Here are the key organ-preserving treatment options for penile cancer:
- Circumcision for very small, prepuce-confined tumors
- Local wedge excision or partial penectomy for small T1 tumors
- Glansectomy for selected T1 tumors not involving corpora cavernosa
All local options have significant recurrence risks of 40-50%. Close follow-up is required.



![Risk factors
• What are the risk factors?
1. Smoking
2. UV radiation
3. Foreskin: phimosis , poor hygiene
• neonatal circumcision eliminate risk by 5x [Daling 2005]
• But not circumcision in adult (Maden 1993)
4. HPV infection (16, 18): asso in 50%
• Sexual transmission causing genital warts, condyloma acuminate
• HPV infects the basal epithelial cell that proliferates
• Daling (2005) HPV DNA was detected in 80 % of tumor specimens
• Carcinogenesis : interfering with p53 & pRB
• Role in prognosis is unclear
• Verrucous carcinoma is not related to HPV infection
5. Penile trauma
• Prognostic makers:
– p53, SCC antigen, P16, Ki-67m E-cadherin and MMP-2
4](https://image.slidesharecdn.com/capenisedmond-130318091738-phpapp01/85/Ca-penis-edmond-4-320.jpg)




![Risk factor for metastasis
1. Growth pattern (Cubilla 1993)
– Superficiallly spreading, LN met in 42%
– Vertical growth, LN met in 82%
1. Basaloid and sarcomatous histologic
pattern [MSKCC review (Cubilla 2001)]
2. Stage
3. Grade
4. Status of vascular invasion (Slaton 2001)
9](https://image.slidesharecdn.com/capenisedmond-130318091738-phpapp01/85/Ca-penis-edmond-9-320.jpg)
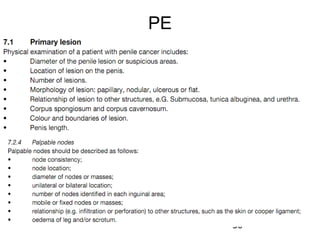
![How do they present ?
Presentation:
• a sore that has failed to heal
• a subtle induration in the skin, to a large exophytic growth.
• a phimosis may obscures the tumor and allows it to grow undetected.
• Rarely, a mass, ulceration, suppuration, or hemorrhage may manifest in the
inguinal area because of nodal metastases.
• Pain is infrequent.
• Buck fascia, which surrounds the corpora, acts as a temporary barrier.
• Eventually, the cancer penetrates the Buck fascia and the tunica albuginea,
where the cancer has access to the vasculature and systemic spread is
possible
• Delay presentation (50%) due to
– Embarrassment, guilt, fear, ignorance, and neglect
– Self treatment with various skin creams and lotions.
– Doctor: confuse with other benign penile lesions
• Metastasis :
– Dehydration : hypecalcemia in 20% on presentation (PTH like) [MSKCC]
– SOB
10](https://image.slidesharecdn.com/capenisedmond-130318091738-phpapp01/85/Ca-penis-edmond-10-320.jpg)






![Premalignant lesion: CIS
• Erythroplasia of Queyrat: [non keratinising CIS]
– CIS: as oppose to Bowen’s disease, occur in glans or inner part of prepuce
– Red velvety circumscribed painless lesion , may ulcerate and painful
– Histology:
• Atypical hyperplastic mucosal cell with malignant features
• Hyperchromatic nuclei & multi-level mitotic figures
• Submucosa : proliferation of capillaries & inflammatory infiltrate of plasma cell
– 10x more likely to progress then Bowen’s disease
– Treatment
– Penile preserving:
• Topical 5-FU or imiquimod
– 5-FU: block DNA synthesis (structure similar to thymine) SE: erythema , weeping
– 5% Imiquimod (imidazoguinonin tetracyclicamine): induce IF-alfa
• Laser (CO2) , photodynamic therapy , cryotherapy , Mohs MS
• If affect large area or recurrence: Total glans resurfacing + skin graft + deep biopsy
– High risk of local recurrence in penile preserving txn
• Bowen’s disease: [Keratinising CIS ]
– CIS in the genital and perineal skin
– Txn : WLE , laser, cryoablation
18](https://image.slidesharecdn.com/capenisedmond-130318091738-phpapp01/85/Ca-penis-edmond-18-320.jpg)

















![What is organ preserving therapy?
• Laser surgery
– For local and limited invasive disease
– Four types of lasers have been used
1. Carbon dioxide
2. Neodymium:yttrium-aluminum-garnet (ND:YAG)
3. Argon
4. Potassium-titanyl-phosphate (KTP) lasers
– The carbon dioxide laser
• vaporizes tissue
• penetrates only to a depth of 1mm
• coagulate blood vessels less than 0.5 mm
– The ND:YAG laser
• penetrate 5 mm depending on the power
• Can coagulate vessels up to 5 mm
– The argon and KTP lasers have less tissue penetration than the
carbon dioxide laser and are rarely used
– Result : 7% recurrence in 4yr FU [Frimberger 2002]
41](https://image.slidesharecdn.com/capenisedmond-130318091738-phpapp01/85/Ca-penis-edmond-41-320.jpg)













![Incidence
• Depends on:
– Tumor grade: 30% G1 vs 40% G3
– Local stage : 60% in pT2 & 75% in pT3-4
– T1G2: 50% [Naumann BJU 2008]
– Type of local tumor: Basoloid vs Classic
56](https://image.slidesharecdn.com/capenisedmond-130318091738-phpapp01/85/Ca-penis-edmond-56-320.jpg)









![Non-palpable LN : by pT stage
• Low risk gp: pTis, pTaG1/2, pT1 G1 (LN met < 17%)
– Active surveillance
– Optional: modified inguinal LND
• Intermediate risk gp: pT1G2 or higher (LN met 50%)
– DSNB , follow by complete LND if tumor +ve
– If DSNB not available base on risk factor + nomogram
• Superficial growth + no vascular invasion: Active surveillance
• vascular or lymphatic invasion OR infiltrating growth pattern: modified LND radical if tumor
+ve
• High risk gp: pT2-4 , any G3 (LN met 70%)
– Active surveillance is not appropriate:
• Higher risk of recurrence [Leijte]
– Immediate LN staging
• DSN then LND if +ve
• 3 yr DSS: 91% vs 80% (surveillance) [Lont]
– Modified radical inguinal LND (if FZ +ve in MILND)
– Immediate vs delay LND:
• 3yr survival: 84% vs 35%
• Which side? Both side
66](https://image.slidesharecdn.com/capenisedmond-130318091738-phpapp01/85/Ca-penis-edmond-66-320.jpg)

![What is the approach for palpable LN ?
• Explained:
– Palpable LN present at diagnosis in 58% patients
– Traditional : 50% +ve for metastasis, 50% inflammatory [Brazil]
– Today’s thinking: > 90% palpable LN are met
– If LN +ve on one side there is 50% chance to be +ve on the other side
• Any investigation suitable ?
– No value in dx of inguinal LN met
– Ultrasound + FNAC
• may reveal abnormal nodes & guide for fine-needle aspiration biopsy
• Palpable LN: SV 93% , SP 91%
• If negative repeat biopxy
– Dynamic SNB – No role is palpable LN
– Pelvic CT/MRI scan are widely done but with low SV/SP
– Nanoparticle-enhance MRI :SV 100%, SP 97% , PPV 80%
– 18FDG PET/CT: SV 80% , SP 100%
• But since LND is going to be perform irrespective of FNA result , FNA
may not be useful
• Thus early & bilateral radical LND is the standard procedure
68](https://image.slidesharecdn.com/capenisedmond-130318091738-phpapp01/85/Ca-penis-edmond-68-320.jpg)



![Fixed inguinal LN
• Neo-adjuvnat chemotherapy (response rate 20-60%)
– [Pizzocaro’s series]
– 3-4 courses of cisplatin & 5FU in 16 patients for fixed LN
– 60% could be radically resected following primary chemoTx
– 30% have probably cured
– Survival rate 25%
• Subsequent radical ilio-inguinal LNectomy strongly
recommended
• Should be used as part of a clinical trial
• Or Radiotherapy followed by lymphadenectomy but
higher morbidity
• Problem: high toxicity + high number of non responder
72](https://image.slidesharecdn.com/capenisedmond-130318091738-phpapp01/85/Ca-penis-edmond-72-320.jpg)


























