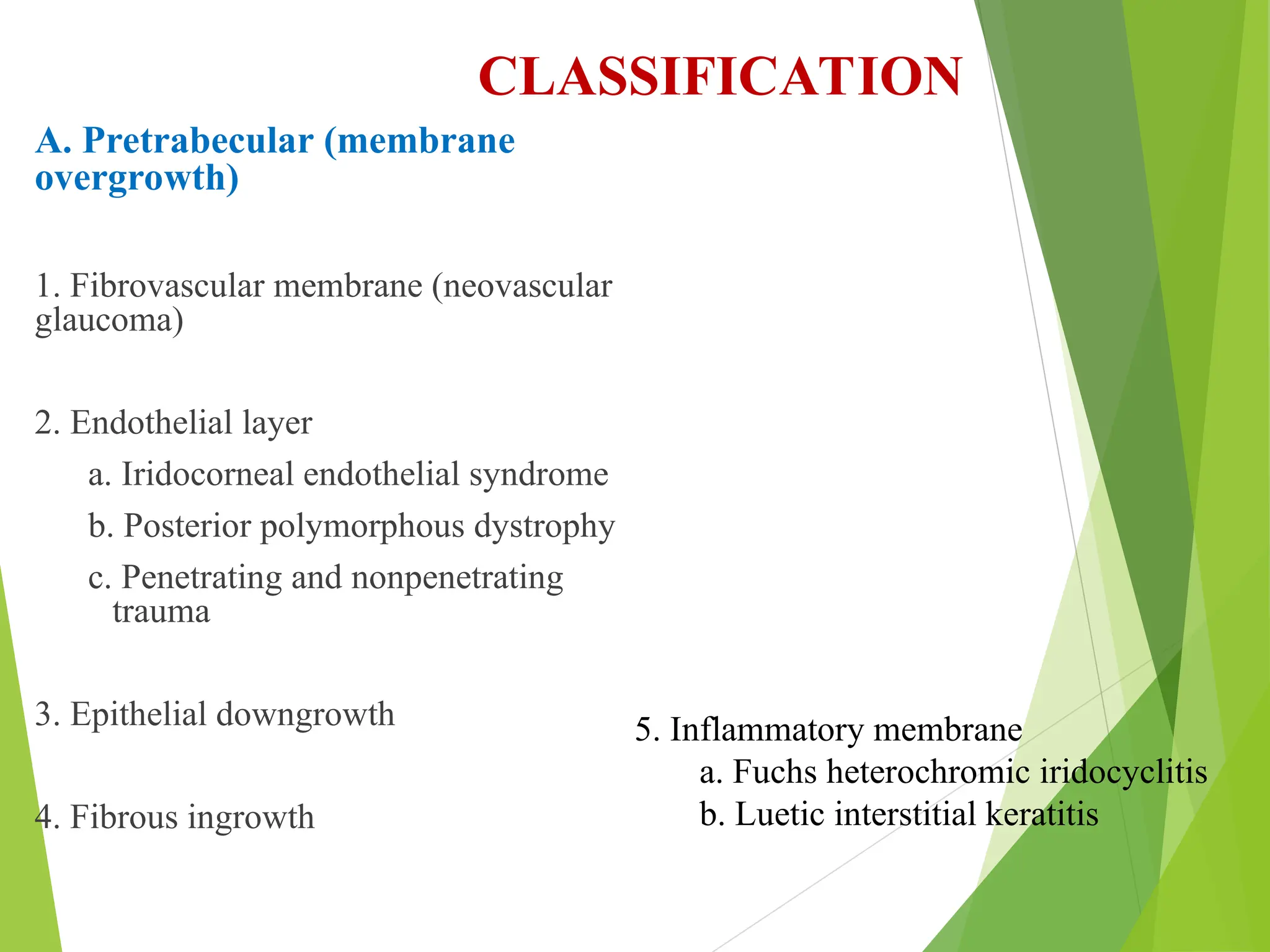
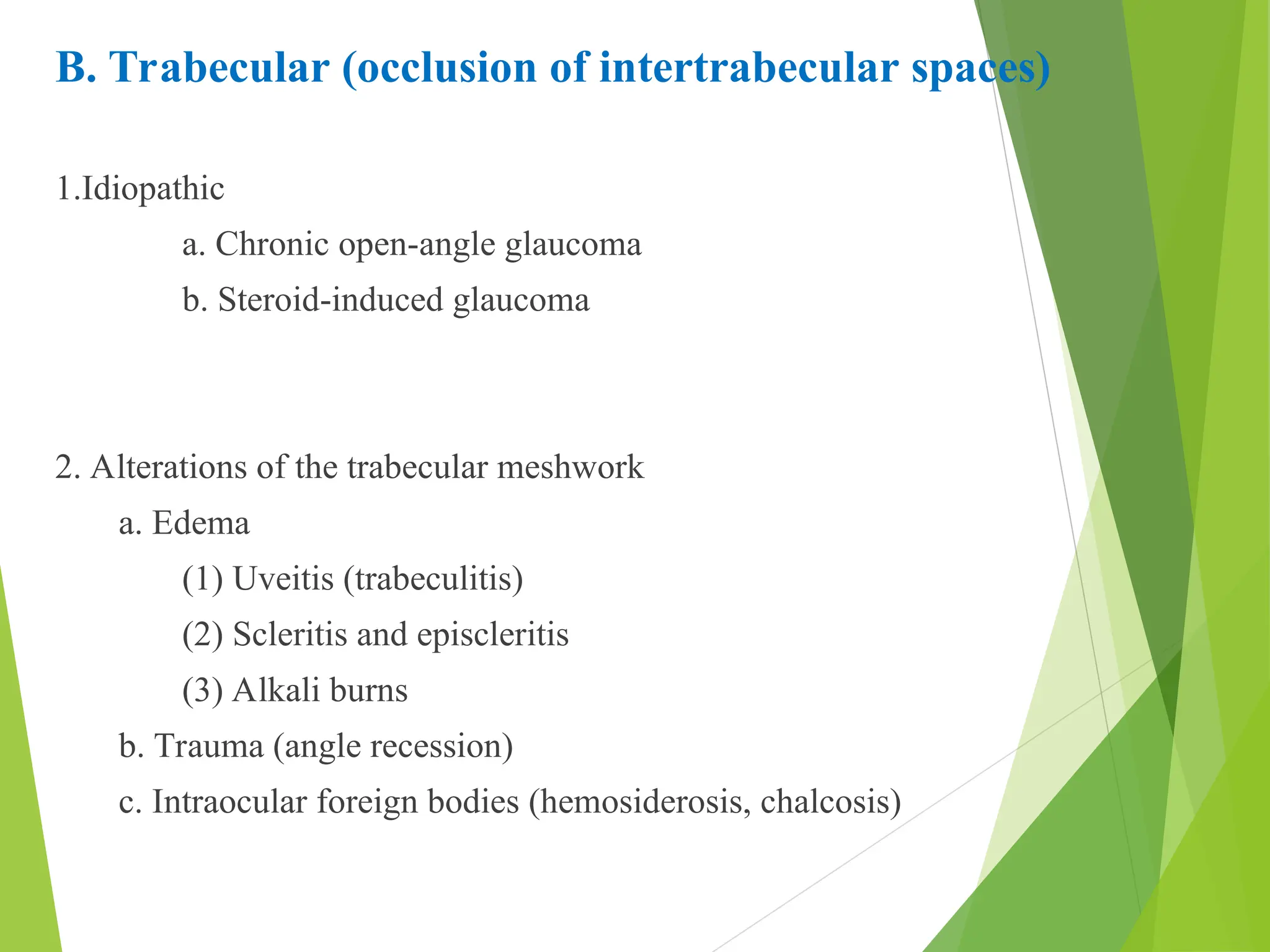
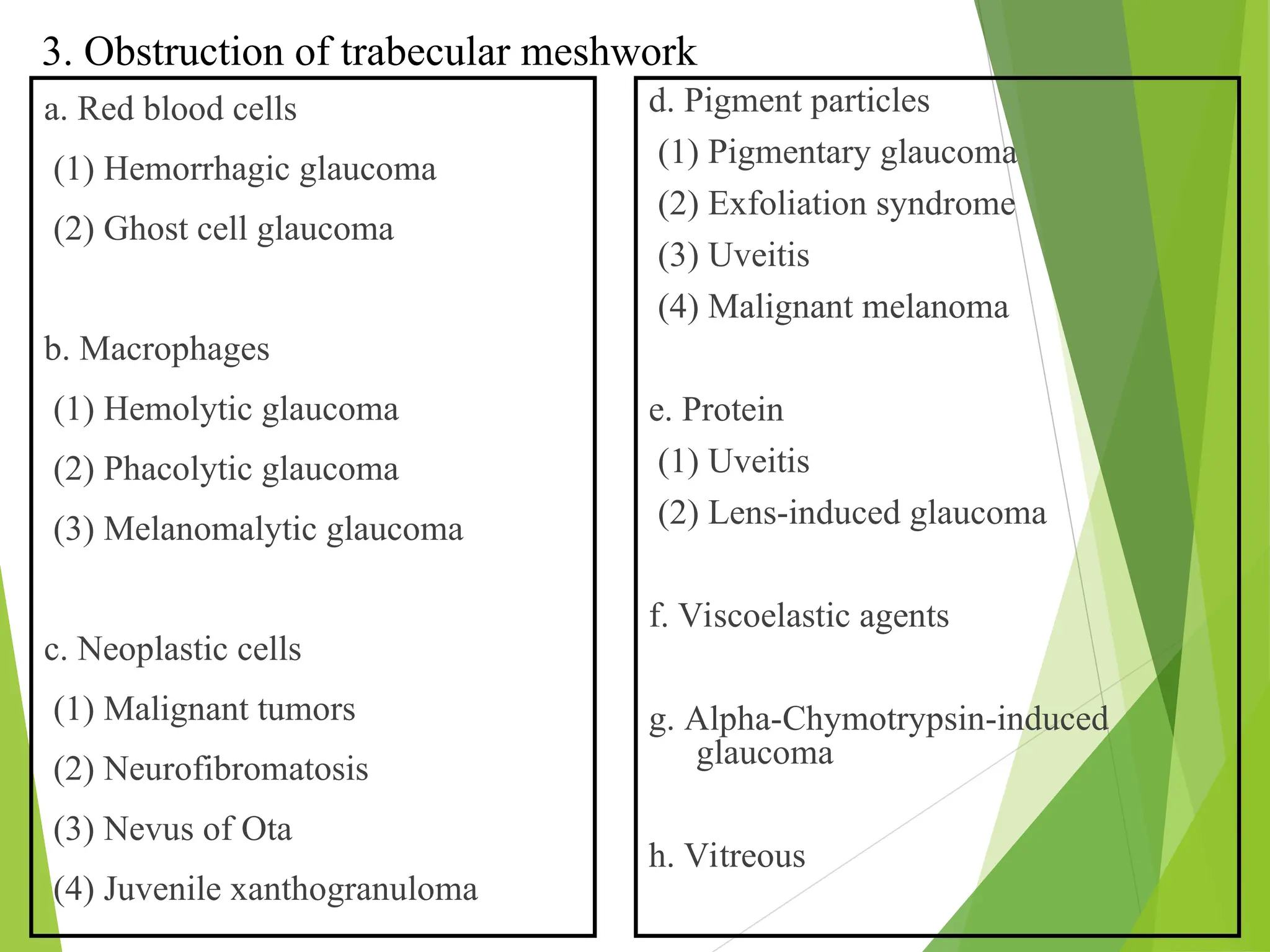
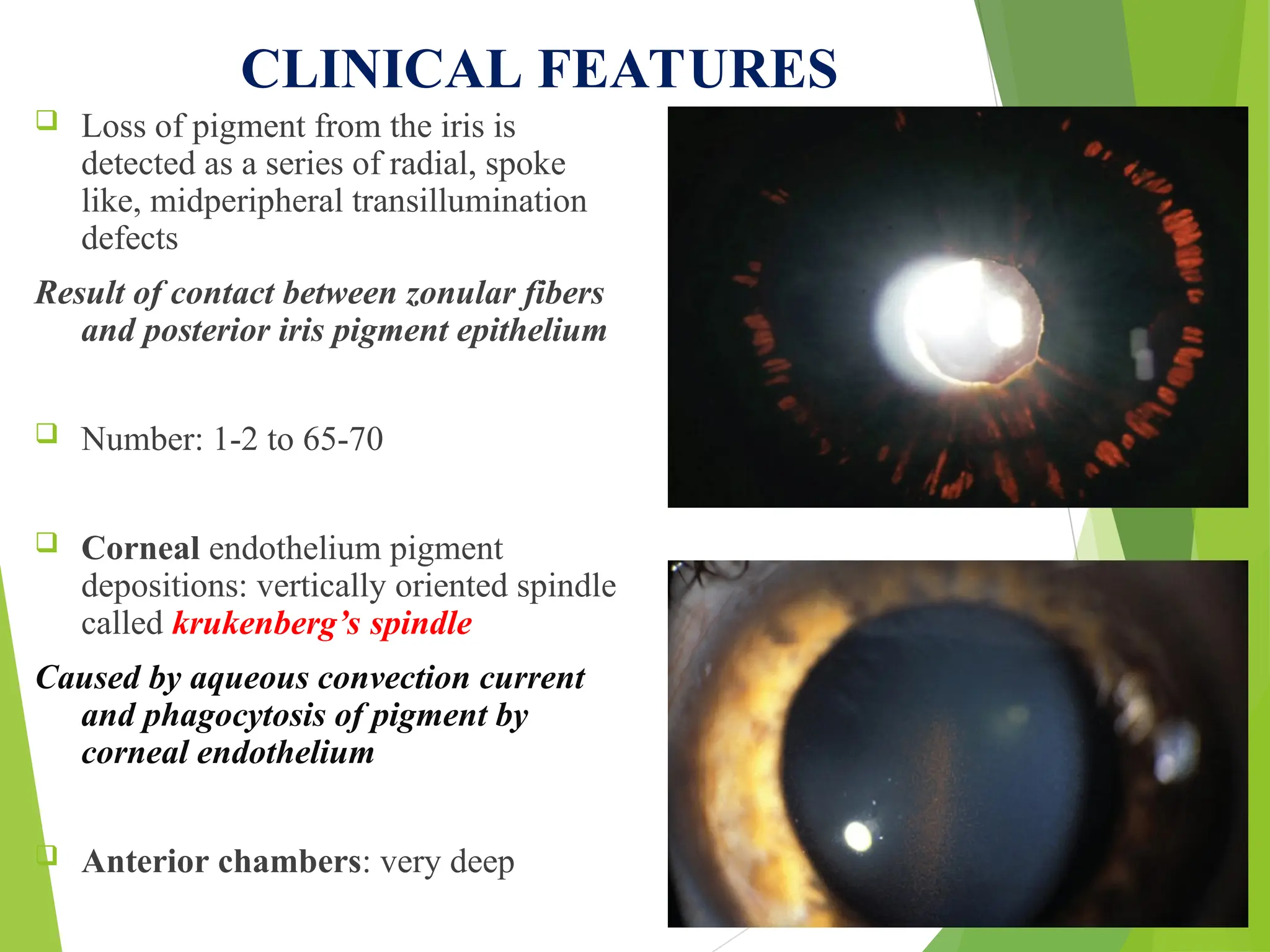
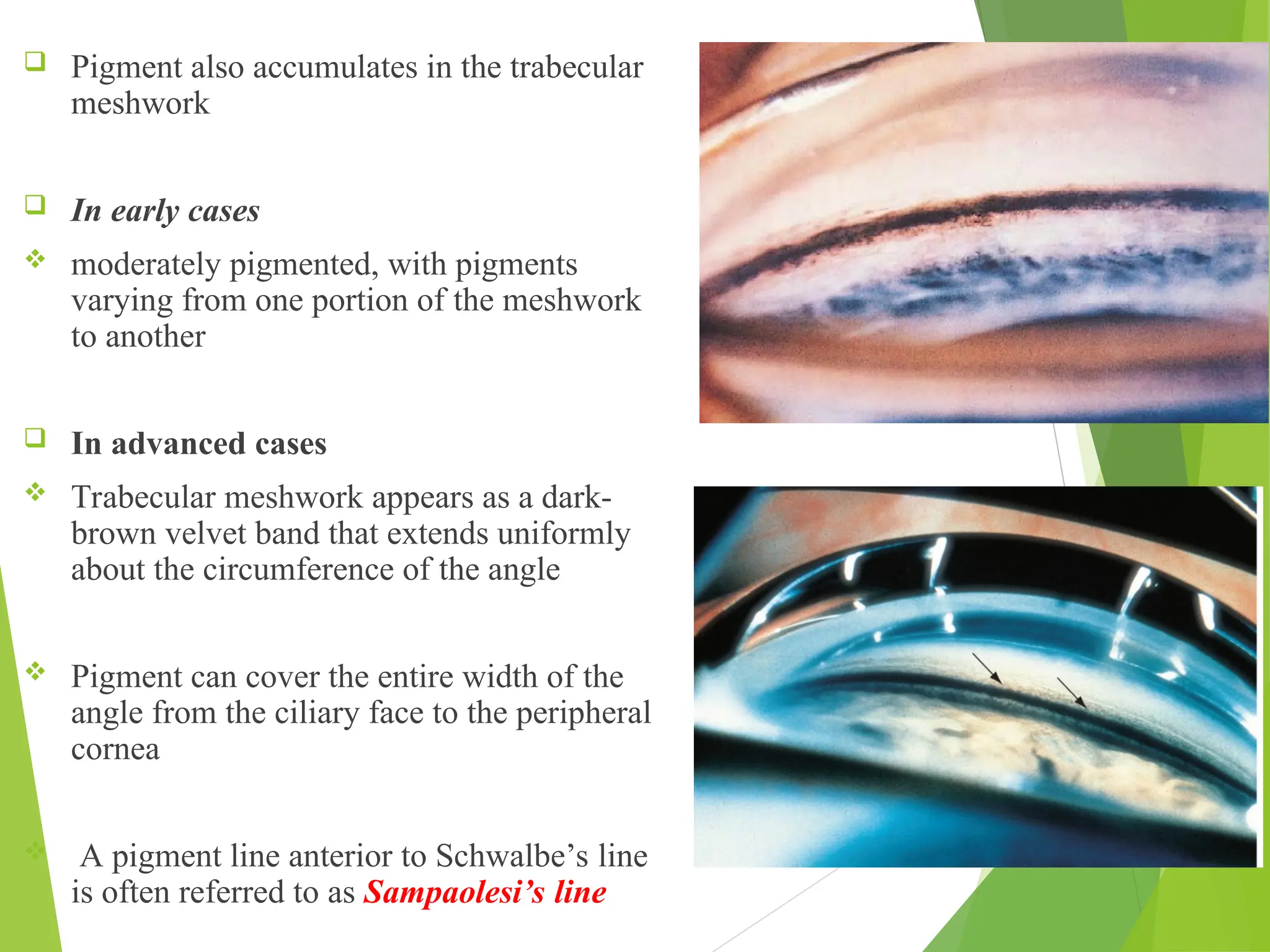
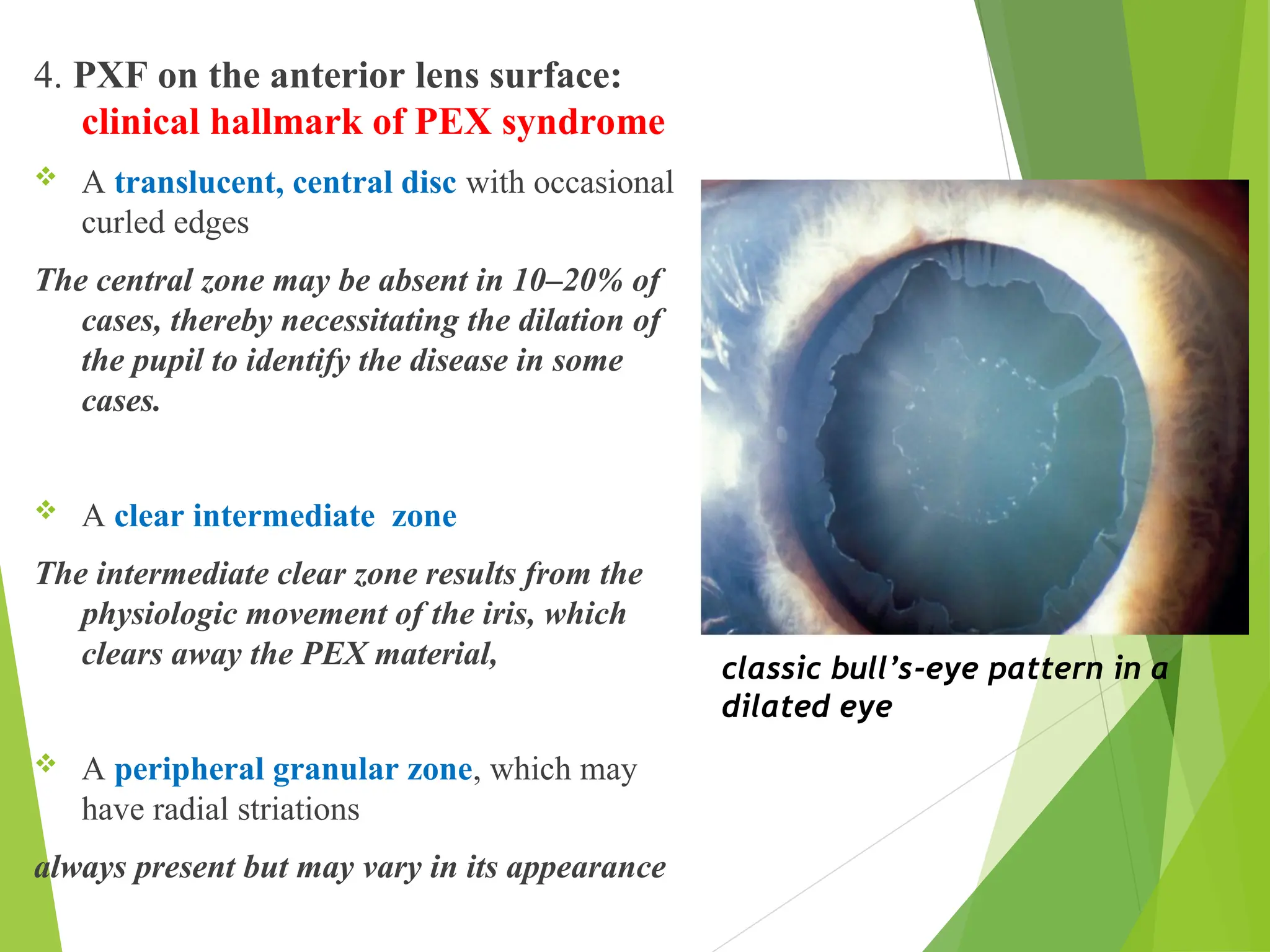
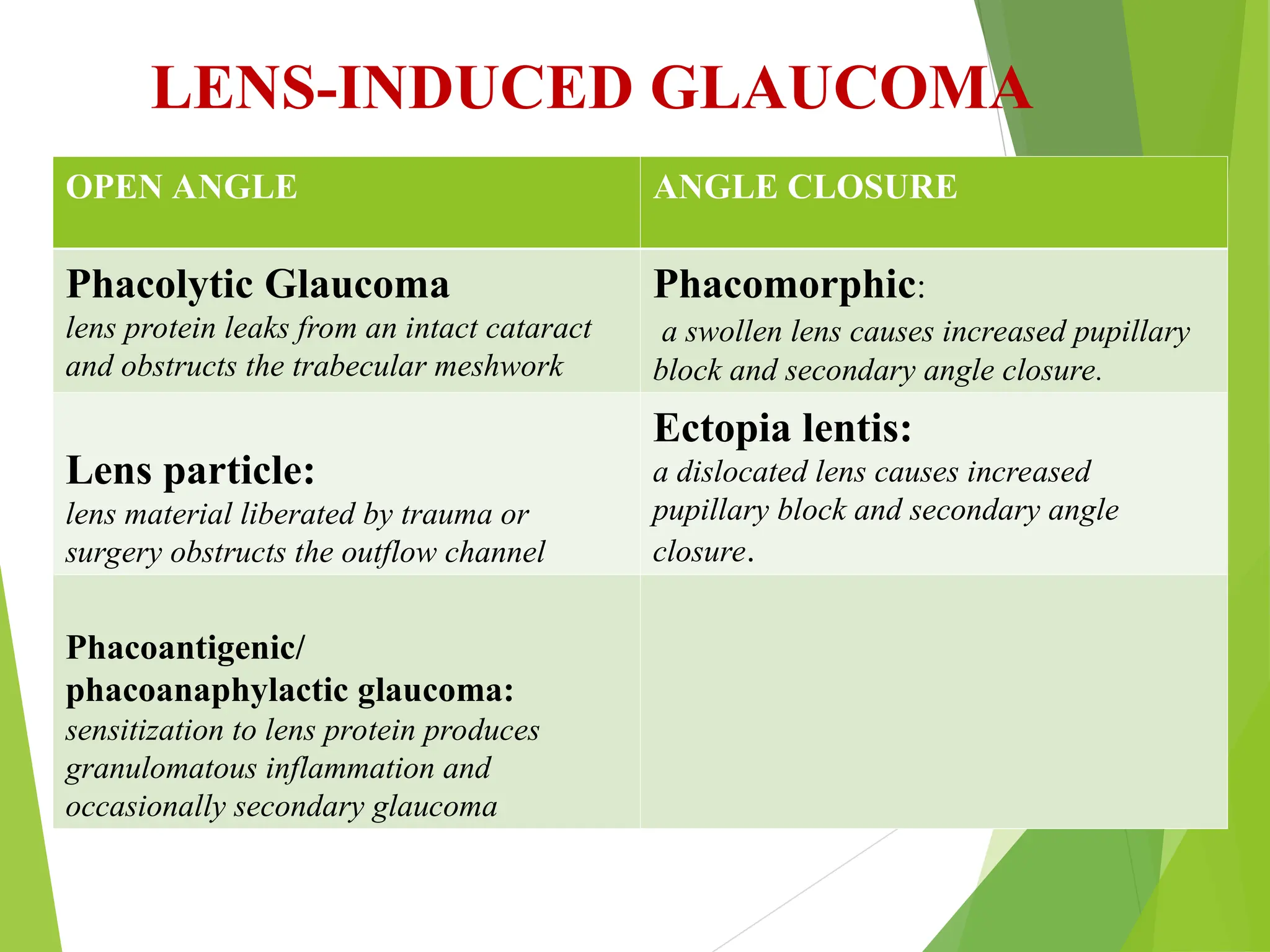
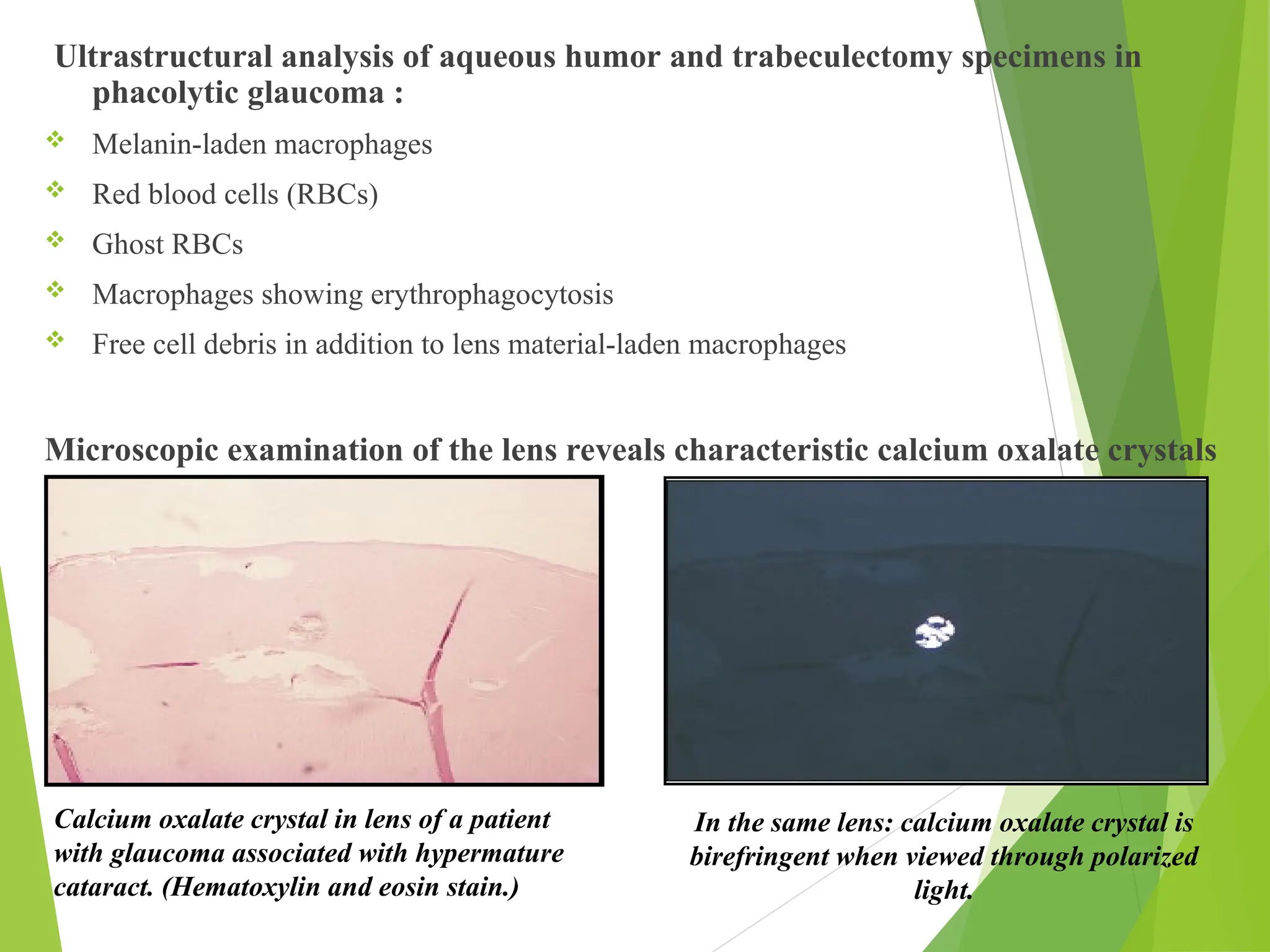
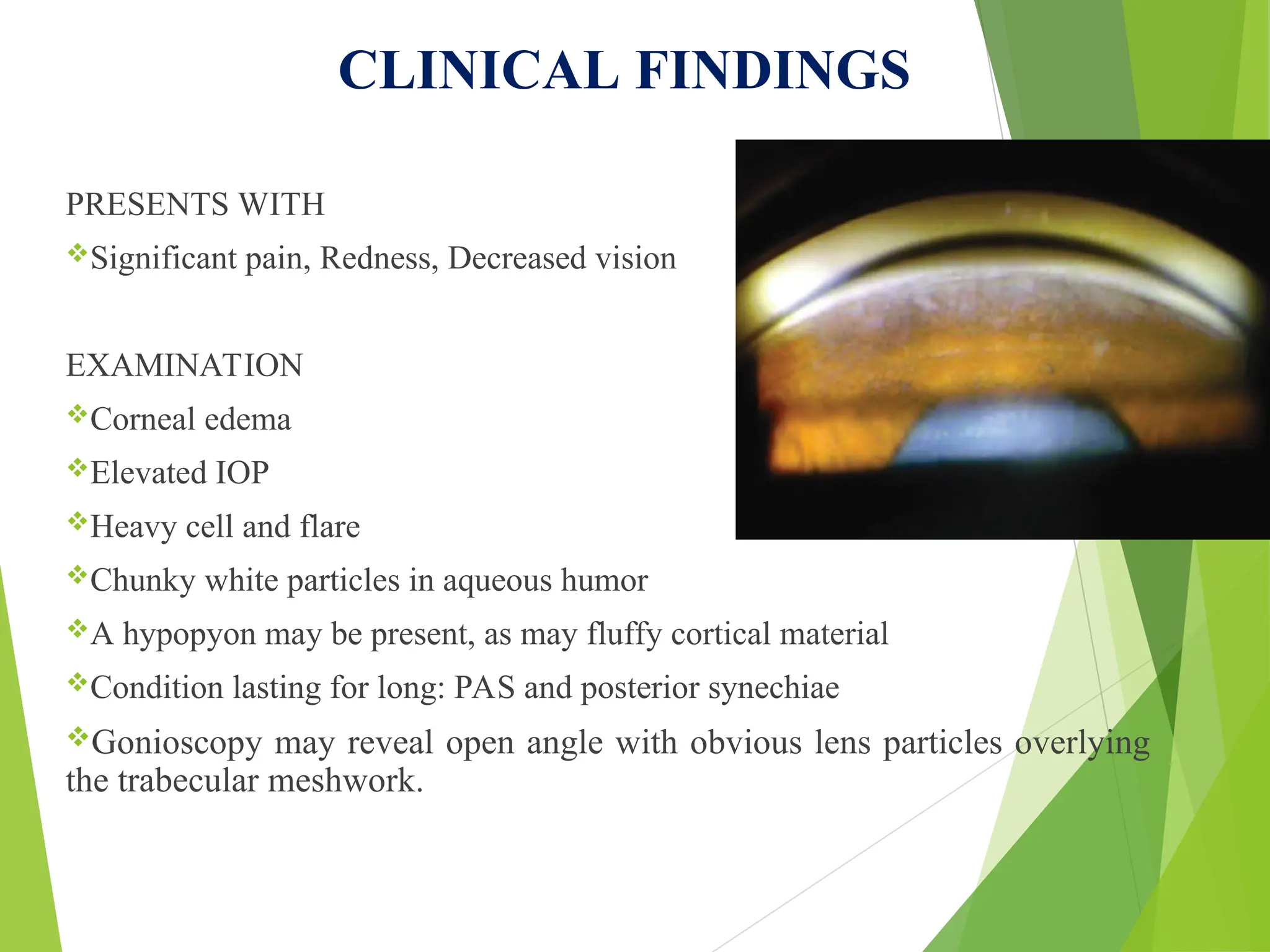
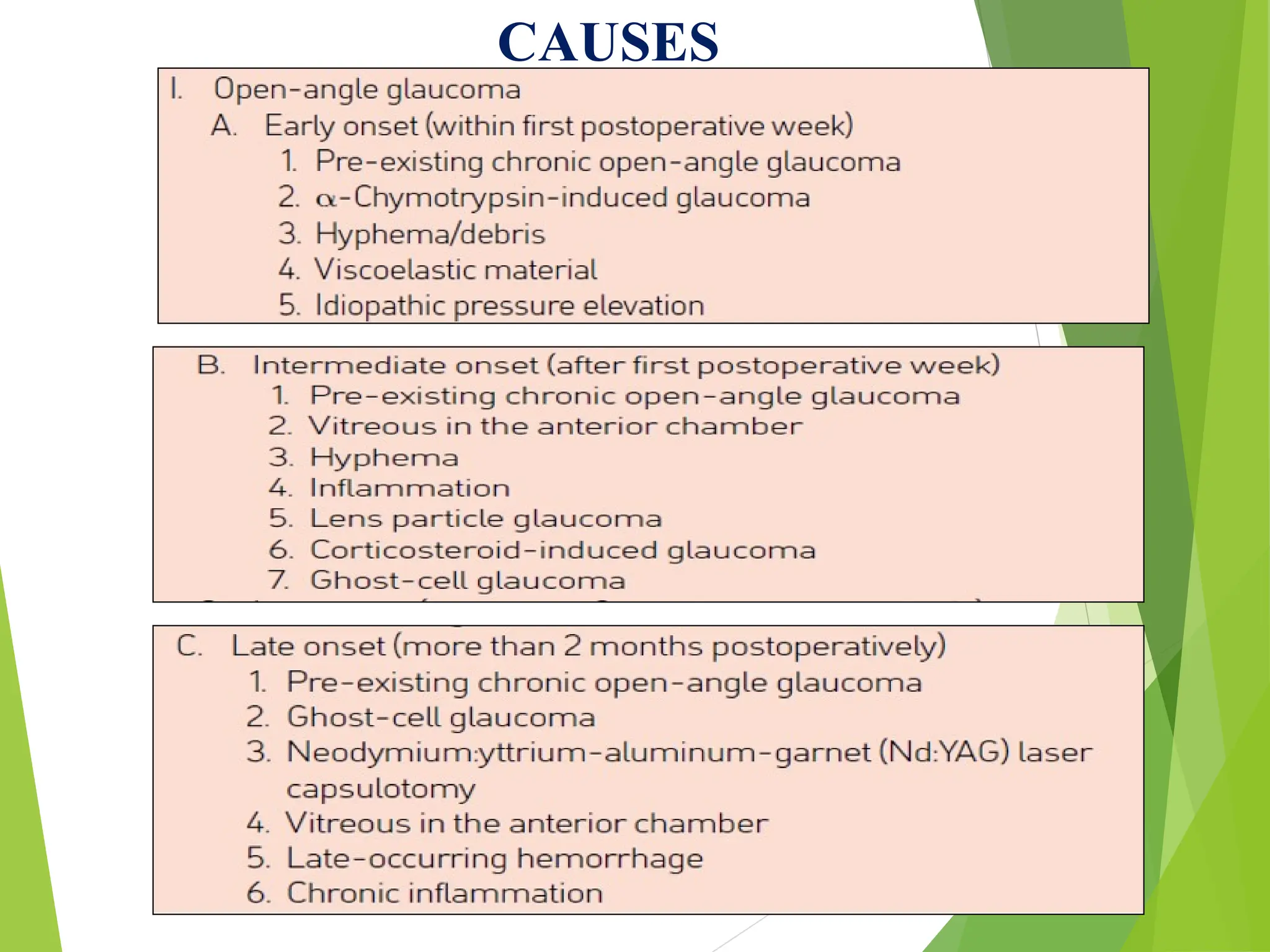
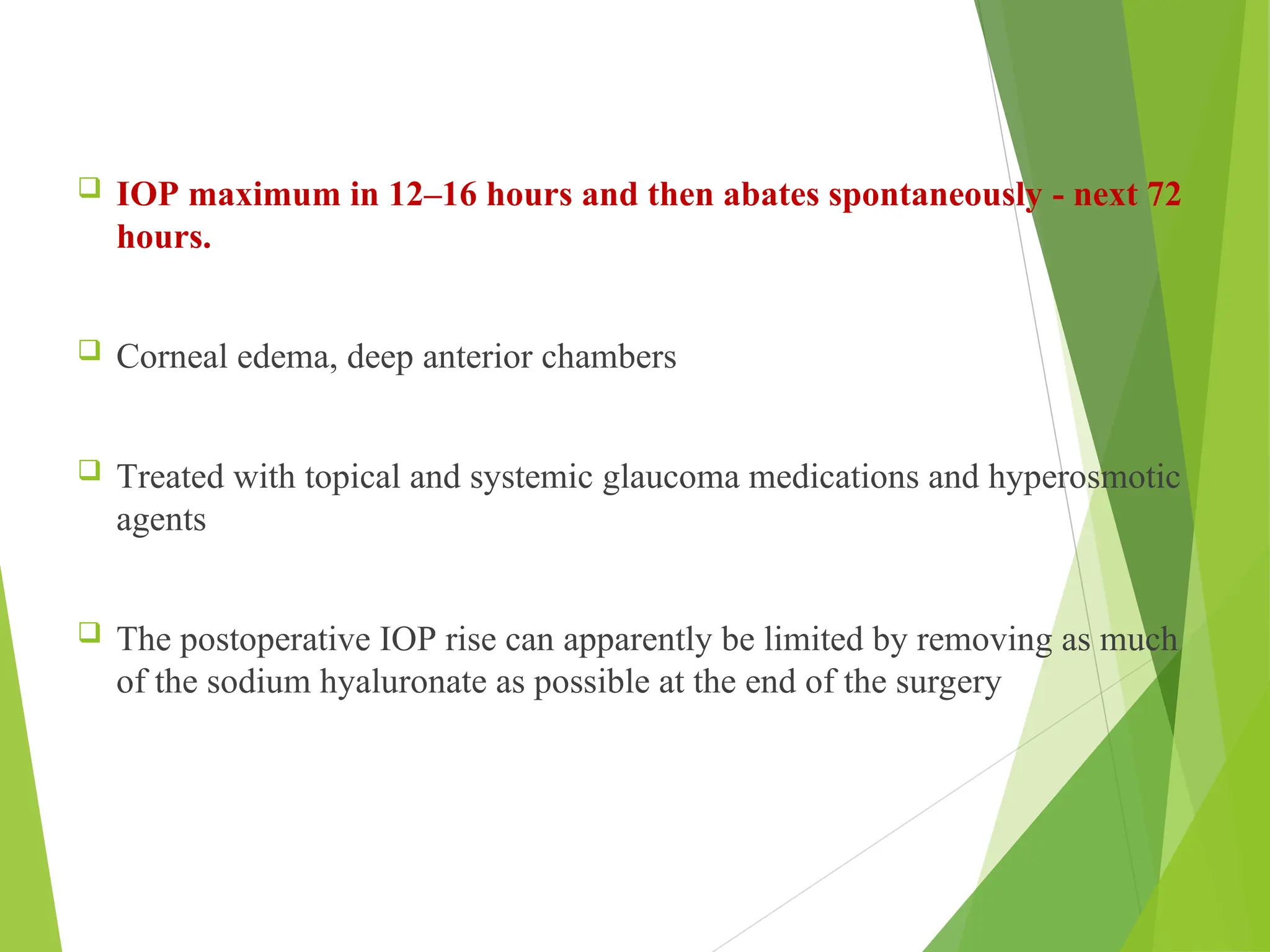
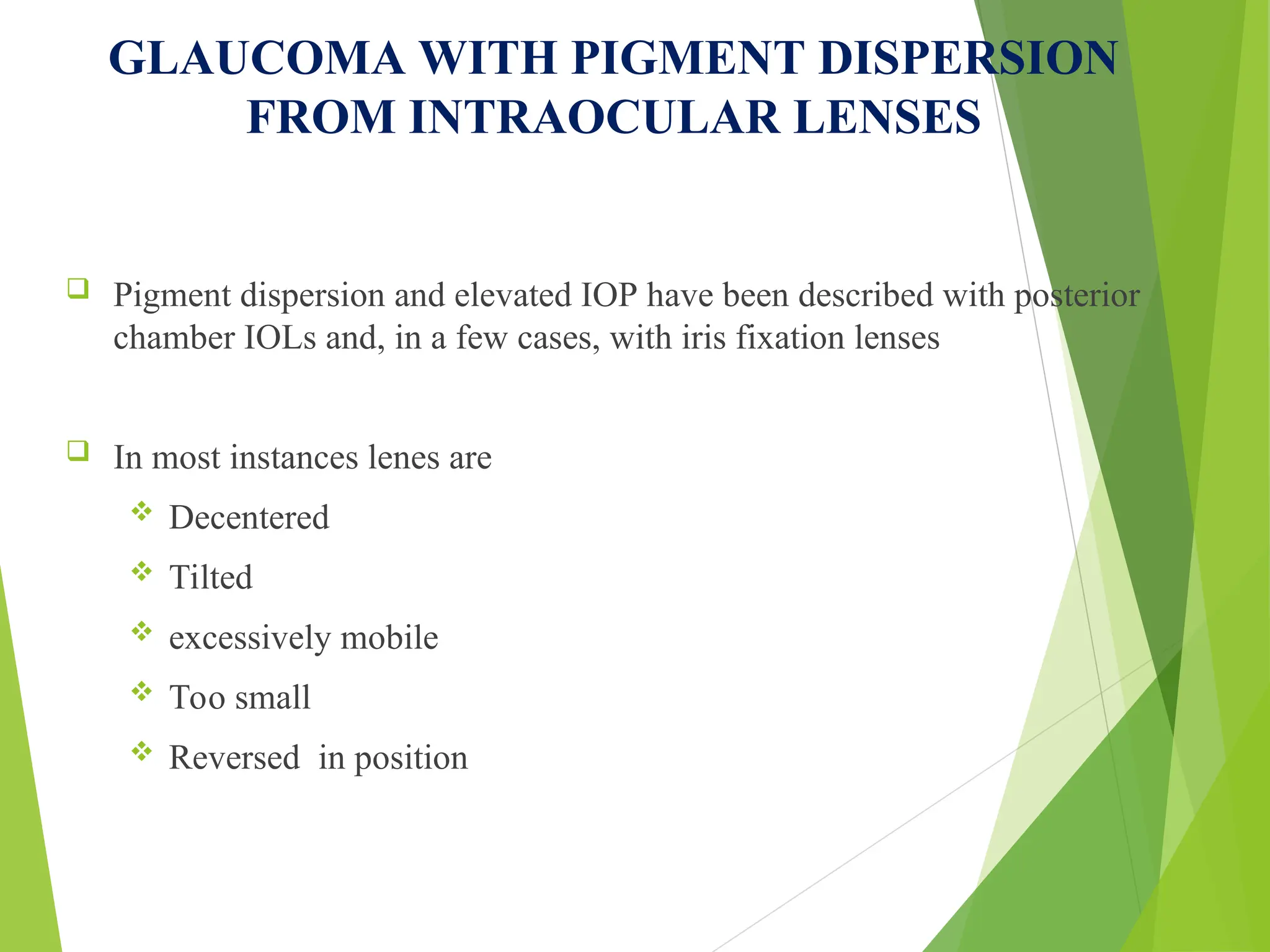
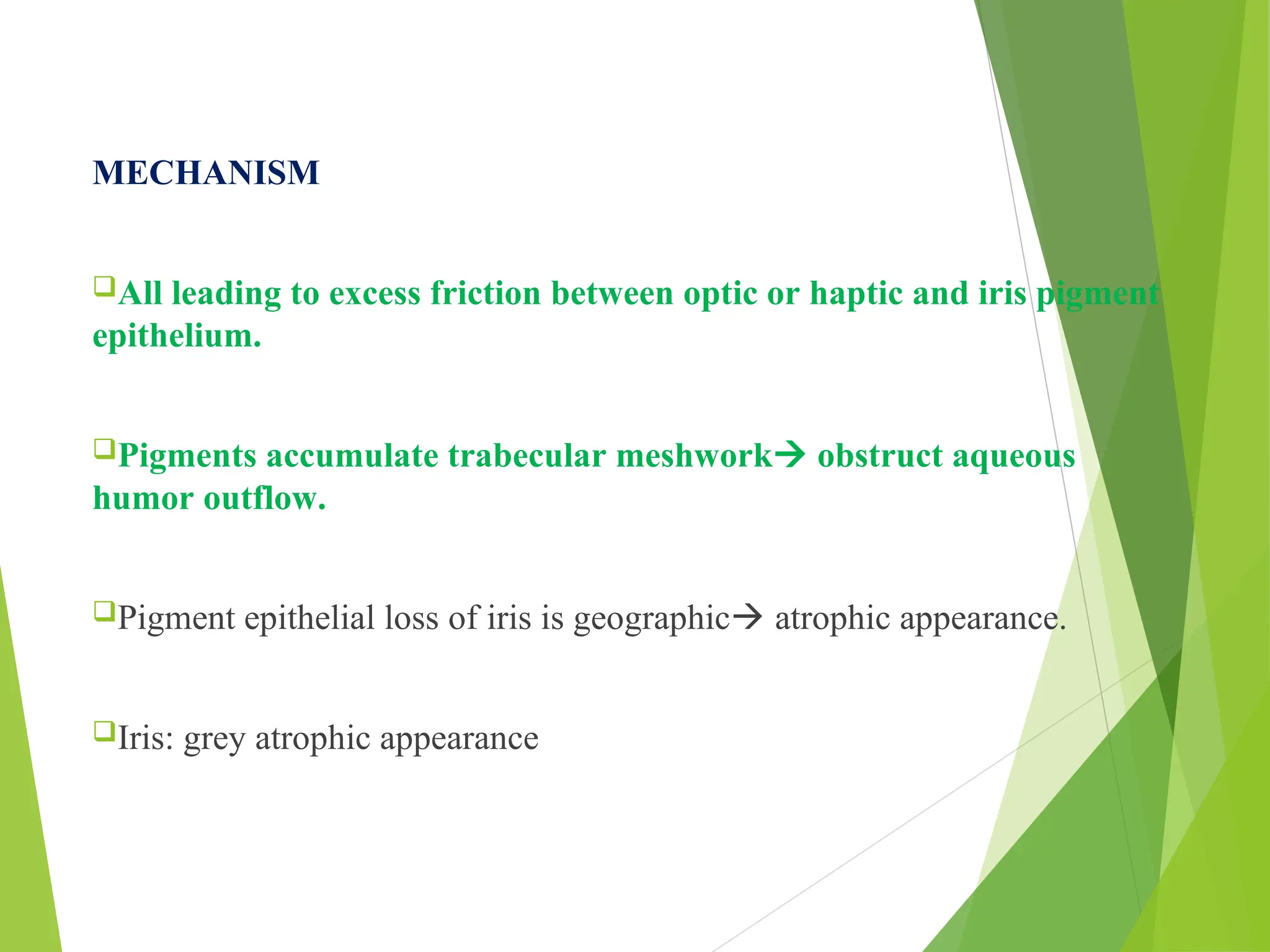
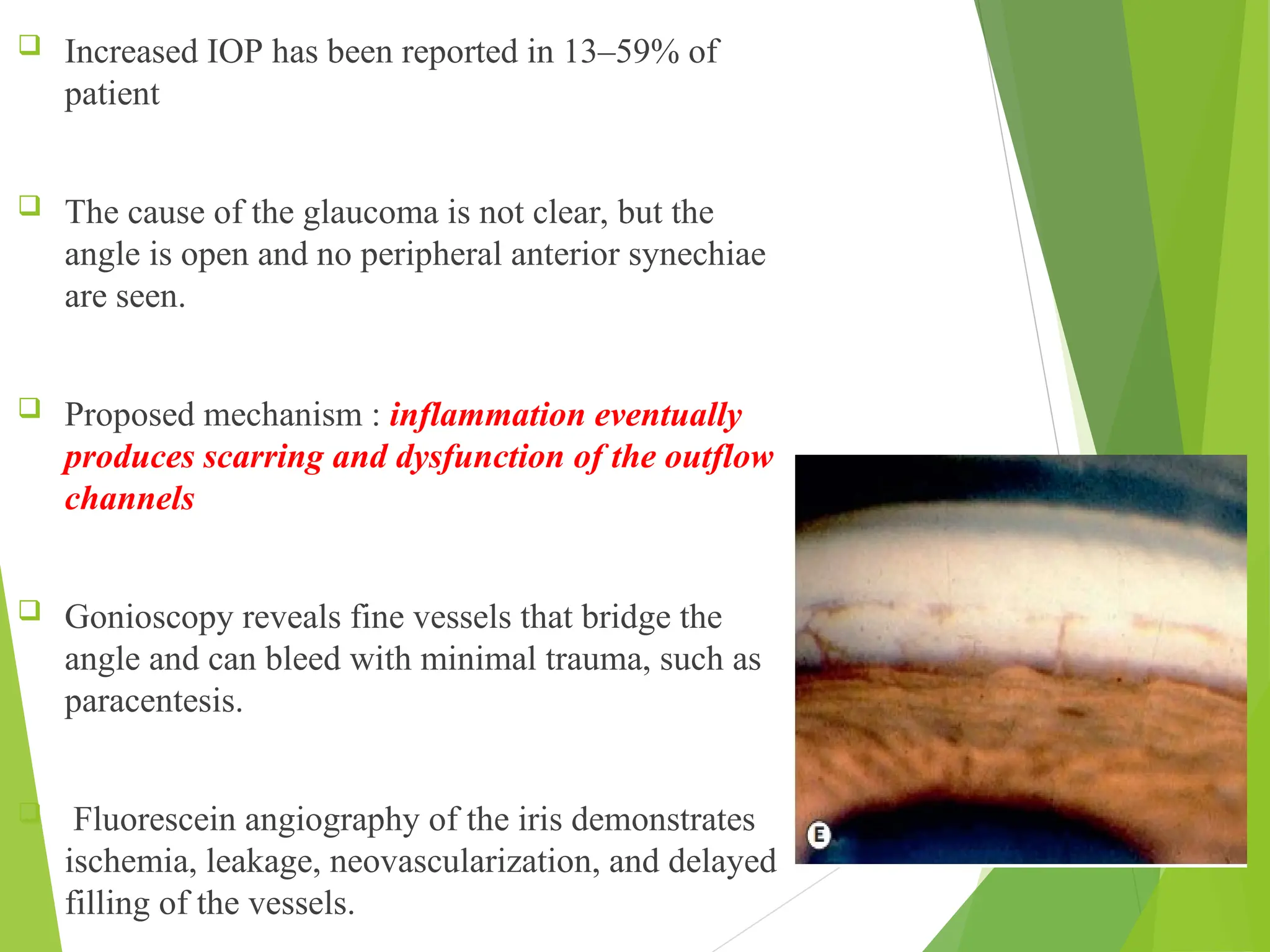
The document discusses secondary open angle glaucoma, detailing its classification, epidemiology, and pathogenesis. It highlights various causes, including pigment dispersion syndrome and pseudoexfoliation syndrome, along with their clinical features and differential diagnoses. Treatment options and the associations of glaucoma with ocular and systemic conditions are also covered.