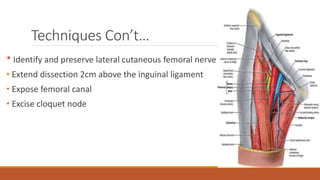
The document discusses different techniques for inguinal lymph node dissection (LND). It describes the anatomy of the superficial and deep inguinal lymph nodes and indications for LND. Two main techniques are described: the classic Daseler approach and a modified Catalona approach. The classic approach involves a longer incision and mobilizing the sartorius muscle. The modified approach uses a shorter incision and preserves the saphenous vein. Complications of LND include skin flap necrosis, lymphedema, wound infection, and thromboembolic events. Sentinel lymph node biopsy is now the standard approach for staging early stage melanoma and penile cancer.