1) Carcinoma of the penis has a higher incidence in South America, East Africa, and South East Asia. Risk factors include HPV infection, phimosis, smoking, and lack of circumcision.
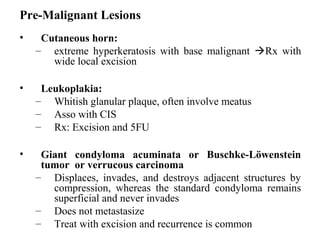
2) Early stage lesions include erythroplasia of Queyrat, Bowen's disease, balanitis xerotica obliterans, and giant condyloma acuminatum. Advanced lesions are staged using the TNM system.
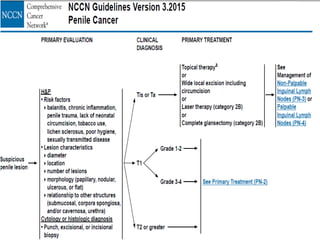
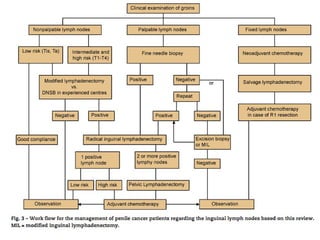
3) Treatment depends on the stage but may include local excision, circumcision, partial or total penectomy. Sentinel lymph node biopsy helps determine if inguinal lymphadenectomy is needed.





![• Erythroplasia of Queyrat: [non keratinising CIS]
– Red velvety circumscribed painless lesion , may ulcerate and
painful
– Histology:
• Atypical hyperplastic mucosal cell with malignant features
• Hyperchromatic nuclei & multi-level mitotic figures
• Submucosa : proliferation of capillaries & inflammatory
infiltrate of plasma cell
– 10x more likely to progress then Bowen’s disease
– Treatment
– Penile preserving:
• Topical 5-FU or imiquimod
• Laser (CO2) , photodynamic therapy , cryotherapy , Mohs MS
• Bowen’s disease: [Keratinising CIS ]
– CIS in the genital and perineal skin
– Rx : WLE , laser, cryoablation](https://image.slidesharecdn.com/seminarcapenis-160325100953/85/Seminar-ca-penis-8-320.jpg)