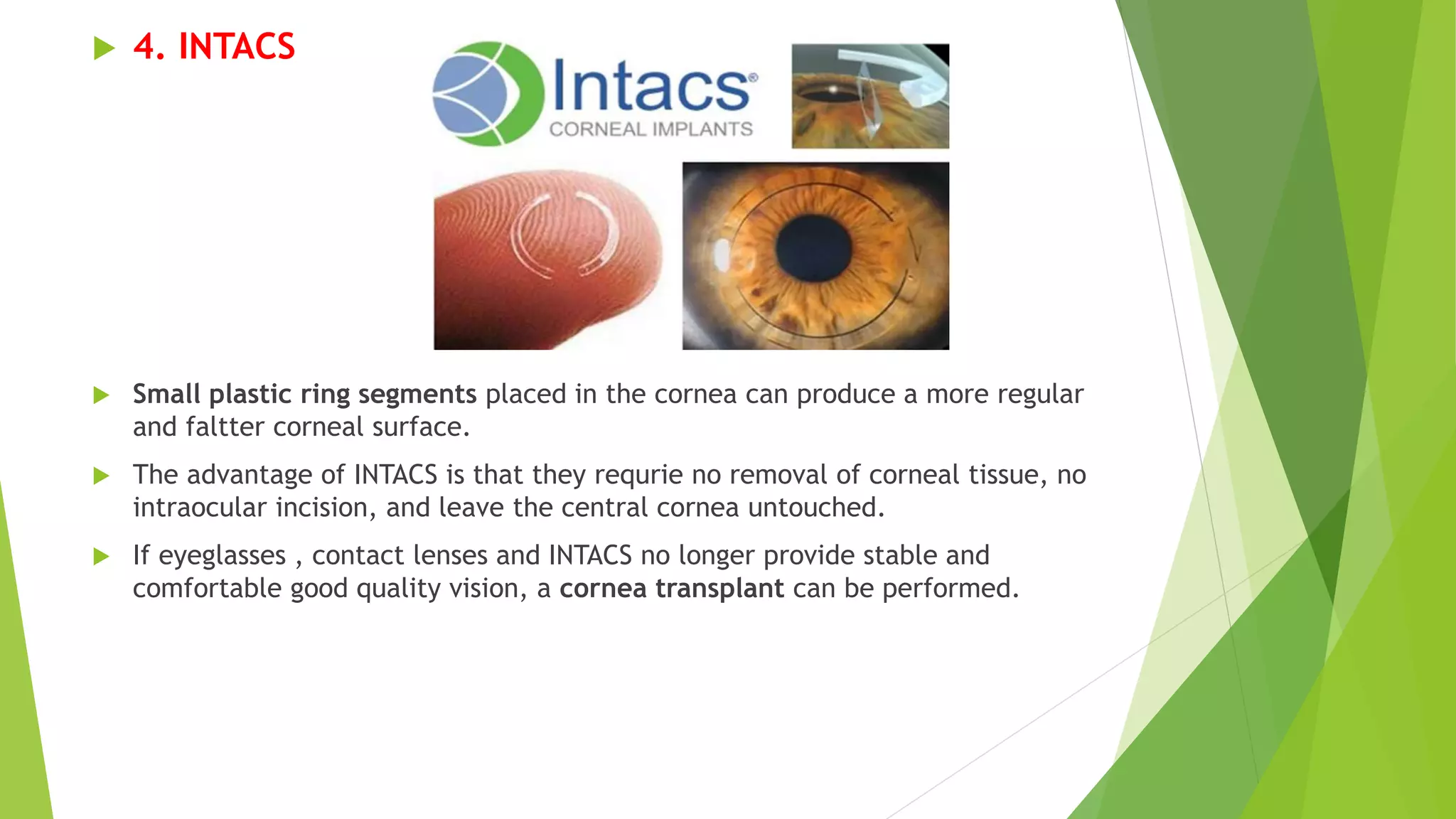
Keratoconus is a progressive eye disease where the cornea thins and bulges into a cone shape. It is diagnosed based on a patient's visual complaints and examination findings showing corneal thinning and irregularity. Treatment progresses from glasses and rigid contact lenses for mild cases. For more advanced cases, corneal collagen crosslinking may be used to stop progression, and INTACS ring segments or corneal transplantation may be needed to improve vision. The main types of transplantation are deep anterior lamellar keratoplasty and penetrating keratoplasty.