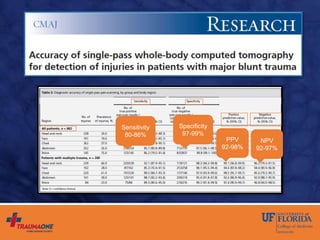
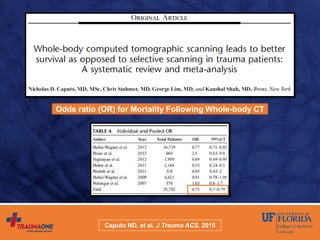
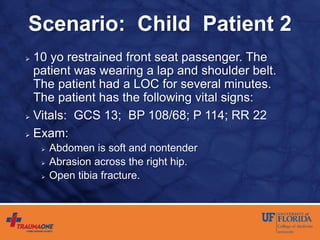
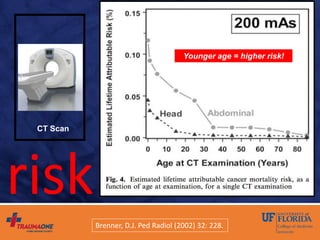
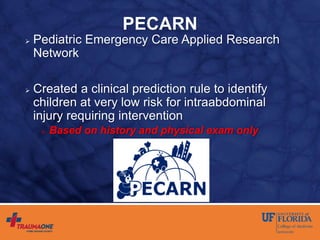
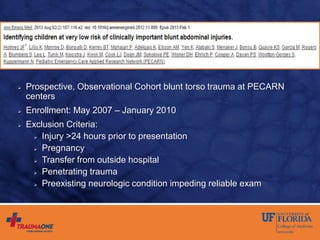
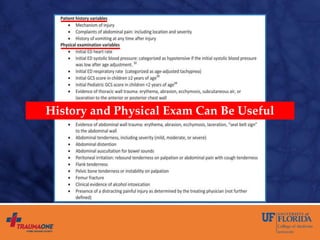
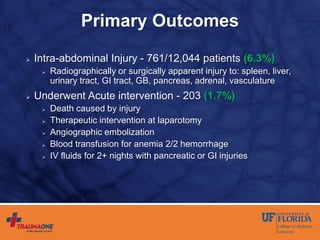
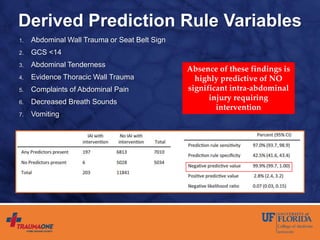
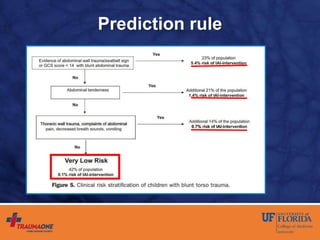
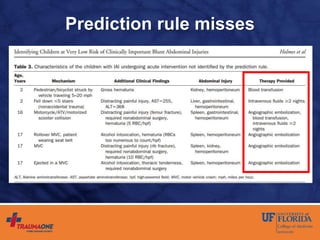
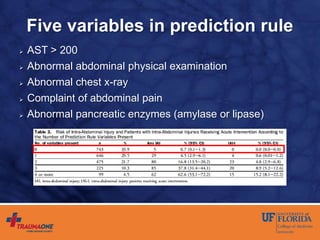
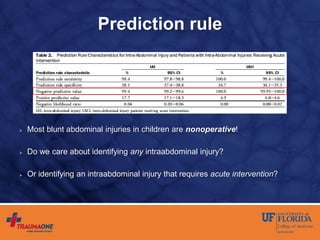
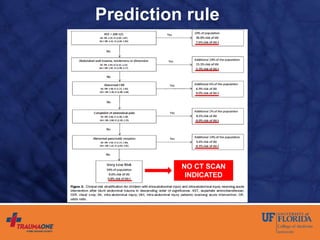
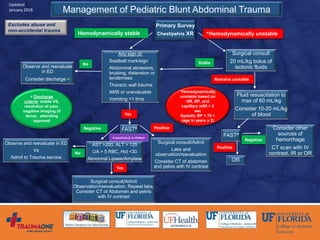
The document discusses prediction rules for identifying pediatric patients at low risk for intra-abdominal injuries after blunt abdominal trauma. It summarizes the PECARN prediction rule, which identifies variables from history and physical exam that predict whether a child needs intervention. The rule achieved high sensitivity and specificity. The document also discusses the UF-Jax algorithm for managing pediatric blunt abdominal trauma, which incorporates physical exam findings, labs, ultrasound, and CT imaging to determine need for observation, admission, or intervention. The goal is identifying injuries requiring treatment while avoiding unnecessary radiation exposure.