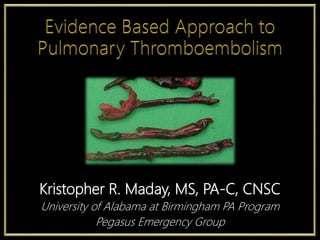
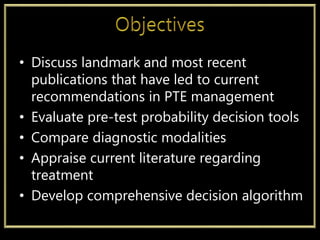
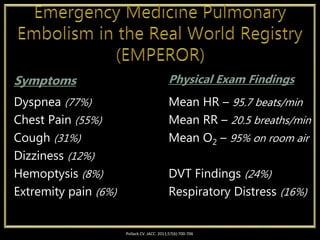
This document provides an overview of pulmonary embolism (PE) including epidemiology, risk factors, clinical presentation, diagnostic evaluation, and treatment recommendations. Some key points:
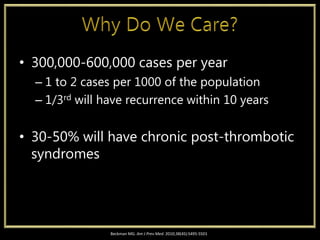
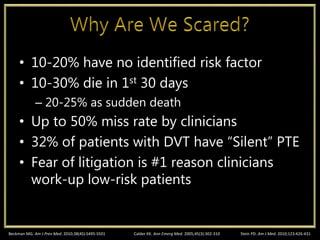
- PE affects 300,000-600,000 Americans annually, with 30-50% developing long-term complications. Up to 50% of cases are initially missed by clinicians.
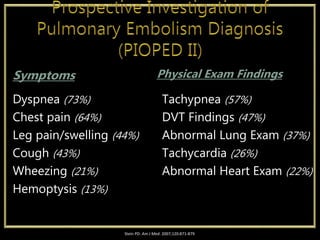
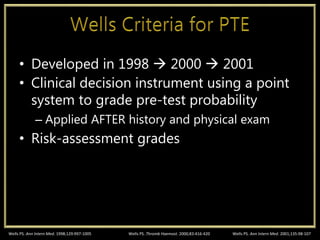
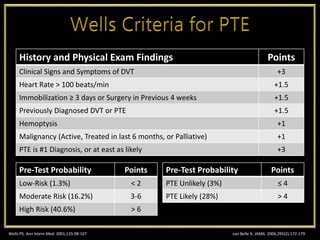
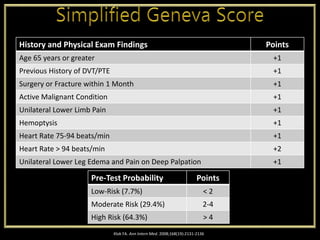
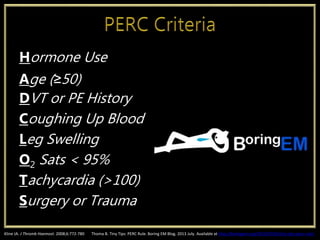
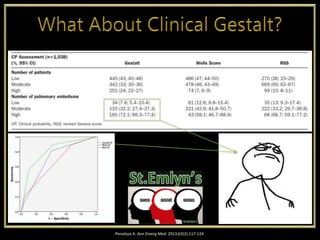
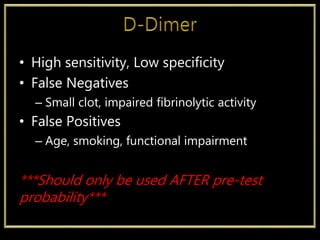
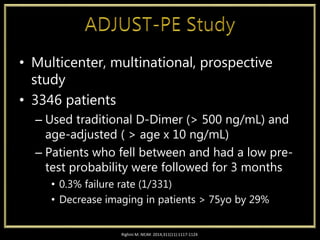
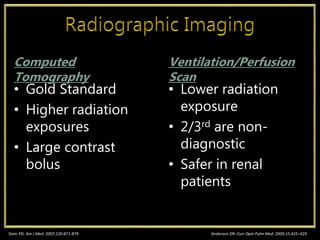
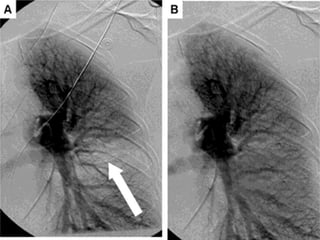
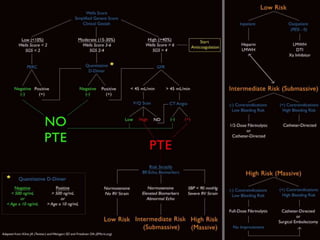
- Clinical prediction tools like the Wells Criteria and PERC Rule can assess pre-test probability. D-dimer can help exclude PE in low risk patients. CT pulmonary angiography and ventilation-perfusion scans are used for diagnosis.
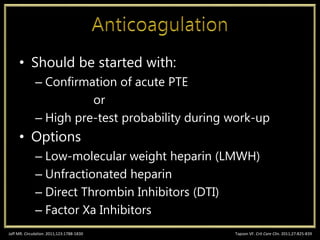
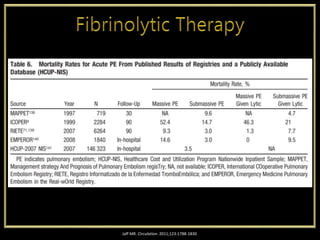
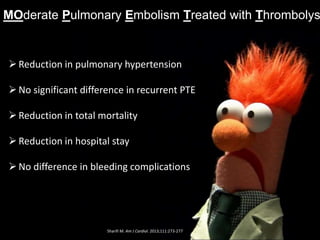
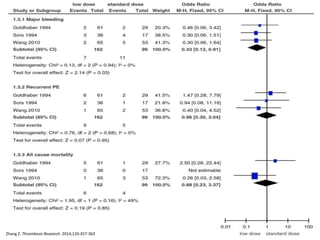
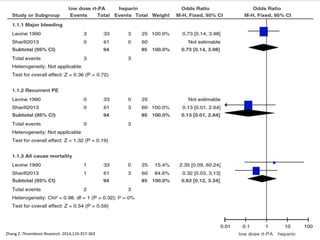
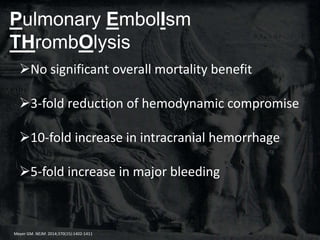
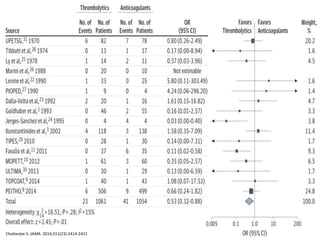
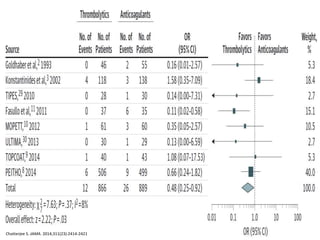
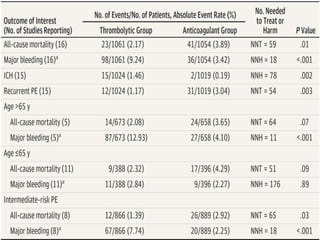
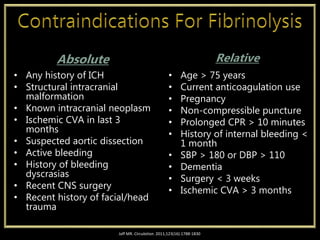
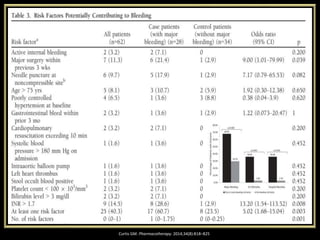
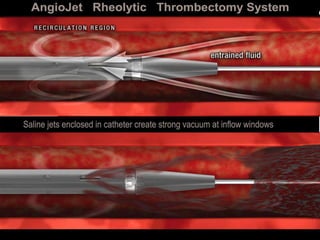
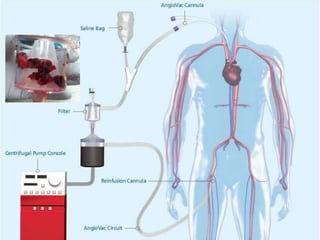
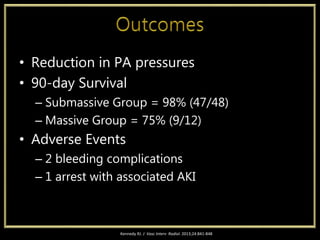
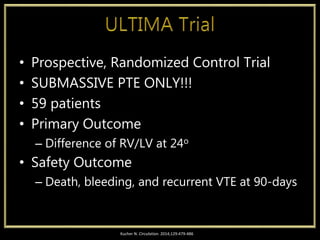
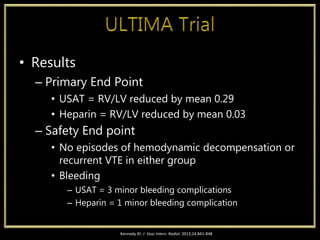
- Anticoagulation is standard treatment for PE. For intermediate/high-risk PE, thrombolysis,