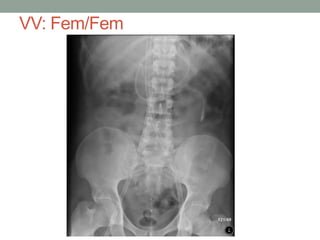
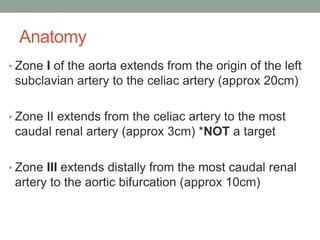
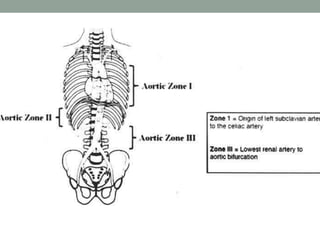
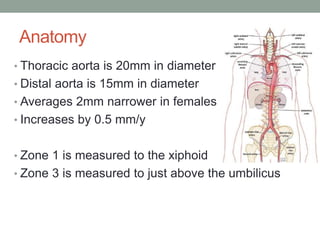
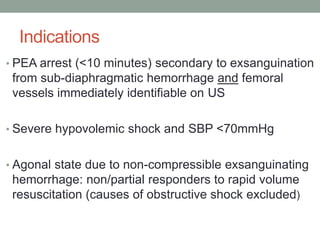
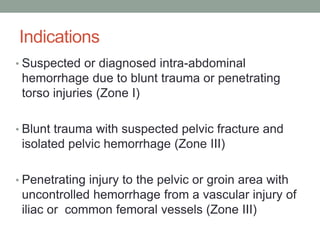
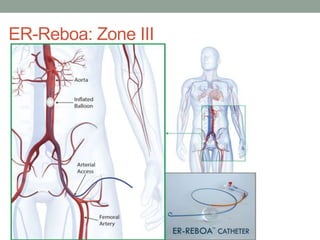
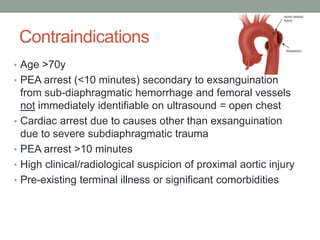
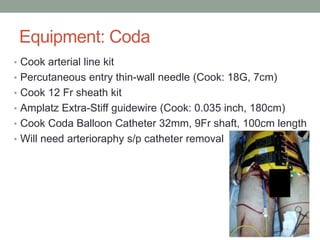
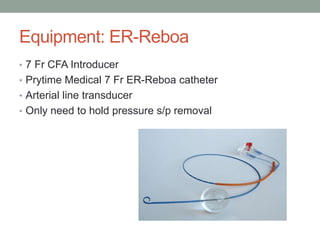
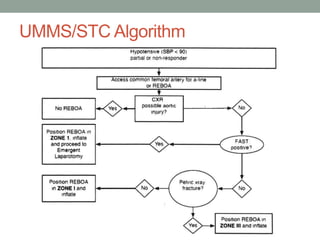
REBOA is the placement of a balloon in the aorta to control hemorrhage from the abdomen or pelvis. It is indicated for trauma with suspected bleeding below the diaphragm and can control bleeding until surgery.