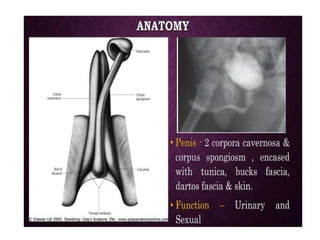
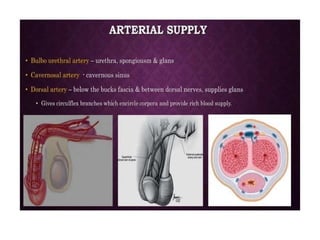
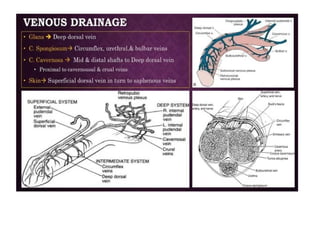
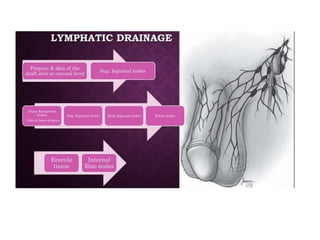
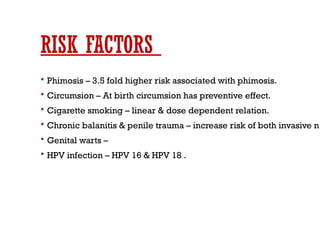
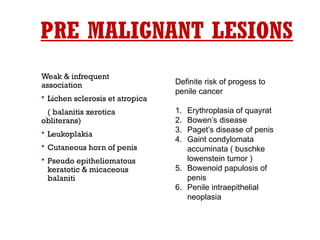
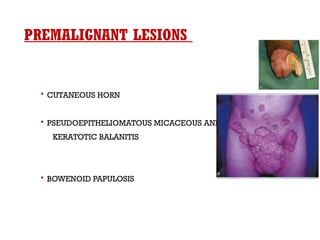
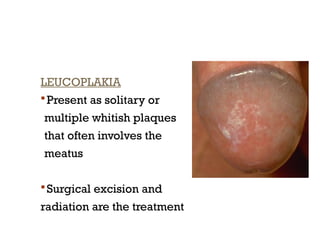
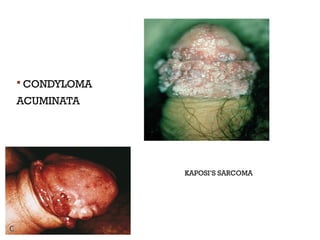
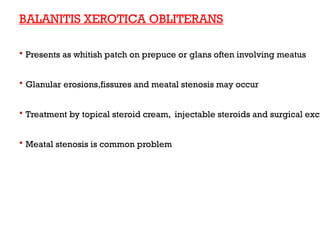
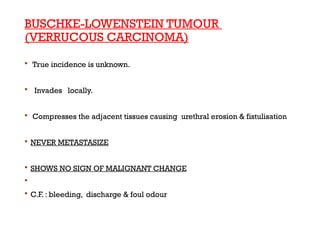
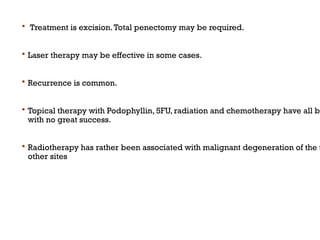
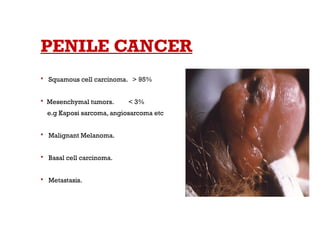
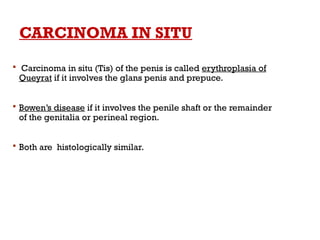
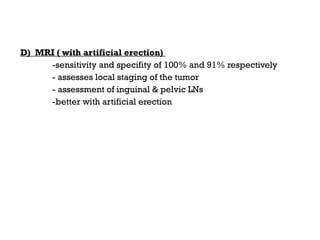
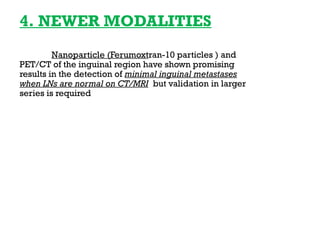
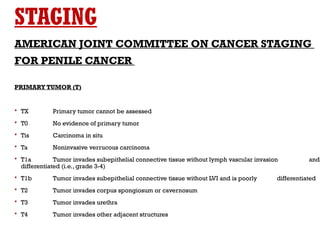
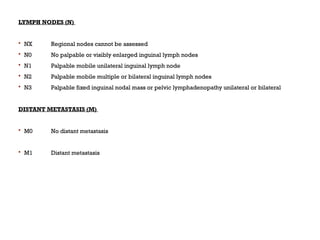
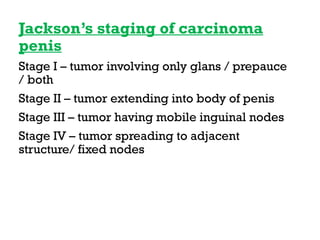
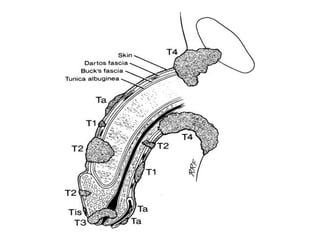
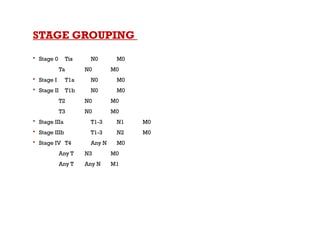
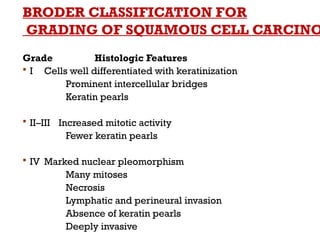
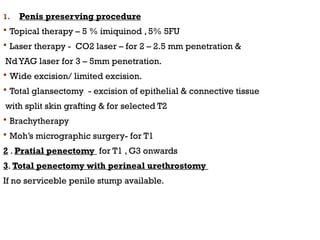
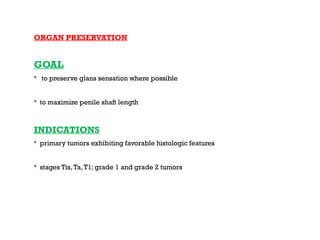
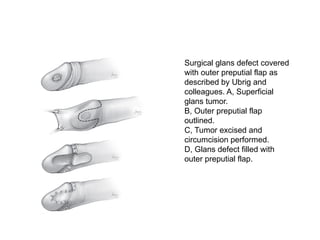
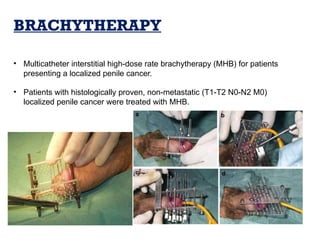
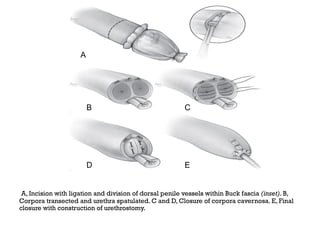
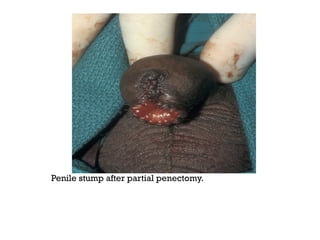
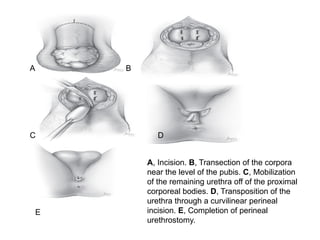
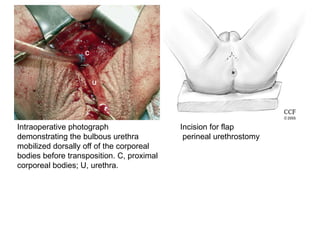
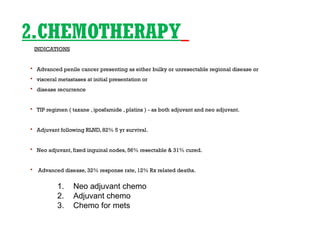
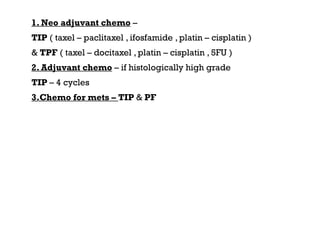
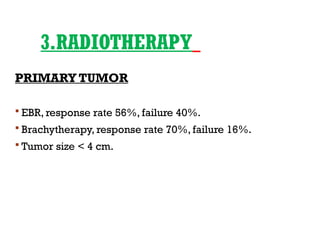
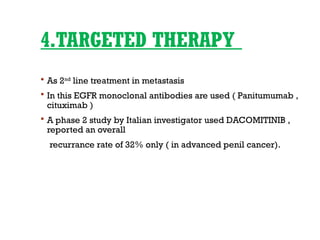
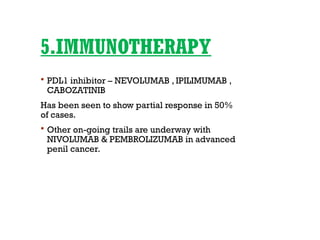
The document discusses the management of penile carcinoma, including its epidemiology, risk factors, clinical features, and various treatment options. It highlights the importance of a multidisciplinary approach and emphasizes surgical interventions such as penectomy, as well as chemotherapy and radiotherapy for advanced cases. Additionally, it describes the classification and staging of penile cancer, noting the significant recurrence rates and the challenges in treatment effectiveness.