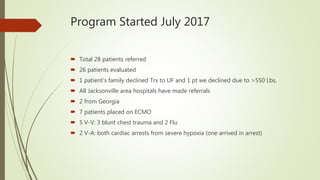
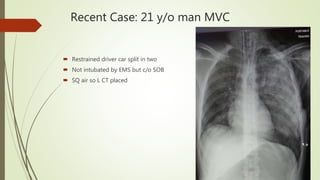
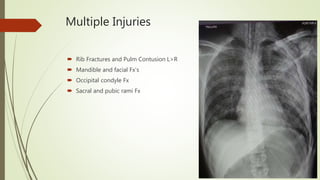
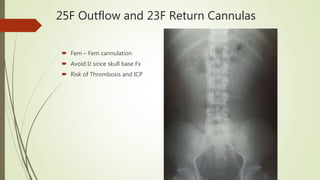
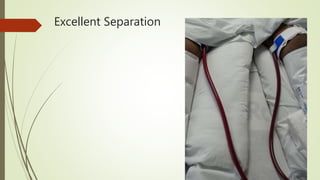
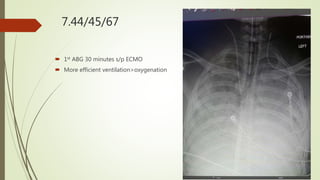
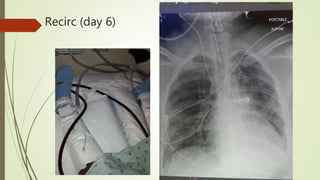
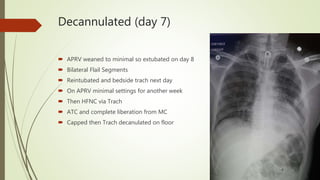
The ECMO program at UF Health has treated 28 patients referred since starting in July 2017, with 7 patients placed on ECMO support. The program has accomplished several milestones like treating two patients simultaneously and cannulating patients back-to-back. Survival rates for patients treated with ECMO are over 80%. The program aims to progress through three phases, currently rescuing patients at UF Health and from the Jacksonville area who need advanced support. A recent case described a 21-year-old trauma patient who required multiple surgeries and ultimately ECMO support, showing improvement over his ICU course before being successfully decannulated.